A Review of Myotatic Reflexes and the Development of Motor
advertisement

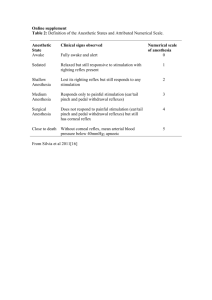
A Review of Myotatic Reflexes and the Development of Motor Control and Gait in Infants and Children: A Special Communication Although the mechanism of the phasic myotatic (or '?@etch'>reflex is well-known, the role of this re@ in adult gait remains speculative. The acquisition and development of locomotor skills with respect to the development of the myotatic reflex requirefurther study in both healthy and neurologically impaired children. In this article, the well-documentedpropenies of the healthy adultk myotatic reflex are compared with recentwings of the myotatic reflex in healtby infants and children and contrasted with reflex propertl'es in patients with cerebralpalsy. These data allow us to begin to characterize the emergingfeatures of the stretch reflex in normal andpathological early development. From these data, we can begin to speculate about the relationship between changes in stretch reflexes and the acquisition of skillful movement and gait in early childhood [Mykkbust BM: A revlevleu of myotatk reflexes and the development of motor control and gait in infants and children:A special communication. Phys 7;6er 70:188-203, 1990] Barbara M Myklebust Key Words: Gait;Motor activity;Muscle pe@ormance, general; Pediam'cs, development. The age at which children start to walk independently is quite variable,' and there is considerable debate about how children learn to walk.2 Studies of' children by Diet23 and Berger et a14 suggest developmental differences of the myotatic reflex in gait between very young children (1-2 years of age) and older children (G 10 years of age). The acquisition and development of locomotor skills with respect to the development of the myotatic reflex requires further study in both healthy and neurologically impaired children. Abnormal myotatic or "stretch" reflexes (evoked by tendon tap) have been described in nonambulatory children and adults with spastic cerebral palsy (CP).5 The hypothesis that the hyperactive stretch reflex is related to the inability to walk in these patients remains to be tested.~atafrom ambulatory adults with spasticity suggest that hyperactive stretch reflexes may interfere with gaits and the performance of smooth voluntary limb movements.7 B Myklebus~:,PhD, is Assistant Professor of Neurology and of Physical Medicine and Rehabilitation, Medical College of Wisconsin, and Research Health Scientist, Laboratory of Sensory-Motor Performance, Clernent J Zablocki Veterans Administration Medical Center, Research Services 151, Milwaukee, W1 53295 (USA). This work has been supported by research Funds from the VA Rehabilitation Research and Development, the Foundation for Physical Therapy Inc, the United Cerebral Palsy Foundation, and National Institutes of Health Grant AM 33189 to Gerald L Gottlieb, PhD. This solicited ariicle was submitted Februcuy 1, 1989; was with the authorfor ra~isionfor file weeks; and was accepted October 25, 1989. Physical TherapyNolume 70, Number YMarch 1990 'The phasic myotatic reflex, evaluated by tendon tap, is a standard element of the clinical examination used to characterize neurological abnormalities. Although the mechanism of the myotatic reflex is wellknown, the utility of this reflex response in identifying deficits of posture and movement remains elusive. Although the role of the stretch reflex in adult gait remains speculative and has not been specifically addressed in classical texts such as that of Inman et al,R recent studies suggest that primary afferent reflex pathways may play a role in walking, running, and error correction in gait.Sl3 In this special communication, the well-documented properties of the healthy adult's myotatic reflex are compared with recent findings of the myotatic reflex in healthy infants and children and contrasted with 188/51 reflex properties in patients with CP! These data allow us to begin to characterize the emerging features of the stretch reflex in normal and pathological early development. From these data, we can begin to speculate about the relationship between changes in stretch reflexes and the acquisition of skillful movement and gait in early childhood. Motor control deficits in patients with spasticity are presented to illustrate the possible relationship between abnormal myotatic reflexes and impaired voluntary movement. A H-Reflex 1.5 m v Y-B Tendon Tap 0.75 mV : -.J,,pSOL. - Y Ct Myotatic Reflexes and Postmyotatic and Voluntary Responses 20 mmc C During the last 15 years, the nomenclature has evolved for identifying muscle electromyographic activity that is evoked reflexively and voluntary contraction. Electromyographic waveforms have been named according to onset latency! For purposes of simplicity, the myotatic refex (or spinal stretch reflex) is defined as having onset latencies of about 25 to 45 msec, depending on the distance of the stretched muscle from the spinal cord and the type of perturbation (ie, tendon tap or mechanical stretch of the muscle). The amplitude of the myotatic reflex has little dependence on prior instruction to the subject and great dependence on prior contraction.l5 Voluntary responses occur after about 100 to 120 msec in adults. The amplitude and latency of voluntary responses are dependent on prior instruction to the subject and less dependent on prior contraction of the agonist muscle. Electromyographic activity evoked in the intermediate interval is called postmyotatic responses. Postmyotatic I I I I Mechanical Ankle Rotation 2.01 -mvl 0 e y & A 50 msec Fig. 1. Soleus (SOL) and tibialis anterior (TA) muscle electromyogt-aphicresponses in one health adult subject for (A) a single H-reflex responsefollowing electrical stimulation of the tibial nerve, (B) a single Achilles tendon tap, and (C) an average of 10 responses to a rapid mechanical dmiflmon of the ankle joint of 17 degrees. Electrom-yographicactivity is recordedfrom sutface electrodes. For rapid ankle dorszJIexion, sutface EMG signals were full-wave rectijied In each diagram, onset of the reflex 13 identtfid with an arrow: m e II-reflex onset is at approximately 32 msec, the tendon jerk reflex onset is at approximately 38 msec, and the stretch reflex onset in response to mechanicalperturbation of the ankle joint is at approximate[v 48 msec. responses are moderately affected by prior instruction and may be modified by prior agonist contraction. 'Studies performed at the Motor Coordination Laboratory and the Laboratory of Motor Reflex Development, Rush Medical Center, Chicago, IL, and the Laboratory of Sensory-Motor Performance, Clement J Zablocki VA Medical Center, Milwaukee, W, have been approved by the human studies research review committees. Informed written consent has been provided for all research studies. +Tattonand Lee use the terms "MI,""M2,""M3,"and "voluntary response" to define these EMG signals.14 The MI waveform is the myotatic reflex at 25 to 45 msec. The M2 response begins after 50 msec and peaks before 80 msec, and is followed by (and sometimes commingled with) the M3 response, or "long-latency"or "long-loop" response, which begins near 85 msec and peaks before 100 msec. Activity after 100 msec is considered "voluntary." 52 / 189 M TA Myotatlc Reflexes In Healthy Adults In the healthy adult, stretch of the soleus (SOL) muscle evokes a synchronous burst of EMG activity in the stretched (agonist) muscle at monosynaptic latencies (about 40 msec), and relative electrical silence is observed in the antagonist tibialis anterior (TA) muscle (Figs. 1,2).5 Myotatic (or "stretch") reflexes in the normal, relaxed TA muscle have an extremely high threshold, resulting in delayed or absent responses when the TA tendon is tapped.5.16 The normal Physical TherapyNolume 70, Number 3/March 1990 limb length (which increase the onset laten~y).~3 &A HEALTHY ADULT subject, the latency of the stretch reflex is shortest (approximately 35-40 msec) for the H-reflex and longest for mechanical dorsiflexion of the ankle (approximately 45-50 msec). Rapid mechanical rotation of the ankle joint causes a stretch of the SOL muscle when a torque motor is used to deliver torque pulses of 1 second's duration to dorsiflex the ankle. The ankle is rotated from the neutral position to approximately 10 degrees of dorsiflexion over the period of 50 to 100 msec, and the dorsiflexed position is maintained for 1 second; then, the ankle joint is returned to the neutral position before the next stimulus is applied. The stretch-reflex onset latency, measured from the onset of the applied torque to the onset of the EMG activity, is extremely stable at about 45 msec, and it varies about + 10 msec among different subjects.16 This onset latency is approximately 5 to 10 msec longer than the reflex evoked by tendon tap. Unlike the tendon-tap stimulus (which lasts about 5 msec), the mechanical dorsiflexion of the ankle is extended over a 50- to 100-msec period, and the SOL muscle's EMG response begins and ends while the muscle is still lengthening. The short-latency reflex response is more likely the result of the large initial transient stimulus of the ramp stretch (a change in muscle length), rather than the change in velocity, which is monitored by the muscle spindles. The SOL muscle's stretch reflex is essentially unchanged by body orientation (sitting, supine, or prone p ~ s i t i o n ) .However, ~ ~ ! ~ ~ suprasegmental control (including voluntary contraction of the SOL muscle) influences and modifies the amplitude of the H-reflex. The onset latency of the monosynaptic reflex increases with limb length in the adult subject. Changes in the reflex latency in early childhood development are attributable to central and peripheral myelinization (which increases conduction time and consequently shortens the onset latency) and to increases in Differences in reflex onset latencies between the H-reflex and Achilles tendon tap are attributable to the different stimulation sites; that is, the H-reflex directly stimulates the tibial nerve at the posterior aspect of the knee, and the tendon tap excites muscle spindles of the SOL muscle. The electrical stimulation of the H-reflex (1.5 msec duration) is a precisely controlled stimulus; this stimulus is unlike the tendon tap (approximately 5 msec duration), which may excite muscle spindles differently, depending on the angle, force, and exact location on the tendon that is tapped. 4- +40msec [ 50 0.5 mV 0.5 mV k&& &,A- BIRTH-ONSET C N S INJURY 0.5 mV [ 30 ADULT-ONSET CNS INJURY [ 40 2.0 mv 2.0mv Joint Angle SOL EMG TA EMG Fig. 2. Repex responses in soleus (SOL) and tibialis anterior (TA) muscles to sudden ankle d m @ m ' o n .Electromyographic raponses werefull-wave rectij7ed and filtered. Top diagrams show respoms of a healthy, r e k e d adult subject. Middle di6gram.s show resjmmes cda loyear-old child with spastic cerebral palsy. Bottom diagrams show data from a spznul cord injured adult patient three months after injury. Each horizontal record is the average of 10 respomes. Three dwerent torque levek were used, with Stronger stimuli plotted toward the background. Time markers are at 50-msec intervals. The dtferences in SOL muscle response latencies between the top and middle diagrams are due to dtferences in age and size of the subjects. (CNS = central nervous system.) (Adaptedfiom Myklebust et al.5) SOL muscle's stretch reflex is produced by activation of the SOL muscle's motoneurons through monosynaptic (and oligosynaptic) spinal cord path~ays.17~1"his agonist muscle activation is accompanied by an inhibition of the antagonist muscle through a disynaptic pathway. This is the classically described pathway of reciprocal inhibition (Fig. 3). The myotatic reflex loc~pconsists of the muscle spindles, fast-conducting Ia aEerent fibers, and agonist alpha motor fibers. Activation of the myotatic reflex of the SOL muscle may be achieved by rapid dorsiflexion of the ankle16 or by a tap to the Achilles tendon.19 The monosynaptic (or oligosynaptic) spinal reflex path may also be activated by electrical stimulation of the tibial nerve (Hoffmann reflex or "H-reflex.")*(Fig. l).zOIn a single *Unfortunately, the H-reflex has been referred to as a "late response" in electroneuromyopathy. With respecr to onset latencies of nerve conduction studies of the tibial nerve and other peripheral nerves, the H-reflex is "late." Physical TherapyNolume 70, Number 3/March 1990 Differences in amplitude of stretch reflex responses may be attributable to the fact that muscle spindles are 'more sensitive to the velocity of stretch than to changes in muscle length. That is, the monosynaptic reflex may be most effectively evoked by the brief stimulus of the tendon tap (stimulus duration of 55 msec) than by mechanical rotation of the ankle (stimulus duration of 50-100 msec). Furthermore, to an extent, larger-amplitude tendon taps and larger angular rotations of the ankle tend to produce larger-amplitude reflex EMG responses than smaller stimuli. In the "H-reflex recruitment curve," the changes in the amplitude of the SOL muscle's EMG response are plotted with respect to the stimulus amplitude. At low levels of electrical stimulation, Ia afferent fibers from SOL muscle spindles are excited. About 30 msec after the stimulus, a synchronized EMG burst, the "Hwave," is recorded from the SOL muscle. As the amplitude of stimulation is increased, the H-wave increases until the threshold of the SOL muscle's motor fibers in the tibia1 nerve is reached. About 8 msec after the stimulus, an EMG burst called the "Mwave" occurs as a direct motor response to the stimulation. Further increase in the stimulus amplitude results in a monotonic increase in the M-wave until the full recruitment of all motor units is achieved. At this stimulus level, the H-wave increases only slightly and then decreases. When the M-wave is maximal, the Hwave has vanished. Typical responses to progressively stronger stimuli (from threshold H-reflex to maximal M-response) are shown in Figure 4. This behavior results because largeamplitude electrical current stimulates both efferent fibers and Ia afferent fibers; the Ia afferent nerve fibers conduct the reflex wave faster than the antidromic signal is conducted in the alpha motoneuron fibers. Therefore, at strong stimulus amplitudes, the Hwave is blocked by a collision of the antidromic impulses and the reflexelicited orthodromic impulses in the alpha motoneuron fiber.2" The H-reflex recruitment curve is characterized by the threshold of electrical stimulation amplitude to elicit - Inhibitory Synapses Fig. 3. Spinal cord circuity depicting normal stretch reflexpathwa-y (paths 3 and 4) and bypothetical "wiring"underlying pathological sh-etch reflexes d i b i t e d in p a t h t s with cerebral paLy (CP) and in healthy neonates (paths 1 and 2). The healthy adultk reqonse to sh-etch is the result of$ring fa affmentfifibers,which are excitatory on the agonist alpha motor fiber (path 4) and simultaneously inhibitoty on the antagonist alpha motorfiber through an interneuron (path -3). It is qeculated that in patients with CP and in newborn infants, sh-etch is simultaneous!yfacilitoty on the stretched muscle and its antagonist (ty m o n q m p t i c or polysynaptic pathways) (path I). This 'keciprocally excitatory connection" may be normally present at birth and then i s gradually masked or dies during normal development. In patients with CP, the pathway of recqrocal excitation may persM (ie,fail to be masked or to die) or it may develop gradua l [ ~This . pathway may be present, but tonically inhibited, in the healthy adult. Path 2 supposes the absence of the normal tonic inhibition as a developmental defect in patients with CP and as a pathway that is not yet complete in the neonate. (Adapted from Myklebust et a15 and from Myklebust.23) the reflex contraction of the muscle, by the maximum H-reflex amplitude (H,,), and by the extinction of the H-reflex when stimuli of increased intensity produce occlusion between antidromic and orthodromic impulses in the same alpha motoneurons. Mresponse recruitment curves are used with H-reflex recruitment curves to ensure that technical conditions for stimulation and recording remain constant.21 The H-reflex has a lower threshold than the M-response and an H,, that is half that of the maximum Mresponse (M,,,). In adults, the Hma.JMmaxratio, or WM ratio, is 0.54 + 0.10.25 The H/M ratio is 0.65 + 1.00 at birth; it decreases to 0.40 + 0.13 at age 1 year and then slightly increases to age 3 years, when values similar to those of the healthy adult are reached. Use of the WM ratio, rather than the absolute amplitude of the H-reflex, tends to minimize errors attributable to individual differences in test conditions. If the H-reflex is elicited by paired stimuli, the amplitude of the reflex varies according to the interval between the stimuli.2Whe "H-reflex recovery curve" is used to identlfy the period during which a test (second) reflex is influenced by a conditioning (first) reflex. Using identical nearthreshold stimuli, a low-amplitude H-reflex can be evoked with stimulation intervals between 5 and 9 msec (early facilitation), which gradually decays as the interval is increased to 20 msec. Between 20 and 80 msec, Physical TherapyNolume 70, Number YMarch 1990 the reflex is completely inhibited (early depression). As the interval is increased further, the H-wave increases (:second facilitation) but is followed by a transient decline in amplitude between 300 and 800 msec (late depression). A slow return to normal excitability is attained only with intervals longer than 2 seconds. HEALTHY ADULT'S H-REFLEX AND M-RESPONSE RECRUITMENT CURVES Myotatlc Reflexes in Healthy Neonates Studies of the H-reflex and the tendon jerk reflex in healthy newborn infants have demonstrated dserences between healthy neonates and healthy adults. The excitability of the monosynaptic pathway has been studied in newborn infants.27-32 Tests of the Hreflex (H-reflex recruitment curves, WM ratio, and paired stimuli excitability curves) have demonstrated that this reflex pathway of the lower limbs of infants is hyperexcitable compared with that of healthy adults. Prechtl recorded muscle electrical activity from the ipsilateral and contralateral quadriceps femoris (QUAD) and hamstring (HAM) muscle groups following patellar tendon taps.29 The elevated excitability of the myotatic reflex in the neonate has been attributed to a reduced level of supraspinal inhibition33 and to facilitory influences that outweigh inhibition resulting from dfierences in myelination of descending pathwa~s.27!~8 In tendon jerk reflex studies of the full-term neonate,* distinct myotatic reflexes were evoked in 58 healthy newborn infants when serial taps were applied to the tendons of the lower limb (Fig. 5).2334 The neonates were 1 to 4 days old and were determined to be healthy by neurological examination and by history of the pregnancy and delivery. During testing, the irlfant was positioned supine Stimulus Amplitude (V) I Fig. 4. H-reJlexand M-response recruitment curves of healthy adult subject in Figure I . (SOL = soleus muscle; EMG = electromyographic response.) with the hips flexed and externally rotated, the knees flexed, and the ankles in'a neutral position. The infant's head was in the neutral position when asleep and turned to the right when awake. The "state" of consciousness (eg, awake or asleep35) was documented for each tendon tap. Taps were applied to the tendons of the SOL, TA, and QUAD muscles; sole of the foot; and medial malleolus. A twitch was observed with each tendon tap recorded. Four to 43 taps were applied to each tap site for each infant. Tendon jerks were elicited with a modified reflex hammer instrumented.with a strain gauge to measure haqmer force and activate the data-collection system. Surface dfierential myoelectrodes were placed on the skin overlaying the muscle bellies of the antagonist SOL and TA muscles and the QUAD and HAM muscles. §~nthropornetricdata on neonates gives the distance from the pelvis to the sole of the foot as 23.1 a 1.9 to 28.8 2 2.6 cm in 40-week gestational age infants.23.36 Nerve conduction velocities for the tibia1 nerves of full-term infants are 25.8 2 2.0 to 28.8 + 2.0 dsec.37 The resulting approximate conduction time from the ankle to the lumbar spine and back ([2 x 23.1 cmy28.8 d s e c to [2 X 28.8 cmy258 d s e c ) is 16 to 22 msec. These figures are consistent with a rnonosynaptic pathway, but do not preclude the existence of polysynaptic pathways. Physical TherapyNolume 70, Number 31March 1990 Taps to the Achilles tendon frequently evoked almost simultaneous EMG bursts in SOL and TA muscles, of comparable amplitudes and at monosynaptic latencies of approximately 20 msec23§For 537 Achilles tendon taps to 18 neonates, the mean SOL muscle stretch-reflex latency was 19.4 + 1.4 msec and the mean TA muscle response was at 19.6 + 1.3 msec. Sequential Achilles taps in these healthy neonates evoked reflexes that were more variable in amplitude, onset latency, waveform, and ratio of the peak-to-peakstretch-evokedEMG voltages (or "TASOL muscle reflex ratio") than those of the healthy adult. Tendon taps consistently produced near-synchronous (but variable) responses at electrodes over the tapped muscle, the antagonist muscle, and distant muscles of the leg. The onset latency of the Achilles tendon jerk reflex is quite variable among neonates and between successive taps to one neonate. This variability persists even when limb position, head position, and state of consciousness (eg, awake or non-REM [rapid eye movement] sleep) are unchanged. 192155 8 2mv AchBk, Tondm Tap TA Tadon Tap As in all studies using surface EMG -a 7 82mv k#lu Tadon Tap 7 * 7 Fig. 5. (A) Ensemble electromyographicactivityfrom sequential tendon taps to one heal@ I-day-old neonate during non-REM (rapid eye movement) sleep (size appropriate for gestational age, 40 week gestational age by examination and dates, Apgar scores of 9 at 1 minute and at 5 minutes, normal spontaneous vaginal delivety). Surface EMG recordingsfrom gastrocnemius-soleus(SOL) muscle and tibialis anterior (TA) musclefor taps to Acf~illestendon, TA tendon, and patellar tendon. During data collection, record numbers were serially incrernentedfrom 1 to 99 for SOL and TA muscle EMG electrodes. (Adaptedfrom Myklebust et al.34) (B) Simultaneous EMG recordings from SOL, TA, qqudricepsfernoris (QLrAD),and hamstring (HAM) muscles for a single Achilles tendon tap to a dt@erent healthy neonate. During data collection, record numbers were serially incrementedfrom 1 to 99 for SOL and TA muscle EMG electrodes and simultaneous record numbers for QUAD and HAM muscle EMG electrodes were incremmztedfrom 101 to 199. (Adaptedfrom Myklebust.23) As an example, for 80 serial Achilles tendon taps of two different neonates, the SOL muscle reflex latencies were 21.1 +- 2.93 msec and 23.4 + 0.99 msec, respectively. This variability in the latency of the myotatic reflex may be explained by incomplete myelination of the spinal cord and peripheral nerves. Fluctuations in physiological excitability levels would contribute to variability in latencies. Variability in thresholds for synaptic transmission may be attributable to lability of postsynaptic membranes. Furthermore, several monosynaptic and oligosynaptic pathways for stretch 56 / 193 manually applied hammer taps varied from trial to trial. The measured force of tap did not correlate with the amplitude of the evoked agonist EMG activity. That is, "light" taps sometimes evoked reflex EMG responses with amplitudes that were comparable in size to responses to taps of twice the applied force. reflexes may coexist at the time of birth; different circuits with dlferent conduction times may be activated by successive tendon taps. Current research methods do not permit us to determine which (if any) of these anatomic or physiologic conditions may be responsible for the variability in the reflex latency in the newborn infant. Measurements of peak EMG amplitudes were made 18 to 35 msec after the tendon tap (the period that includes the onset and duration of the myotatic reflex). The force of these recordings, the measured amplitude of the reflex EMG response is difficult to compare between taps of a single neonate or among neonates. However, the relative amplitudes of the agonist and the antagonist EMG responses were significantly different in the healthy neonates when compared with those of healthy adults. To quantify the degree of simultaneous activation of SOL and TA muscles, the TASOL muscle reflex ratio was computed. This ratio is a measure of the relative excitabilities of the antagonist muscles for a single tap. The TA:SOL muscle reflex ratios for Achilles tendon taps for all neonates tested were higher than for healthy adults. The mean TA:SOL muscle reflex ratio for 51 neonates was 0.69 + 0.78 (range = 0.12455). This ratio compares with a mean TA:SOL muscle reflex ratio of 0.08 ? 0.04 for healthy adult subjects.23 In an individual infant, the TASOL muscle reflex ratio varied from tap to tap. (For example, the TA:SOL muscle reflex ratios for two neonates were 0.27 + 0.10 and 1.96 + 2.72, respectively.) The relative amounts of muscle activity in the two antagonist muscles varied even in infants who were asleep. From a series of taps during a 30-minute test, there was no trend in the relative amplitudes of muscle activity, even when head and limb position (as well as state of consciousness) were controlled. Electromyographic responses were consistently produced by tapping sites not normally thought to excite shortlatency afferents in the corresponding motoneuron pools. Simultaneous short-latency EMG responses were also recorded from HAM and QUAD muscles when the SOL and TA ten- Physical TherapyNolume 70, Number 3lMarch 1990 dons were tapped (Fig. 5), and the HAM and QUAD muscle responses were nearly coincident with the SOL and TA muscle responses. This phenomenon of reflex-evoked EMG activity from distant limb muscles is called reflex irradiation. Several explanations, which are not mutually exclusive, may account for the large 'TA:SOL muscle reflex ratios of neonates, the short-latency EMG responses from distant muscles, and the EMG 1:esponses recorded from tapping sites such as the TA tendon, the patellar tendon, and the medial malleolus: 1. In these small limbs, the SOL mus- cle EMG signals are electrically volume-conducted from the stretched agonist muscle to electrodes over the antagonist muscle (ie, to the electrode overlying the TA muscle) or over a distant portion of the limb (ie, to the electrode overlying the QUAD or HAM musck:). 11 2. Vibration is mechanically transmit- ted throughout the limb from the tap site to provide an effective stimulus to other muscles of the limb. 3. At birth, muscle spindles are very sensitive to stimulation and sense taps at distant sites. 4. At birth, the spinal cord is physiologically hyperexcitable; therefore, motoneurons respond to afferent signals that would normally be insignificant. 5. Each muscle fiber is innervated by several efferent fibers (as in neonatal rats and kittens and chicken ernbryos)38.39#;each muscle would then be more sensitive to afferent input. 6. Spinal pathways exist for "reciprocal excitation" of antagonist motoneurons by primary afferent fibers. That is, in reciprocal excitation, short-latency spinal cord pathways exist that simultaneously excite the agonist and antagonist muscles (Fig. 3).5,23,*0,44 Reciprocal excitation in neonates is believed to be reflex generated and segmental in 0rigin.~3The EMG response from the stretched SOL muscles, with an onset latency of about 20 msec, is accompanied by time-locked activity in the shortened TA muscle. A parsimonious explanation of the observations of tendon jerk reflexes in healthy neonates may IIVolume conduction of electrical signals is a passive and stable phenomenon. If electrical conduction of SOL muscle activity to electrodes over the TA muscle is responsible for the observed TA muscle response to Achilles tendon tap, then the data should have two features. First, the relative waveforms of the two EMG responses should exhibit a constant relationship from tap to tap with respect to relative amplitudes and latencies as long as the electrodes are not moved. Second, both electrodes 'would be measuring a common signal through different, but invariant, passive tissue filters. As a consequence, the TA:SOL muscle reflex ratio in a single testing session of an individual neonate should be independent of the tap site. However, the data show independent variabiliry of the two EMG responses from tap to tap. Furthermore, the relative changes in the reflex ratio are not consistent between antagonist tap sites in one neonate. By these tests, volume conduction of muscle sigrials is neither a sufficient nor a likely explanation of the data. Finally, with volume conduction, a signal attenuates rapidly with distance so that the more remote electrode pair always yields the smaller EMG signal. This phenomenon is incompatible with the Achilles tendon taps, in which the TA muscle response is sometimes larger than the SOL muscle response. The exclusive role of volume conduction in these data cannot be assessed, and it cannot be excluded as a contributing factor. However, volume conduction is an insufficient explanation of these data because the antagonist EMG signals are often larger than agonist EMG signals, regardless of the tap site. *Pathways other than those responsible for reciprocal inhibition have not been reported in the healthy human. Inappropriate spinal cord connections have been found in the normal development of chicken embryos.40Anomalous pathways in the neuromuscular j~nction3~.3%ndcerebral cortex41 are present in neonatal mammals. In neonatal mammals, reorganization occurs during the postnatal period by the elimination of processes or neuronal death. None of the results of animal studies can be directly applied to human reflex studies. However, variabiliry and plasticiry are features of subprimate neonates that are not apparent in the adult. In many parts of the nervous system, "wirir;g" is rearranged during early postnatal life." Competitive interactions may be "the basis of the human nervous system to adapt to an everchanging external environment."43(~5~~) Physical TherapyNolume 70, Number 3/March 1990 be the presence of functional excitatory connections from primary afferent neurons to both agonist and antagonist motoneuron pools (Fig. 3). We cannot assess the exclusive roles of any of the possible mechanisms of volume conduction, vibration of the limb, hypersensitive muscle spindles, motoneuron hyperexcitability, hyperexcitable motor units, or reciprocal excitation. However, reciprocal excitation provides the most comprehensive (and the most speculative) single explanation of the data. It does not require that a new set of physiological criteria be invoked to explain data of different tap sites, the variability from one tap to the next, or the variability from one infant to the next. This hypothesis does not preclude the contribution of other mechanisms. The mechanisms of reflex irradiation can be proposed to explain the shortlatency responses of muscles that are distant to the tap site (ie, QUAD and HAM muscle responses to SOL and TA tendon taps, SOL and TA muscle responses to patellar taps). All four limb muscle groups are innervated by nerves at the L4 level of the spinal cord. It is possible that at the time of birth, some shared communication exists at this level of the spinal cord among alpha motoneuron fibers to the muscles of the thigh and the calf; stimulation of the muscle spindles in any one of these muscles may result in the spread of the reflex responses, which may be recorded from all the muscles of the leg. We may speculate that during normal maturation the appropriate L4 connections develop between afferent and efferent fibers for a particular muscle and that the inappropriate connections die or are masked. Tests on a small population of healthy children aged 1 year and older have not demonstrated reflex irradiation. On the other hand, reciprocal excitation has been reported in healthy children as old as 3 years of age. The significance of the apparent differences in the time course for the alteration of the functional pathways of reciprocal excitation and reflex irradiation remains to be identified. It is hypothesized that reciprocal excitation and reflex irradiation are properties of tendon jerk reflexes in infancy and that these properties gradually disappear in normal development. That is, "functional" spinal cord pathways are proposed to exist in the neonate, consisting of excitatory connections from primary afferent neurons to agonist and antagonist motoneuron pools (reciprocal excitation) and motoneuron pools of distant muscles (reflex irradiation). These pathways are gradually masked or eliminated during normal development. A ACHILLES TENDON TAPS FROM HEALTHY CHILDREN 30 - K Myotatic Reflexes in Healthy Children H-reflex studies have demonstrated that the excitability of the shortlatency reflex pathway of the neonate decreases in the early years of normal de~eloprnent.*7~2~~3()~31 However, the relationship of changes in stretch reflex excitability to the normal development of motor skills from infancy through early childhood is poorly understood. Preliminary studies of tendon jerk reflexes of the lower limbs have been performed in 15 healthy children aged 1 month to 6 years.* Some children have been tested longitudinally, but most of the data are from a population sampling.23The onset latency of the tendon jerk reflex changes during early childhood development with myelinization of peripheral nerves and central pathways (which tends to increase conduction velocity and thereby shorten the onset latency) and increases in limb length (which tends to increase the onset latency).23 In the 33 tests of 15 children, Achilles tendon jerk reflex latencies ranged from 16.5 + 1.0 msec (representing 20 tendon taps for an 11-month-old child) to 25.3 + 4.5 msec (representing 14 tendon taps for an 8-month-old child) (Fig. 6A). The TA:SOL muscle reflex ratio is used as a quantitative measure of the EMG responses to tendon taps. During the first year of life, there was considerable variability in the TA:SOL mean neonate latency = 19Af 1.4 mscc ACHILLES TENDON TAPS FROM HEALTHY CHILDREN ~umncoMIc TkSOL .4.55 ~aconatcTkSOL 1 healthy sdult TA:SOL = 0.08 f 0.04 minimum nrmate TkSOL 0 0.12 0 12 24 38 48 80 72 Fig. 6. Aterage soleus (SOL) muscle stretch reflex latencies (A) and average r@ex ratiosfor tibialis anterior (TA) and SOL muscles (TA:SOLmuscle reflex ratios) (B)for Achilles tendon taps of 15 children aged 1 to 67 months. Changes in SOL muscle refix latencies over time are compared with the mean refix latency for healthy neonutes. Changes in TA:SOL muscle reJd ratios are compared with minimum, maximum, and mean valuesfrom healthy neonafes and with the healthy adultk mean TA:SOL muscle refix ratio. (Adaptedfrom Myklebust.2.3) muscle reflex ratio for Achilles tendon taps, and the ratio was higher than in the healthy adult in all tests (Fig, 6B). For children aged 1 to 11 months, the largest TA:SOL muscle reflex ratio was 3.34 + 5.32 (repre- senting 14 tendon taps for an 8monthald child) and the smallest reflex ratio was 0.15 ? 0.07 (representing 15 tendon taps for a 10monthald child).23 Physical TherapyNolume 70, Number 3/March 1990 The period from 11 to 24 months of age is the time when the children learned to walk independently. During this time period, the mean TA:SOL muscle reflex ratios were larger than the mean values for adults. By age 4 to 6 years, the mean TA:SOL muscle reflex ratio for each child, which ranged from 0.17 to 0.05, was approaching or comparable to the mean adult values.23 These measures need to be validated in a larger population of healthy children. Furthermore, the significance of these data remains to be identified with respect to changes in locomotor slull acquisition and the ability to hop, jump, and perform tandem ("heel-toe") walking. Postmyotatic Responses and Voluntary Reaction Times in Healthy Children Bawa evaluated changes in the shortlatency (cnyotatic reflex) and longlatency (postmyotatic reflex) responses and simple reaction times of wrist flexor muscles in children from 2 to 10 years of age.45Onset of reflex responses was only slightly different in the 2- to 6-year-old subjects. In children aged 2 to 6 years, the duration of postmyotatic responses was longer than in the adult; by age 8 years, this measure was in the range of the healthy adult. By 10 years of age, "simple" voluntary reaction times**resembled those for adults. Neural processing for simple voluntary reactions is more complex than for reflex responses, and it appears to develop later in childhood. This finding may be due to the gradual developnlent of supraspinal structures or inhibitory spinal mechanisms, increased central conduction velocities, or more effective synaptic transmission. Bawa asserts that the "hardwired" circuitry of reflexes appears to develop earlier than the "open" circuits used in voluntary tasks.45 Myotatic Reflexes in Patients with Cerebral Palsy The myotatic reflex has been compared in patients with spasticity secondary to central nervous system insults acquired in the perinatal period and adulthood.5.44 Electromyographic activity evoked during rapid mechanical dorsiflexion of the ankle joint in patients with CP (eg, birth onset injury to the CNS) differs markedly from that of the healthy adult and patients with stroke, incomplete spinal cord injury, or traumatic head injury (eg, insults to the mature CNS). In severely handicapped adults and children with CP, a strong SOL muscle myotatic reflex is accompanied by simultaneous activation of the antagonist TA muscle (Fig. 2). This pattern of reciprocal excitation evoked by forced ankle rotation is in marked contrast to the reciprocal inhibition normally seen. Reciprocal excitation in patients with perinatal CNS injuries has been confirmed by studies of tendon jerk reflexes46 and H-reflexes using concentric needle EMG electrodes.5 Cerebralpalsy is classically defined as brain injury that occurs during the perinatal period. However, the stretch-reflex behavior in severely handicapped patients with CP with reciprocal excitation suggests that the definition of the disease may need to be revised. A fundamental developmental error in neuronal interconnections of the spinal cord may exist in patients with CP.5 This hypothesis implies that reciprocal excitation in patients with CP reflects functionally disordered spinal cord circuitry. These data suggest that damage to the immature suprasegmental structure may impose a secondary developmental disorder on the spinal cord. This abnormality could represent an emer- **"Simplen is contrasted to "choice" reaction studies. In a simple reaction paradigm, the subject is instructed to make a voluntary movement in o n e direction only. In a choice reaction test, the subject is instructed that his o r her movements will be made in o n e of two (or more) directions, such as wrist flexion o r extension. A visual cue or' target is generally used to specify the direction (and distance) of movement; an auditory cue may be given to prepare the subject for the visual cue. Physical TherapyNolume 70, Number 3/March 1990 gent pathological condition that develops subsequent to perinatal injury (Fig. 3).5 It may also indicate a failure of normal maturation in which the pathway of reciprocal excitation would be suppressed. To distinguish between these alternatives, the pattern of myotatic reflex responses in healthy infants and in infants at risk for CP must be compared and evaluated longitudinally during development. Voluntary Lower Limb Movement and Gait Normal Development of Motor Function in Infants and Chlldren Little information is available on the neural development of human motor control or on the development of neural regulation of locomotion in children and their ability to adapt to the environment.47 Bawa45 and Forssberg and Nashner48 have suggested that changes in supraspinal structures or in the spinal reflex mechanism may correlate with the acquisition of motor slulls. To begin to understand neural control mechanisms in the development of motor control, the kinematics and muscle activity of the lower extremities have been monitored during lucking and stepping movements in infants, as well as in gait in early childhood. Development of lower limb movements. Electromyographic activity has been recorded in response to tactile stimuli in neonates.29 Electromyographic activity and joint kinematics associated with voluntary kicking and stepping movements have been monitored in small populations of infants from birth to the time of first independent steps.4951 In early infancy, lower limb movements usually begin without inhibition by antagonist muscles. In contrast, antagonist inhibition is well-expressed in children between 2.5 and 3 years of age. Voluntary kicking movements of infants in the supine position demonstrate close temporal and spatial synchrony of hip, knee, and ankle joint movements. These rhythmic kicking 196 / 59 movements are associated with simultaneous activation of agonist and antagonist muscles.29~50~~ The reciprocal organization of antagonist muscle contractions during voluntary movements reportedly develops gradually during the first year. The processes of excitation and inhibition appear to undergo continuous development and maturation during early childhood. Voluntary limb movements in healthy neonates may differ from those of the adult because descending pathways may not be complete,49 spinal inhibition may be variable:' and facilitation of the CNS may outweigh inhibiti0n.~7J~ In addition to neural mechanisms, the changes in "biodynamic" properties of body segments during normal growth and development may contribute to the evolving character of voluntary limb movements.50 Interactions between limb biomechanics and neural systems are not well-understood, and they may be even more complicated when neural control is impaired, as in patients with CP. As higher levels of organization are achieved in normal development, neural systems probably undergo d s appearance and remodeling of earlier networks, development of inhibition, and changes in connection of sensory and motor channels in response to the rivalry between developing neural ~atterns.5~ Motor development appears to be uneven in character. Major reorganizations in function probably undergo regressions and transformations, but the underlying neural mechanisms are not known.50 Development of postural-control strategies in stance. Our understanding of the neurophysiological bases for the development of equilibrium in children is fragmentary. Forssberg and Nashner studied strategies used to maintain upright standing when the support surface and visual conditions were changed in children aged 1.5 to 10 years.48 Children younger than 7.5 years of age were unable to suppress responses because of conflicting orienting information and often lost their balance. When evaluated by EMG recruitment patterns, all the children made postural adjustments and used strategies similar to adults. However, the children's EMG responses were more variable and slower than those of adults. In children, the stereotyped automatic postural adjustments of lower limb EMG recruitment patterns are interpreted as evidence for central networks within lower levels of the motor hierarchy that control walking and standing. The variability in responses in children under 7 years of age is evidence that adaptive mechanisms are undeveloped. If the automatic postural system is an elementary unit of motor action that can be integrated into complex behaviors, then the performance limitations of the child result from his or her inability to systematically coordinate elementary units of action into a complex act.43 Berger et a1 report that the pattern of coaaivation of antagonist SOL and TA muscles is predominant when children first change to a bipedal gait from quadrupedal locomotion (crawling); the EMG pattern later becomes reciprocally organized when independent wallung and running develop.47 The authors suggest muscle coactivation at this early stage of development seems to be less related to propelling the body forward in locomotion, but may be important in maintaining the body's equilibrium in the upright posture. Development of gait patterns. Children demonstrate the ability to walk unsupported at about 1 year of age.'.5=54 Children walk independently as early as age 9 months and as late as 17 months.1.52.53 Children who do not walk by age 18 ttVolume conduction of EMG signals from small infant limbs cannot be excluded as a contributing factor. However, the relative amplitudes and waveforms of antagonist EMG signals are not constant in one infant. Therefore, as in studies of the tendon jerk reflex in neonates, it is unlikely that the EMG responses recorded in normal-kicking infants are attributable to volume conduction alone. 601 197 months are usually evaluated for developmental delays.' Gait patterns of children have been studied on level ground52.53.55.56 and using a treadmill with surface EMG recordings.4,47,57Forssberg and Wallberg tested children as young as 5 hours of age and as old as 12 months of age." Limb movements were recorded via light-emitting diodes placed on joints of the lower limbs, and surface EMG responses were recorded from antagonist limb muscles. Reaction forces were recorded in separate trials on a force plate. Burnett and Johnson tested healthy children from 9 months to 11 years of age and compared joint kinematics with cinematography and electrogoniometry.52~53Using cinematography and surface EMG recordings, Berger and colleagues studied gait in healthy children aged 6 months to 10 years and in children with CP.4.47 Ankle joint angles were measured by goniometry, and footswitch&swere used to record foot contactitime. Neonatal gait patterns and stepping in the first 6 months. Newborn infants demonstrate a primitive walking pattern, with extreme hip flexion followed by rapid placement of the forefoot.57 In stance, the limb cannot fully support the body or propel it forward. This sequence of events has been attributed to a "spinal locomotor generator" (ie, "central-pattern generator"). In the proposed neural network, basic activity is generated in the spinal cord; supraspinal centers provide only minor influences.57The early foot contact pattern seen in infancy resembles a digitigrade pattern. Berger et a1 reported that, in the 6month-old infant, forefoot contact with the ground causes a short, quick dorsiflexion of the ankle with a fast stretch of the slightly preactivated calf mu~cles.~7 ~lectrom~o~ra~hic responses were recorded 25 to 30 msec after the onset of stretch at amplitudes two to three times the amplitude of tonic EMG activity. Physical TherapyNolume 70, Number 3March 1990 Electromyographic responses in young infants are irregular and exhibit a high degree of coactivation. The TA muscle is active throughout the step cycle.47.57The gastrocnemius muscle is active prior to foot contact. This fact has been taken as evidence against a 1:eflexively induced response and as evidence in favor of a "central program" for the control of movement patterns.57 Berger et a1 have characterized the "immaturity" of the irregular early stepping pattern of 6-month-old infants by three features: 1) Coactivation of an.tagonist muscles of the leg is prominent and becomes less pronounced when independent steps are first taken; 2) the amplitude of the TA muscle's :EMG response during the swing p h s e of gait is often larger than the gastrocnemius muscle's EMG response in the stance phase of gait; and 3) large-amplitude solitary bursts of EMG activity are evoked, primarily 7 in the gastrocnemius m ~ s c l e . ~These EMG responses are associated with rapid ankle joint movements and, based on constant onset latencies, appear to represent reflex-evoked EMG responses. These data recorded during early stepping suggest that immature gait patterns are under spinal control and may be reflexive. - NORMAL CHILD (D.M.) SUPPORTED WALKING INDEPENDENT WALKING I- l SEC-4 LEFT LWEI) &* SI '-, mwcrc: Y - - W I I- &* LIMB I amI - I H --I I H -4 I HEEL 0 H - I TOE N m l gait patterns in thefirst 7 years. Sutherland et a1 described five kinematic: gait characteristics that change in normal childhood developyears): me duration ment (age of single--limbstance increases with age (especially up to age 2.5 years); 2 ) walking velocity increases steadily (especially up to age 3.5 years); 3) cadence (and its variability) decreases with age; 4) step length increases (especially until age 2.5 years); and 5) the ratio of body width to stride widthss increases rapidly until age 2.5 years, increases more slowly until age 3.5 years, and then plateaus. Furthermore, the "step factor" (step length divided by limb o , s & ~ m ~ s m ~ Ifc IFC Ifc IFC IFC IFC ~ IFC S S IW IFC sIFC Fig. 7. Displacementpatterns of the rght lower limb during supported walking and independent walking of a healthy child. Patterns were measured at 0.07-second intervals through two successive walking cycles. Walking cycles began and ended at the instant of initiulfloor contact (IFC) and consisted of one period of stance (St) and one period of swing (Sw). For sagittal rotation patterns, upward deflections on the ordinate representflemon (FI) and downward deflections represent extension (Ex). Flexion of the ankle is dotstJltxion; extension of the ankle is plantarJlexon. For heel and toe patterns, ordinate values indicate distance of heel target or toe target from floor (0 on ordinate scale). (Reprinted with permision from Statham and Muma-y and J B L@pincott C0.59) length) increases during the first 4 years of life and is suggested as a measure of neuromuscular maturation.58 **The ratio of body width to stride width is computed from the "pelvic span," measured from the level of the anterior superior iliac spines, and from the "ankle spread," the distance between left and right ankle centers during double-limb support. Physical TherapyNolume 70, Number 31March 1990 Statham and Murray also identified differences in hip and ankle flexion and extension patterns and vertical trajectory of the heel and toe in early walking patterns of children (Fig. 7).59 Mature patterns of heel-strike, kneeflexion wave (knee flexion after heelreci~strike! rocal arm swing, and joint angle 198161 rotations throughout the gait cycle are acquired by the age of 3 years, before the development of mature cadence, step length, and walking speed. A longer step length, not greater step frequency, is responsible for increased walking velocity with growth and maturation. Inadequate step length in the immature child appears to be due to lack of stability in the supporting limb. Sutherland et a1 suggests this inadequate step length may be the result of lack of balance, weak ankle plantar-flexor muscles (which would prevent undue drop of the center of mass of the body and allow the body to be extended forward beyond the point of support), or lack of control of these muscles.5~ Electromyographic studies of young children demonstrate that muscle activation changes with age.-'.47.58 Children younger than 2 years of age demonstrate coactivation of TA and gastrocnemius-SOL muscle activity during gait. In children aged 1 to 2 years, the TA muscle's EMG activity is insufficient to lift the foot during the swing phase. In these children, the foot contacts the floor in the foot-flat position, rather than with a heel-strike. The adult-like pattern of reciprocal recruitment of antagonist muscle activation begins to emerge at about 2 years of age with the appearance of a true heel-strike." This EMG pattern, in which the TA muscle's EMG response is electrically silent during most of the stance phase, is generally established and consistent by the age of 5 or 6 years. To compare the movement performance of healthy children with that of children with CP who walk on their toes, Berger et a1 asked healthy 4- and 6-year-old children to perform a toewalking test.47 In the 4-year-old group, biphasic EMG potentials were recorded from the gastrocnemius muscle at stretch reflex latencies following forefoot contact with the ground. In contrast, in the 6-year-old group, contact of the forefoot with the ground did not evoke a stretch reflex. Gait patterns in childrm with deuelopmental disorders. Habitual "toewalkers" (eg, patients with CP) contact the floor with the forefoot. Children with CP aged 8 years and older demonstrate a digitigrade gait pattern, similar to that seen in I-year-old children.47 The EMG patterns associated with toe-walking in children with CP are similar to recordings made from healthy I-year-old chi1dren:'The amplitude of the gastrocnemius EMG response is lower than in healthy children aged 6 years and older, the TA muscle fails to actively dorsiflex the ankle during the swing phase of gait, antagonist muscles of the leg are coactivated during stance, and large reflex EMG signals are recorded at the beginning of the stance phase. It is significant that Berger et a1 have identified stretch-reflex-induced EMG activity during foot contact in older patients with CP.4' Although this EMG pattern is similar to early gait patterns in healthy I-year-old children and in toe-wallung patterns of healthy 4-yearold children, these stretch-evoked EMG responses are abnormal in children after about age 6 years. They suggest that, in children with CP, spinal patterns that control locomotion are impaired before the children learn to walk. As a consequence, children with CP use a simpler and immature locomotor pattern. These patients appear to lack the ability to modify EMG firing patterns to adapt to different environmental conditions and modulate their walking speed. Berger et a1 conclude that during normal maturation, stretch-reflex activity is integrated into preprogrammed muscle activity.47Locomotor patterns of older children with developmental disorders (eg, CP) resemble early gait "The relationship between the EMG patterns evoked in gait and in tendon jerk reflex trials has not been specifically addressed in this context. Preliminary studies suggest that reciprocal excitation is still evocable hy tendon tap in 2- and 3-year-old children, but not in children older than 6 years of age." 62 1199 patterns of young healthy children; the immature patterns fail to be suppressed during development. Movement Deficits in Patients with Spastlclty The effect of impaired stretch reflexes on the performance of voluntary tasks requires further study. In our laboratory,* patients with spasticity secondary to adult-acquired injuries to the CNS (eg, stroke), did not demonstrate stretch-evoked reciprocal excitation of SOL and TA muscles, yet they had limitations in independent ambulation and demonstrated movement deficits, as revealed by clinical examination. On the other hand, the patients we tested with perinatal insults to the CNS did have reciprocal excitation of SOL and TA muscles, were severely limited in voluntary movements of the lower extremities, and were functionally nonambulatory. Reciprocal excitation is not a necessary condition for impaired performance of slulled motor tasks, but it may be a sufficient condition. Tests to evaluate the relationship between impaired voluntary movement and stretch-evoked reciprocal excitation remain to be performed. Corcos et a1 evaluated the ability of patients with spasticity secondary to adult-onset CNS iquries to make accurate, rapid ankle dorsiflexion and plantar-flexion movements over different distances to a target.7 In three of the eight patients tested, dorsiflexion evoked velocity-dependent activation of the antagonist (SOL) muscle, which impeded the movement, and the limb reversed the direction of movement (Fig. 8). The authors propose that this EMG activity is reflexive because it is highly synchronized with the limb movement, has a large peak amplitude, occurs about 50 msec after the initiation of movement, and is velocity dependent. These neurophysiologic criteria must be met to consider these EMG responses as reflexes. It is hypothesized that in some patients with spasticity, hyperactive stretch reflexes in the SOL muscle are Physical The:rapyNolume 70, Number 3lMarch 1990 ing the execution of voluntary movements; therefore, these reflexes may modulate movement performance. Figure 8 demonstrates that in one patient, the voluntary dorsiflexion movement is initiated by a typical EMG burst in the agonist (TA) muscle. The delay from the onset of the TA muscle's EMG response to the onset of dorsiflexion (determined from the velocity trace) is about 45 msec. The further delay to the antagonist (SOL) muscle burst is another 50 msec. Dorsiflexion is arrested in another 80 msec. The latency and pattern of the SOL muscle's EMG response is indistinguishable from what is observed if the ankle were being passively dorsiflexed by a torque motor.5 The magnitude of the stretch-evoked reflex in the SOL muscle is proportional to the stretch velocity, and the latency decreases with increasing stretch velocity. It is proposed that increased velocity in these voluntary movements results in an antagonist TA muscle EMG burst by stretch reflex mechanisms. This EMG activity is often sufficient to arrest the movement and, in some cases, to reverse the direction of movement. Fig. 8. Recordingsfrom agont3t (tibialis anterior [TA]) and antagonist ( s o h (SOL]) muscles, with position and velocity projles for an I8degree ankle dorsiflexion movement to an 8-degree target from an adult with qastic cerebral paly. Electrom~lographicmeasurements are in a r h i ~ r units; y joint angle is measured in degrees, and velocity is measured in degrees per second. (Reprinted with permhion fiom Corcos et a1 and Oxjord UniversiQ Press Inc. 7 ) not incidental to voluntary movements but instead play a causal role in the execution of those movements. In other words, in some patients with spasticity, hyperactive stretch reflexes may be activated dur- The presumed contributions of the stretch reflex to antagonist muscle activity in healthy individuals and in patients with spasticity remain to be determined. However, the patients Corcos et a1 have tested have reflex excitabilities that are greater than normal, which is to their distinct disadvantage.' Some individuals with impairments of voluntary movement may have learned an adaptive mechanism to avoid the problems imposed by hyperreflexia: By slowing their movements, they can reduce their rate of movement to the preferred level. The role of stretch-evoked reciprocal excitation in modulating voluntary movements remains to be evaluated. The patients with CP in whom Myklebust et a1 identified reciprocal excitation were unable to actively dorsiflex and plantar flex the ankle more than a few degreess; therefore, the authors cannot comment on the impact of reciprocal excitation in modulating Physical TherapyNolume 70, Number 3/March 1990 voluntary movements in these patients. Berger et a1 have suggested that patients with CP who walk on their toes appear to lack the ability to modify EMG firing patterns to modulate their walking speed.47Whether these patients also have reciprocal excitation of SOL and TA muscles has not been determined by tendon jerk reflex studies. It is possible that both reciprocal excitation and hyperreflexia of spasticity interfere with the execution of rapid voluntary movements because movements that are "too fast" evoke a stretch reflex and reverse the direction of movement. It is also possible that patients with spasticity "intentionally" move slowly because their impaired stretch reflexes do affect the execution of movements. The possibility of differential effects on voluntary movement performance of reciprocal excitation and hyperreflexia has not been assessed. The relationships of impaired stretch reflexes and abnormal voluntary limb movements, including gait, will require further study in patients with spasticity. The development of stretch reflexes and the impact that reflexes may have on the acquisition of normal motor and locomotor skills will also need to be tested in healthy and developmentally delayed children. Summary As previously stated, Bawa suggested that the "hard-wired" circuitry of reflexes appears to develop earlier than the "open" circuits used in voluntary tasks.45 Studies of the stretch reflex in infancy and childhood also suggest that even the stretch reflex pathways may not be "hardwired,"22.23.34 as previously described by classical studies of neurophysiology. That is, the spinal pathways of reciprocal inhibition have characterized our understanding of spinal cord circuitry for a hundred years. However, studies of ddferences in myotatic reflex responses in infants and children suggests that spinal cord circuitry in normal early development may be more complicated than the simple spinal pathway of the healthy adult. Plasticity of the "wiring" of the spinal cord may help us explain the existence of reciprocal excitation in infancy and the apparent modulation of reciprocal excitation in early childhood until the pattern of reciprocal inhibition emerges later in childhood. Studies of the healthy neonate suggest that stretch-evoked reciprocal excitation and reflex irradiation may be properties of the normal spinal cord in early development, before the acquisition of motor skills. In the healthy infant, the pathway of reciprocal inhibition may develop later, o r it may be present at birth but with a higher threshold than the pathways of reciprocal excitation and reflex irradiation. The normal spinal cord pathway of reciprocal inhibition may fail to develop in children with CP, or abnormal suprasegmental structures may foster the persistence of the reciprocally excitatory pathways. The possibility of the causal role of reciprocal excitation and reflex irradiation in impaired ambulation in children with CP requires further study. Precise relationships between reciprocal excitation (and reflex irradiation) and impaired voluntary movements have not yet been determined in patients with CP or spasticity secondary to adult-onset CNS injuries. However, reciprocal excitation and reflex irradiation may be a sufficient, although not a necessary, cause of impairments in skilled movements. Measures of the myotatic reflex and gait in children may help us understand the physiologic mechanisms of motor control in normal early development, as well as the pathophysiology of delayed and abnormal development in children with perinatal-onset CNS injuries. The changing pattern of reciprocal excitation in the healthy child may have a direct impact on the time that independent ambulation begins; failure of the CNS to suppress o r inhibit this functional pathway at an appropriate time may make independent ambulation impossible. Correlated studies of tendon jerk reflexes and kinematic and EMG mea- 64 / 201 sures during gait in healthy children and in children with CP could be used to construct an objective index of development. Berger et a1 have demonstrated that the antagonist leg muscles of children with CP who walk on their toes are coactivated during stance and that an abnormal burst of SOL muscle EMG activity is evoked at a short latency after the toe contacts the floor.47Because this burst of SOL muscle EMG activity occurs at a short latency following the toe contact and the response is obligatory and stereotypic, this abnormal EMG activity in gait is presumed to result from an abnormal spinal reflex. Whether these same children have reciprocal excitation evoked by tendon jerk reflexes has not been determined. Coexistence of stretch-evoked reciprocal excitation and abnormal reflex EMG activity in gait is not sufficient to demonstrate that the same spinal reflex pathways are responsible for these two types of abnormal behavior or that reciprocal excitation causes toe-walking. Moreover, we may never be able to prove the anatomic or physiologic mechanism of either reciprocal excitation or reflex EMG responses in gait. The same caveats apply to identification of patterns of tendon jerk reflexes and kinematic and EMG changes during normal childhood development. That is, if reciprocal excitation disappears (or decreases to some low o r infrequently triggered level) at the same time children make their first independent steps, this fact does not prove that these events are related. The coexistence of two events in time does not guarantee a causal role o r that these events are correlated. However, without records of both tendon jerk reflex data and gait data in children, we will not be able to evaluate the hypothesis that reciprocal inhibition must be a dominant feature of spinal cord circuitry at a critical time in human development for children to be able to learn to take steps and walk independently and without deviations. Preliminary studies to address this issue are being conducted.GO* The identification of a "template" of normal development of motor coordination, by tests of tendon jerk reflexes and gait, could provide a method of screening developmental delays or disabilities in children as well as a predictive index of development for early assessment of neurodevelopmental delays of locomotor skills. Such a template could also provide an objective assessment tool to evaluate the effectiveness of early therapeutic intervention in children with motor delays. If this template of motor development can be designed, then we may be able to make better recommendations about therapeutic interventions to minimize motor handicaps. The clinical utility of such investigations of the myotatic reflex and gait in children may be understood by the following hypothetical scenario. Suppose we have identified that, in children aged 18 to 24 months, the persistence of reciprocal excitation or reflex irradiation (monitored in tendon jerk reflex studies) is consistently associated with persistent obligatory toe-walking, with abnormal reflex EMG responses evoked at foot contact, and with impaired velocity profiles at the knee and ankle. We might then develop biofeedback exercise programs61 or inhibitory casting methodsG2.@or evaluate other pharmacologic or surgical methods that may modulate the abnormal stretch reflexes in these children. If methods are developed to modulate abnormal reflexes and minimize gait abnormalities in 2-year-old children, then we may introduce these therapeutic measures as a preventive therapy in younger children. We may be able to use longitudinal tendon jerk reflex evaluations as an early identification measure to screen children of about 1 year of age who are "at risk" for toewalking and other gait abnormalities and as a method of deciding which children will benefit from this early preventive therapy. Physical TherapyNolume 70, Number 3/March 1990 How children construct coordinated actions or what neurological, psychological, and environmental conditions are essential for the development of motor slulls is largely unknown. Maturation is necessary,"* but it is probably not sufficient for human motor development,"5 as witnessed in the individual. variability in achieving motor milestones. Similarly, experience is not a sufficient condition for motor slull acquisition, such as learning to walk. Although we do not understand all of the controlling circumstances of motor skill acquisition, research on motor development of children has identified the following: 1. The onset of voluntary motor skills does not occur if primitive reflexes (and a.ssociated motor automatism) of infancy persist." That is, conlplex motor skills require flexibility in their organization and cannot develop in the presence of obligarory reflex-induced motor stereoiypes. 2. The ability to increase the speed and accuracy of movement requires practice. 3. At a certain age, children can learn from past performance to improve their motor output. 4. The ability to acquire a motor skill depends on the inhibition of extraneous movements, a process that requires effort. 5. The brain is required for the adjustments necessary for motor coordination.65 In addition to the neural development required for acquisition of locomotor skills, Thelen suggests that biodynamic changes occur in early childhood.' During the first year of life, the center of mass moves closer to the legs, which increases the eficiency of' locomotion. Strength of the limb and trunk muscles increases for support, and a balance between flexor and exte~nsormuscle groups develops. According to Thelen, Learning to walk is a complex, gradual process of maturation of motivation, the integration of subcortical patterngenerating centers with neural substrate for control of posture and balance, and important changes in body proportions and bone and muscle strength.z(pl39) Acknowledgment I am indebted to Gerald L Gottlieb, PhD, for his collaborative efforts in the scientific endeavors described in this manuscript. References 1 Lundberg AE: Normal and delayed walking age: A clinical and muscle morphological and metabolic study. In Berg K, Eriksson BO (eds): Children and Exercise. Baltimore, MD, University Park Press, 1979, vol 10, pp 23-31 2 Thelen E: Learning to walk is still an " o l d problem: A reply to Zelazo (1983). Journal of Motor Behavior 15:139161, 1983 3 Dietz V: Role of peripheral aEerents and spinal reflexes in normal and impaired human locomotion. Rev Neurol (Paris) 143:241-254, 1987 4 Berger W, Quintern J, Dietz V: Merent and efferent control of stance and gait: Developmental changes in children. Electroencephalogr Clin Neurophysiol 66:244-252, 1987 5 Myklebust BM, Gotrlieb GL, Penn RD, et al: Reciprocal excitation of antagonistic muscles a a differentiating feature in spasticity. Ann Neurol 12:367-374, 1982 6 Berger W, Horstmann G, Dietz V: Tension development and muscle activation in the leg during gait in spastic hemiparesis: Independence of muscle hypertonia and exaggerated stretch reflexes. J Neurol Neurosurg Psychiatry 47:1023-1033, 1984 7 Corcos DM, Gottlieb GL, Penn RD, et al: Movement deficits caused by hyperexcitable stretch reflexes in spastic humans. Brain 109:1043-1058, 1986 8 Inman VT, Ralston HJ, Todd F: Human Walking. Baltimore, MD, Williams & Wilkins, 1981 9 Dietz V. Quintern J, Berger KT:Corrective reactions to stumbling in man: Functional significance of spinal and transcortical reflexes. Neurosci Lett 44131-135, 1984 10 Greenwood R, Hopkins A: Monosynaptic reflexes in walking man. J Neurol Neurosurg Psychiatry 40:448454, 1977 11 Llewellyn M, Prochazka A, Vincent S: Transmission of human tendon jerk reflexes during stance and gait. J Physiol (Lond) 382:82P, 1987 12 Pierrot-Deseilligny E, Bergego C, Mazieres L: Reflex control of bipedal gait in man. Adv Neurol39:699-716, 1983 13 Stein RB, Capaday C: The modulation of human reflexes during functional motor tasks. TINS 11:32%332, 1988 14 Tatton and Lee, referred to in Brooks VB: The Neural Basis of Motor Control. New York, NY, Oxford University Press Inc, 1986 Physical TherapyNolume 70, Number 3/March 1990 15 Jaeger RJ: Stretch-evoked Myoelectric Responses at the Human Wrist. Doctoral Dissertation. Urbana, IL, University of Illinois, 1981 16 Gottlieb GL, Agarwal GC: Response to sudden torques about ankle in man: Myotatic reflex. J Neurophysiol 42:91-106, 1979 17 Burke D, Grandevia SC, McKeon B: Monosynaptic and oligosynaptic contributions to human ankle jerk and H-reflex. J Neurophysiol 52435448, 1984 18 Lloyd DPC: Conduction and synaptic transmission of reflex response to stretch in spinal cats. J Neurophysiol 6:317-326, 1943 19 Agarwal GC, Berman BM, Lohnberg P, et al: Studies in postural and control systems: 11. Tendon jerk input. lEEE Trans Syst Sci Cybernet 6:122-125, 1970 20 Gottlieb GL, Agarwal GC: Effects of initial conditions on the Hoffmann reflex. J Neurol Neurosurg Psychiatry 34:225230, 1971 21 Myklebust BM, Gottlieb GL, Agarwal GC: Orientation-induced artifacts in the measurement of monosynaptic reflexes. Neurosci Lett 48:223-230, 1984 22 Myklebust BM, Gottlieb GL, Agarwal GC, et al: Stretch retlexes in children. Soc Neurosci Abstr 10:915, 1984 23 Myklebust BM: On the Tendon Jerk Reflex in the Human iieonate. Doctoral Dissertation. Chicago, IL, Rush University, 1986 24 Gottlieb GL: Interactions Between the Voluntary and Postural Mechanisms of the Human Motor System. Doctoral Dissertation. Urbana, IL, University of Illinois, 1970 25 Guiheneuc P: The use of monosynpatic retlex responses in man for assessing the different types of peripheral neuropathies. In Desmedt JE (ed): Motor Control Mechanisms in Health and Disease. New York, IVY, Raven Press, 1983, vol39, pp 927-949 26 Goodgold J, Eberstein A: Electrodiagnosis of Neuromuscular Diseases. Baltimore, MD, Williams & Wilkins, 1977 27 Mayer RF, Mosser RS: Excitability of motorneurons in infants. Neurology 19:932-945, 1969 28 Mayer RD, Mosser RS: Maturation of human reflexes. In Desmedt JE (ed): New Developments in Electromyography and Clinical Neurophysiology. Basil, Switzerland, S Karger AG, Medical and Scientific Publishers, 1973, vol 3, pp 294-307 29 Prechtl HFR: Exteroceptive and tendon reflexes in various behavioral states in the newborn infant Biol Neonate 11:159175, 1967 30 Thomas JE, Lambert EH: Ulnar nerve conduction velocity and H-reflexes in infants and children. J Appl Physiol 15:l-9, 1960 31 Vecchierini-Blineau MF, Guiheneuc P: Excitability of the monosynaptic reflex pathway in the child from birth to four years of age. J Neurol Neurosurg Psychiatry 44:309-314, 1981 32 Hodes JR, Gribetz I: H-reflexes in normal human infants: Depression of these electrically induced reflexes (EIRs) in sleep. Proc Soc Exp Biol Med 110:557-580, 1962 33 Vecchierini-Blineau MF, Guiheneuc P: Electrophysiological study of the peripheral nervous system in children. J Neurol Neurosurg Psychiatry 42:753-759, 1979 34 Myklebust BM, Gottlieb GL, Agarwal GC: Stretch reflexes in human infants. Dev Med Child Neurol 28:440449, 1986 35 Prechtl HFR: The behavioral states of the newborn infant: A review. Brain Res 76:185212, 1974 36 Snyder RG, Schneider LW, Owings Cl., et al: Anthropometry of Infants, Children and Youths to Age 18 for Produce Safety Design SP-450. Warrendale, PA, Society of Automotive Engineers, 1970 37 Goeschen K, Purta M, Rothe J, et al: Measurement of motor nerve conduction velocity: Precise method of estimating maturity in newborns. Br J Obstet Gynaecol 9061-68, 1983 38 Bagust J , Lewis DM, Westerman RA: Polyneuronal innervation of kitten skeletal muscle. J Physiol (Lond) 229241-255, 1973 39 O'Brien RAD, Ostberg AJC, Vrbova G: Observations on the elimination of polyneuronal innervation in developing mammalian skeletal muscle. J Physiol (Lond) 282:571-582, 1978 40 O'Donovan MJ, Lee MT: Excitatory sensorimotor connections between anlagonists in the isolated chick embryo spinal cord. Soc Neurosci Abstr 14:579, 1988 41 Stanfield BB: Postnatal organization of cortical projections: The role of collateral elimination. Trends Neurosci 737-41, 1984 42 Thompson WJ: Changes in the innervation of mammalian skeletal muscle fibers during postnatal development. Trends Neurosci 9:2528, 1986 43 Easter SS, Purves D, b k i c P, et al: The changing view of neural specificity. Science 230:507-511, 1985 44 Gottlieb GL, Myklebust DM: Some effects of cerebellar stimulation of cerebral palsy patients: Changes in spinal reflexes and ankle joint complia~ice.In Myklebust JB, et al (eds): Neural Stimulation. Boca Raton, FL,CRC Press Inc, 1985, vol 2 45 Bawa P: Neural development in children: A neurophysiological study. Electroencephalogr Clin Neurophysiol 52:24'+256, 1981 46 Gottlieb GL, Myklebust BM, Penn RD, et al: Reciprocal excitation of muscle antagonists by the primary aferent pathway. Exp Brain Res 46:454456, 1982 47 Berger W, Altenmueller E, Dietz V: Normal and impaired development of children's gait. Human Neurobiol 3:16%170, 1984 48 Forssberg H, Nashner LM: Ontogenetic development of postural control in man: Adaptation to altered support and visual conditions. Neuroscience 2:545-552, 1982 49 Gatev V: Role of inhibition in the development of motor coordination in early childhood. Dev Med Child Neurol 14335-341, 1972 50 Thelen E: Developmental origins of motor coordination: Leg movements in human infants. Dev Psychobiol 18:l-22, 1985 51 Thelen E, Cooke DW: Relationship between newborn stepping and later walking: A new interpretation. Dev Med Child Neurol 29:38&393, 1987 52 Burnett CN, Johnson EW: Development of gait in childhood: Part 1. Method. Dev Med Child Neurol 13196-206, 1971 53 Burnett CN, Johnson EW: Development of gait in childhood: Part 11. Dev Med Child Neurol 13207-215, 1971 54 Grillner S: Control of locomotion in bipeds, tetrapods, and fish. In Brooks VB (ed): Motor Control: The Nervous System. Philadelphia, PA, American Physiological Society, 1981, vol 2, pp 1173-1236 55 Sutherland DH, Olshen RA, Biden EN, et al: The Development of Mature Walking. Philadelphia, PA, J B Lippincott Co, 1988 56 Sutherland DH: Gait Disorders in Childhood and Adolescence. Baltimore, MD, Williams & Wilkins, 1984 57 Forssberg H, Wallberg H: Infant locomotion: A preliminary movement and electromyographic study. In Berg K, Eriksson BO (eds): Children and Exercise. Baltimore, MD, University Park Press, 1979, vol 10, pp 3 2 4 0 58 Sutherland DH, Olshen R, Cooper L, et al: The development of mature gait. J Bone Joint Surg [Am]62:336-353, 1980 59 Statham L, Murray MP: Early walking patterns of normal children. Clin Orthop 79%-24, 1971 60 Myklebust DM, Gottlieb GL, Tomski MA, et al: Myotatic reflexes and gait: Relative roles in early development and successful aging. Soc Neurosci Abstr 14:263, 1988 61 Harrison A: Spastic cerebral palsy: Possible spinal interneuronal contributions. Dev Med Child Neurol 30:76'+780, 1988 62 Hinderer KA, Harris SR, Purdy AH, et al: Effects of "tone-reducing" vs standard plastercasts on gait improvement of children with cerebral palsy. Dev Med Child Neurol 30:37& 377, 1988 63 Malouin F, Richards CL, Dumas F, et al: Interactions in the modifications induced by prolonged muscle stretch on reflex, voluntary and semi-automatic muscle activations. Soc Neurosci Abstr 14:62, 1988 64 Gesell AL, Amatruda CS: Developmental Diagnoses: Normal and Abnormal Child Dttvelopment-Clinical Methods and Pediatric Applications. New York, NY, Hoeber, 1947 65 Wolff PH: Theoretical issues in the development of motor skills. In: Developmental Disabilities in Preschool Children. Laurel, MD, Intellectual Spectrum, 1981 66 Milani-Comparetti A, Gidoni EA: Pattern analysis of motor development and its disorders. Dev Med Child Neurol 9625-630, 1967 Physical TherapyNolume 70, Number 3lMarch 1990