Breath Sounds
advertisement

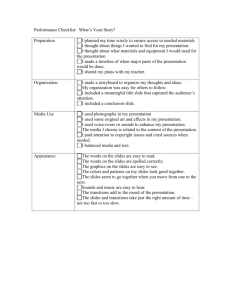
Pulmonary Concepts In Critical Care Breath Sounds There have been Visitors to this website. Return to Nurse Bob's© Page Planning For a Good Assessment One of the most important parts for any patient assessment essence annihilation of the breath sounds. The best way to do that is with ausculation, that is listening with a stethoscope. Often within an intensive care unit, it is difficult to create a quiet environment to listen to breath sounds. Even after turning off televisions and unnecessary equipment there is still quite a bit of noise within the intensive care unit. The patient should be setting up, or setting on the side of the bed when the examination is performed. Ideally, he should have his arms crossed in front of his chest while setting on the side of the bed. However, at times this is not possible, due to the patient's mental status, or physical condition. It's always a good idea to ask for assistance when setting patients up until you determine the patients physical capabilities.when listening to patients with a stethoscope it is always good practice to listen with a stethoscope pressed directly on the patients again. Always insure that the patient is comfortable, he should be drapped and only those areas required for examination should be expose. it is not a good idea among the attempt to listen to breast sounds when the patient is uncomfortable, uncooperative, or in pain. Of course, the stethoscope should be warmed before use. When listening to thepatient's chest, it is always a good idea to do it in a symmetrical manner. First listen to the left side, then listen to the right side in the same location to determine if there's any difference. it's a good idea to start I still waiting at the apex of the lungs and then glue from side aside to Perry as you approach the basis. Remember, is best to do it the same way, in the same sequence, every time. If you get abnormal breath sound title is around it to time to locate its exact extent and character. Categories of Breath Sounds 1. Normal Breath Sounds As mentioned previously, breath sounds categorized according to their location; pitch, intensity, and inspiratory to expiretory ratio. As an air travels through the bronchial tree and pulmonary branches breast sounds are produced. This turbulence is created with each expiration as well as inspiration. When there are no obstructions to the airways normal air movement occurs, this is normal breath sounds. However, when there is an obstruction, by such things as constriction, fluid, or hyperexpansion, abnormal breath sounds will occur. Tracheal Breath Sound: These sounds are usually relatively high pitched and loud. They are equal and a length. They our best heard in the neck over and the trachea. Unfortunately, for this reason, the sounds are not often ausculated. Vesicular Breath Sound: The vesicular breath sound is the major normal breath sound and is heard over most of the lungs. They sound soft and low-pitched. The inspiratory sounds are longer than the expiratory sounds. Vesicular breath sounds may be harsher and slightly longer if there is rapid deep ventilation (eg post-exercise) or in children who have thinner chest walls. As well, vesicular breath sounds may be softer if the patient is frail, elderly, obese, or very muscular. iii. Bronchial Breath Sound Bronchial breath sounds are very loud, high-pitched and sound close to the stethoscope. There is a gap between the inspiratory and expiratory phases of respiration, and the expiratory sounds are longer than the inspiratory sounds. If these sounds are heard anywhere other than over the manubrium, it is usually an indication that an area of consolidation exists (ie space that usually contains air now contains fluid or solid lung tissue). iv. Bronchovesicular Breath Sound These are breath sounds of intermediate intensity and pitch. The inspiratory and expiratory sounds are equal in length. They are best heard in the 1st and 2nd ICS (anterior chest) and between the scapulae (posterior chest) - ie over the mainstem bronchi. As with bronchial sounds, when these are heard anywhere other than over the mainstem bronchi, they usually indicate an area of consolidation. 2. Abnormal Breath Sounds i. Absent or Decreased Breath Sounds There are a number of common causes for abnormal breath sounds, including: ARDS: decreased breath sounds in late stages Asthma: decreased breath sounds Atelectasis: If the bronchial obstruction persists, breath sounds are absent unless the atelectasis occurs in the RUL in which case adjacent tracheal sounds may be audible. Emphysema: decreased breath sounds Pleural Effusion: decreased or absent breath sounds. If the effusion is large, bronchial sounds may be heard. Pneumothorax: decreased or absent breath sounds ii. Bronchial Breath Sounds in Abnormal Locations Bronchial breath sounds occur over consolidated areas. Further testing of egophony and whispered petroliloquy may confirm your suspicions. 3. Adventitious Breath Sounds i. Crackles (Rales) Crackles are discontinuous, nonmusical, brief sounds heard more commonly on inspiration. They can be classified as fine (high pitched, soft, very brief) or coarse (low pitched, louder, less brief). When listening to crackles, pay special attention to their loudness, pitch, duration, number, timing in the respiratory cycle, location, pattern from breath to breath, change after a cough or shift in position. Crackles may sometimes be normally heard at the anterior lung bases after a maximal expiration or after prolonged recumbency. The mechanical basis of crackles: Small airways open during inspiration and collapse during expiration causing the crackling sounds. Another explanation for crackles is that air bubbles through secreations or incompletely closed airways during expiration. Conditions: ARDS asthma bronchiectasis chronic bronchitis consolidation early CHF interstitial lung disease pulmonary edema ii. Wheeze Wheezes are continuous, high pitched, hissing sounds heard normally on expiration but also sometimes on inspiration. They are produced when air flows through airways narrowed by secretions, foreign bodies, or obstructive lesions. Note when the wheezes occur and if there is a change after a deep breath or cough. Also note if the wheezes are monophonic (suggesting obstruction of one airway) or polyphonic (suggesting generalized obstruction of airways). Conditions: asthma CHF chronic bronchitis COPD pulmonary edema iii. Rhonchi Rhonchi are low pitched, continous, musical sounds that are similar to wheezes. They usually imply obstruction of a larger airway by secretions. iv. Stridor Stridor is an inspiratory musical wheeze heard loudest over the trachea during inspiration. Stridor suggests an obstructed trachea or larynx and therefore constitutes a medical emergency that requires immediate attention. v. Pleural Rub Pleural rubs are creaking or brushing sounds produced when the pleural surfaces are inflammed or roughened and rub against each other. They may be discontinuous or continuous sounds. They can usually be localized a particular place on the chest wall and are heard during both the inspiratory and expiratory phases. Conditions: pleural effusion pneumothorax vi. Mediastinal Crunch (Hamman’s sign) Mediastinal crunches are crackles that are synchronized with the heart beat and not respiration. They are heard best with the patient in the left lateral decubitus postion. As with stridor, mediastinal crunches should be treated as medical emergencies. Conditions: pneumomediastinum Summary Type Characteristic Intensity Pitch Description harsh; not routinely auscultated tracheal loud high vesicular soft low bronchial very loud high Normal bronchovesicular medium medium absent/decreased . . bronchial . . Abnormal Location over the trachea most of the . lungs over the sound close to manubrium stethoscope; gap (normal) or between insp & exp consolidated sounds areas normally in 1st & 2nd ICS anteriorly and between scapulae . posteriorly; other locations indicate consolidation heard in ARDS, asthma, ateletasis, emphysema, pleural . effusion, pneumothorax indicates areas of . consolidation discontinuous, may nonmusical, brief; sometimes more commonly be normally crackles (rales) wheeze Adventitious rhonchi stridor pleural rub mediastinal crunch Return to Nurse Bob's Page be normally soft (fine heard on inspiration; high (fine heard at ant. crackles) assoc. w/ ARDS, crackles ) or lung bases or loud asthma, low (coarse after max. (coarse bronchiectasis, crackles) expiration or crackles) bronchitis, after consolidation, early prolonged CHF, interstitial lung recumbency disease continuous sounds normally heard on can be expiration; note if anywhere monophonic over the (obstruction of 1 lungs; high expiratory airway) or polyphonic produced (general obstruction); when there assoc. w/ asthma, is CHF, chronic obstruction bronchitis, COPD, pulm. edema continuous musical sounds similar to low expiratory wheezes; imply . obstruction of larger airways by secretions musical wheeze that heard suggests obstructed loudest over . inspiratory trachea or larynx; trachea in medical emergency inspiration creaking or brushing usually can sounds; continuous be localized or discontinuous; . insp. & exp. to particular assoc. w/ pleural place on effusion or chest wall pneumothorax crackles best heard not synchronized w/ w/ patient in synchronized . heart beat; medical left lateral w/ emerg.; assoc. w/ decubitus respiration pneumomediatstinum position