Vaginitis - Diagnosis, Treatment & Follow-up
advertisement

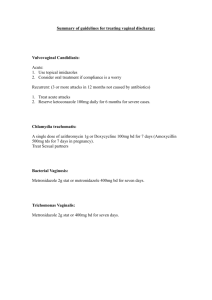
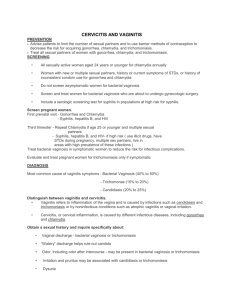
Vaginitis – Diagnosis & Treatment Herbert L. Muncie, Jr. MD 23 year old female complains of a vaginal discharge. What questions do you want to ask regarding the symptom? Evaluating Patients with Vaginal Symptoms History Duration - acute or chronic Medications - taking or used Associated symptoms Itching Burning Dyspareunia Description of any discharge Color and consistency Odor Continuous, spontaneous Amount – copious, more or less than usual What do you want to look for on the physical examination? Evaluating Patients with Vaginal Symptoms Physical examination External genitalia z z Vaginal vault z z Excoriation, spontaneous discharge at introitus satellite lesions consistency of discharge adherence to side walls Cervix z z discharge from os, friability motion tenderness – less likely vaginitis Evaluating Patients with Vaginal Symptoms Physical examination Uterus Size z Tenderness – less likely vaginitis z Adenexa Tenderness – less likely vaginitis z Masses z What diagnostic test will you do for this patient? Evaluating Patients with Vaginal Symptoms Routine laboratory evaluation Wet prep z z z KOH with whiff test Normal saline http://depts.washington.edu/nnptc/online_training/wet_pr eps.html (Tutorial) Vaginal pH (normal 3.8 – 4.4) Cultures for chlamydia and gonorrhea z z Association with discharge not confirmed Test if < age 25, fever or abdominal pain, symptomatic partner, new sexual partner, > 1 sexual partner What are the most common causes of vaginitis? Common Etiologies of Vaginal Discharge Bacterial vaginosis 40-50% of cases. Vulvovaginal candidiasis 20-25% of cases. Trichomoniais 15-20% of cases. Atrophic vaginitis Bacterial Vaginosis Symptoms Unpleasant vaginal odor Odor due to anaerobic bacterial production of amines volatilized in alkaline environment z Menstrual blood & semen alkaline - odor strongest following intercourse or during menstruation z Lack of odor practically eliminates the diagnosis z Spontaneous discharge Vulvar itching, irritation occasionally Bacterial Vaginosis Physical findings No erythema Spontaneous thin homogeneous adherent discharge White to gray-white in color z Often visible on labia prior to speculum z Bacterial Vaginosis -Laboratory Wet prep - KOH + whiff test Normal saline - clue cells Exfoliated vaginal squamous epithelial cells covered with vaginal bacteria obscure cell borders z Lack of WBC support diagnosis z pH > 4.5 (pH< 4.5 excludes BV) z Do not measure cervical mucous pH which is higher around 7 Cultures have no part in the diagnosis Normal findings on wet prep Bacterial Vaginosis - Treatment Metronidazole 500 mg po bid x 7 days (lowest recurrence rate SOR-A) 750 mg qd x 7 days 2 gm po once less effective Metronidazole gel (Metrogel) 0.75% 5g intravaginally qd or bid x 5 days (SORA) Bacterial Vaginosis - Treatment Clindamycin Cream 2%, 5 g intravaginally qhs x 7 days z Clindamycin cream is oil-based and might weaken latex condoms or diaphragms 300 mg po bid x 7 days. 100 mg intravaginal x 3 days effective Bacterial Vaginosis - Treatment Partner treatment does not reduce recurrences Longer treatment (10-14 days) of metronidazole for relapses (SOR-C) Vulvovaginal candidiasis Symptoms Pruritis (70- 90% complain) z Odor z Absence increases likelihood Burning upon urination or dyspareunia White, thick, spontaneous discharge z z Lack of itching decreases likelihood “Cheesy” description increases likelihood Watery discharge makes it less likely Women who complain of “another” yeast infection are more likely to have one Vulvovaginal candidiasis Physical findings Minimal erythema Thick, white, adherent discharge Thick curdled discharge – PPV 84% (SORB) Vulvovaginal candidiasis Laboratory findings Wet prep - KOH + hyphae, pseudohyphae z Normal saline - negative pH < 5 Routine cultures not helpful - 10-20% healthy women positive Culture when: Negative microscopy but compatible clinical picture & normal pH & failed empiric Rx z Before embarking on long term suppressive Rx z Treatment Uncomplicated VVC Agent Type Gyne-Lotrimin 1 % (Mycelex-G) cream 100 mg 100 mg Femstat 2% cream Gynezole 1 2% cream* Monistat 2% cream 100 mg 200 mg Dose Freq. 5g 1 qd 1 bid 1 tab 5g 5g 7-14 d 7d 3d once 3d once 5g 1 qd 1 qd 7d 7d 3d Treatment Uncomplicated (Rx) Agent Type Nizoral 400 mg po Bid 5d Sporanox 200 mg po Bid 200 mg po Qd 150 mg po 1 tab 1d 3d once 0.4%cream 0.8%cream 80 mg 6.5 % oint. 7d 3d 3d once Diflucan Terazol Vagistat Dose 5g 5g 1 qd 5g Freq. Trichomoniasis Symptoms Intermittently spontaneous discharge Thin, slightly yellow-green discharge Often malodorous, fishy odor Rare itching, no burning Physical findings Minimal erythema Thin, slightly clear, yellowish discharge Punctate hemorrhagic cervical lesion pathognomonic but only seen in 2% cases (SORB) Trichomoniasis Laboratory findings Wet prep - normal saline positive for trichomonads. Wet prep positive in 50-70% culture positive cases. z PAP smear - false positive not uncommon [Krieger 1988] z pH > 4.5 Culture more sensitive than microscopy Trichomoniasis - Treatment Metronidazole - 2 g po once Tinidazole (Tindamax) – 2 g once May be better tolerated Metronidazole - 500 mg bid x7 days > 90% cure rate when partner treated simultaneously Aerobic Vaginitis Common after treatment for BV with metronidazole Metronidazole ineffective against strep so can get overgrowth post treatment Aerobic Vaginitis Symptoms white creamy discharge non-pruritic Laboratory normal squamous cells absence of white cells absence of lactobacilli. Aerobic Vaginitis Treatment Milder cases resolve spontaneously Amoxicillin 500 mg tid x 10 days Topical clindamycin (SOR-C) Question - Vaginitis 1. In patients whom you clinically suspect have vulvovaginal candidiasis, a culture would be indicated when? a) b) c) d) Patients who fail initial therapy Patients with normal microscopy and pH Patients who fail three different therapies Pregnant patients at their initial appointment Question - Vaginitis 1. In patients whom you clinically suspect have vulvovaginal candidiasis, a culture would be indicated when? a) b) c) d) Patients who fail initial therapy Patients with normal microscopy and pH Patients who fail three different therapies Pregnant patients at their initial appointment Question - Vaginitis 2. In patients whom you clinically suspect have trichomoniasis, a culture is? a) b) c) d) Never helpful in making diagnosis More sensitive than microscopy Good for screening pregnant patients Only used in research studies Question - Vaginitis 2. In patients whom you clinically suspect have trichomoniasis, a culture is? a) b) c) d) Never helpful in making diagnosis More sensitive than microscopy Good for screening pregnant patients Only used in research studies Question - Vaginitis 3. In patients whom you clinically suspect have BV, a culture is? a) b) c) d) Never helpful in making diagnosis More sensitive than microscopy Good for screening pregnant patients Only used in research studies Question - Vaginitis 3. In patients whom you clinically suspect have BV, a culture is? a) b) c) d) Never helpful in making diagnosis More sensitive than microscopy Good for screening pregnant patients Only used in research studies Secrets of Women’s Language “Fine” This is used at the end of any argument that they feel they are right about but need to shut you up NEVER use FINE to describe how a woman looks This will cause you to have one of those arguments Secrets of Women’s Language “Five minutes” This a half an hour. It is equivalent to the five minutes that your football game is going to last before we take out the trash, so they feel it’s an even trade. Secrets of Women’s Language “Nothing” This means something and you should be on your toes. “Nothing” is usually used to describe the feeling a woman has of wanting to turn you inside out, upside down and backwards. “Nothing” usually signifies an argument that will last ”Five Minutes” and end with the word “Fine!”