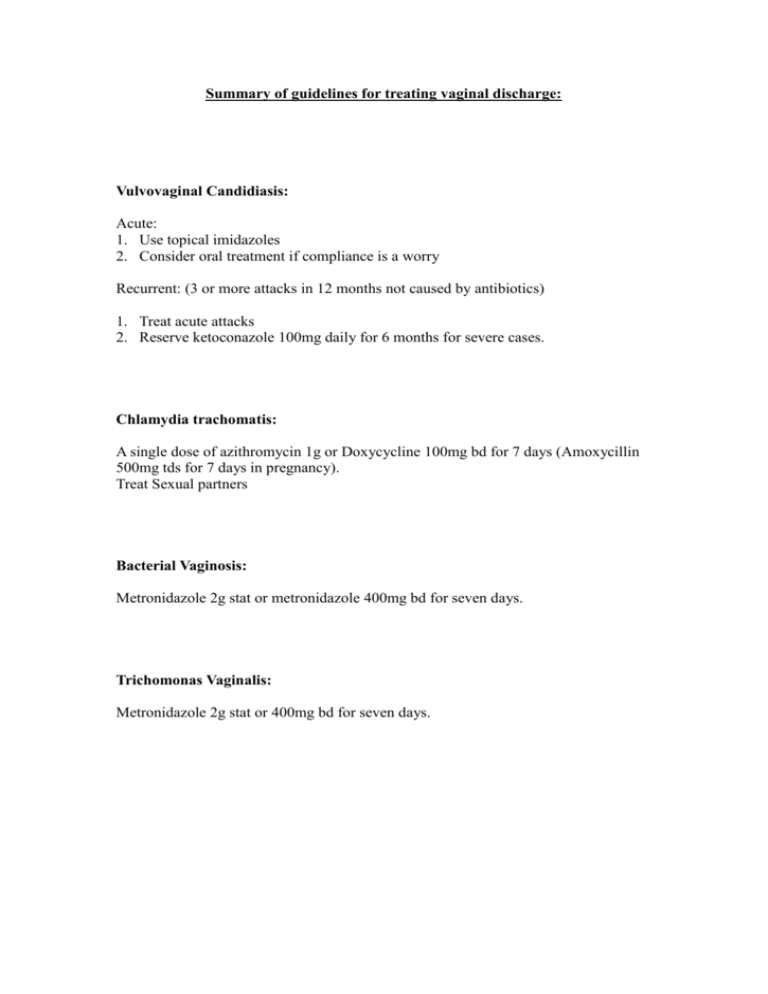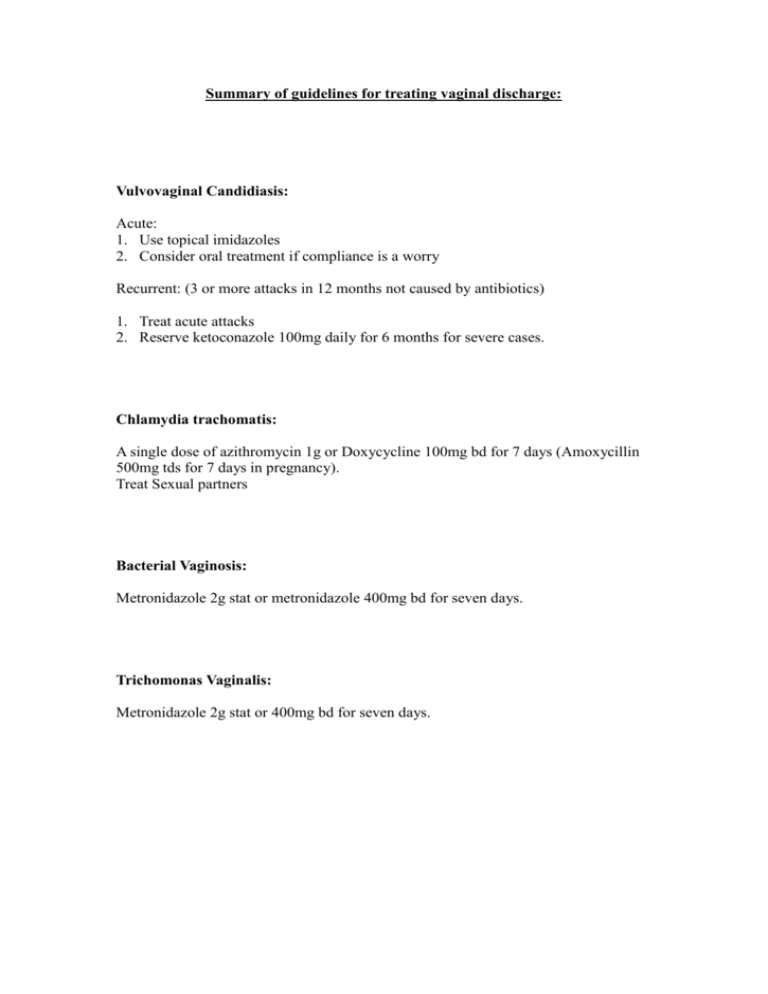
Summary of guidelines for treating vaginal discharge:
Vulvovaginal Candidiasis:
Acute:
1. Use topical imidazoles
2. Consider oral treatment if compliance is a worry
Recurrent: (3 or more attacks in 12 months not caused by antibiotics)
1. Treat acute attacks
2. Reserve ketoconazole 100mg daily for 6 months for severe cases.
Chlamydia trachomatis:
A single dose of azithromycin 1g or Doxycycline 100mg bd for 7 days (Amoxycillin
500mg tds for 7 days in pregnancy).
Treat Sexual partners
Bacterial Vaginosis:
Metronidazole 2g stat or metronidazole 400mg bd for seven days.
Trichomonas Vaginalis:
Metronidazole 2g stat or 400mg bd for seven days.
Guidelines for the management of vaginal discharge
Background
Vaginal discharge accounts for approximately 7% of all GP consultations. It may be
physiological or pathological.
Physiological discharge - comprises secretions of the Bartholin's gland and the
endocervix with cells shed from the vaginal walls. These secretions are affected by
hormonal changes during the menstrual cycle. Cervical ectropions, the intra uterine
contraceptive device and the combined oral contraceptive may increase physiological
discharge. The pre-pubertal and postmenopausal vagina, as they are not well
oestrogenised are more prone to infection.
Pathological discharge - In women of reproductive age, pathological discharge is
usually caused by infection and causative organisms may or may not be sexually
transmitted.
In pre-menarcheal girls - threadworm infestation, intra-vaginal foreign bodies or
sexually transmitted diseases can cause pathological discharge.
In post- menopausal women atrophic vaginitis predisposes to trichomonas infection
and bacterial vaginitis.
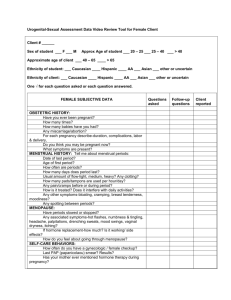
History
Patients will complain of a vaginal discharge. The history should establish the
likelihood of pathological discharge. Ask about:
the nature of the discharge (colour, smell)
associated symptoms e.g. itch
abdominal pain
associated with periods
sexual contacts
inter-menstrual or post-coital bleeding
Examination
Technique:
Pelvic examination with palpitation of vaginal nodes and inspection of the genitalia
for evidence of vulvitis, warts, infestation or ulcers.
Speculum examination with high vaginal swabs taken for trichomonas and candidiasis
and endocervical swabs for gonorrhoea and chlamydia (in sexually active women).
Vulvovaginal Candidiasis:
25% surgery visits for vaginitis
75% of women will develop vulvovaginal candidiasis at some time.
50% will have at east one recurrence.
Predisposing factors:
antibiotic use.
High oestrogen oral contraceptives
Diabetes mellitus
Pregnancy
IUCD use
HIV infection.
Acute vulvovaginal candidiasis: (Reef et al 1993)
The Imidazoles, (Clotrimazole and Miconazole) have higher cure rates than
nystatin, (80-90% compared with 70-90%) in trials comparing 14 days treatment.
Oral therapy is only as effective as topical treatment in non-pregnant women.
Oral treatment can be associated with GI symptoms and headache and there are
important interactions with drugs such as terfenadine, rifampicin and phenytoin.
Adverse reactions with the oral Imidazoles uncommon but still around 6% for
itraconazole, 10% for ketoconazole and 5-12% for fluconazole.
Ketoconazole has a risk ofidiosyncratic hepatitis of 1:15000.
Recommendations:
3. Use topical imidazoles first
4. Consider oral treatment if compliance is a worry
Acute vulvovaginal candidiasis in pregnancy: (Young and Jewell, 1995)
Imidazoles are more effective than nystatin
Treatment for 4 days is less effective than treatment for 7 days
Treatment for 7 days is no more or less effective than 14 days.
No risk of teratogenicity identified.
Minimal systemic absorption
Recommendations:
1. Use topical imidazole for seven days
Recurrent vulvovaginal candidiasis:
Uncommon, only 5% of women who get vulvovaginal candidiasis.
No identifiable risk factors.
Optimal treatment is not yet determined.
Important to establish the correct diagnosis – exclude other causes of vaginitis.
Not associated with invitro-resistance to imidazoles.
Defined as 3 attacks in 12 months not associated with antibiotic use.
Acute attacks should be treated as any other.
There is no benefit in treating sexual partners.
Prophylaxis:
Ketoconazole has been studied both as a continuous treatment and cyclical.
(Sobel, 1986, Fong et al 1993)
100mg is as effective as 200mg
100mg daily for 6 months – 95% attack free at 6 months
and 50% at 12 months
with intermittent use attack rate high after cessation of
prophylaxis and 50% recurrence within 6 months.
Clotrimazole, monthly use, attack rate slightly reduced but study only for 3
months.
Recommendations:
3. Treat acute attacks
4. Reserve ketoconazole 100mg daily for 6 months for
severe cases.
Chlamydia:
Azithromycin is as effective as Doxycycline and in a cost-effectiveness analysis
(Bandolier, [28-4]) a single dose of azithromycin 1g; even though costing 4 times
more than Doxycycline 100mg twice daily for 7 days was more cost effective because
of better compliance giving reduced pelvic inflammatory disease, pelvic pain, ectopic
pregnancy and tubal infertility. (treating chlamydia positive women with azithromycin
would save 4x as much as the additional cost.). Partners should be treated
simultaneously.
In pregnancy: (Brocklehurst and Rooney, 1996)
Amoxycillin is as effective as erythromycin in achieving microbiological cure.
Clindamycin and azithromycin may be considered further alternatives.
Further studies are required to ensure that microbiological cure with
amoxycillin translates into clinical benefit for mother and neonate.
Bacterial Vaginosis: (Drug and Therapeutics Bulletin 1998, Joesoef and Schmid,
1995)
With current treatment 50% of patients will relapse 4 weeks after treatment
Standard treatment is metronidazole orally, either 400-500mg twice daily for 7
days or 2G stat.
There is no benefit in treating the sexual partner
Intravaginal preparations of metronidazole or clindamycin appear as effective, (or
ineffective!) as oral treatments.
Bacterial vaginosis is associated with preterm birth and infective complications
following gynaecological surgery.
Pregnant women with a history of second trimester foetal loss should be screened
for bacterial vaginosis and if this is positive given oral metronidazole early in the
second trimester.
Women undergoing termination of pregnancy and known to have bacterial
vaginosis should be given metronidazole 1g rectally to prevent postoperative
infection and if testing is not available then should be given routinely.
Trichomonas Vaginalis:
Nitroimidazoles are effective in achieving short time cure (Metronidazole).
Single dose metronidazole (2G) is as effective as 400-500mg bd for 7 days.
Treat partners.
Severe symptoms may be helped by intravaginal nitroimidazoles.
Guidelines produced by:
Sheena McMain
Shirley Brearley
Rod Sutcliffe
John Potter
Steve Holmes
Adrian Dunbar
Simon Towers
June/July 1998
References:
Bandolier [28-4] Chlamydia STD treatment
Brocklehurst P, Rooney G, (1996) The treatment of genital chlamydia trachomatis
infection in pregnancy. In: Neilson J, Crowther C, Hodnett E, Hofmeyr G (Eds)
Pregnancy and childbirth module of the Cochrane Database of Systematic Reviews,
[updated 2 December 1997]. Available in the Cochrane Library [Database on disk and
CDRom]. The Cochrane Collaboration; Issue 1. Oxford: Update Software; 1998.
Updated Quarterly.
Drug and therapeutics bulletin (1998) Management of Bacterial Vaginosis. Drug and
therapeutics Bulletin; vol. 36 No 5: May 1998
Fong I, Bannatyne R and Wong P. (1992) Lack of in vitro resistance of candida
albicans to ketoconazole, itraconazole and clotrimazole in women treated for
recurrent vaginal candidiasis. Genitourinary Medicine; 69: 44-46
Joesoef M and Schmid G. (1995) Bacterial vaginosis: review of treatment options and
potential clinical indications for therapy. Clinical Infectious Diseases; 20
(supplement 1): S72-9
Reef S, Levine W, McNeil M, Fisher-Hoc S, Holmberg S, Derr A, Smith D, Sobel J,
Pinner R, (1995). Treatment options for vulvovaginal candidiasis. Clinical Infectious
Diseases; 20(supplement1): S80-S90.
Sobel J, (1986) Recurrent vulvovaginal candidiasis. N. Engl. J. Med; 315: 1455-8
Young G, Jewell M, (1995) Topical treatment for vaginal candidiasis in pregnancy. In:
Neilson J, Crowther C, Hodnett E, Hofmeyr G (Eds) Pregnancy and childbirth module
of the Cochrane Database of Systematic Reviews, [updated 2 December 1997].
Available in the Cochrane Library [Database on disk and CDRom]. The Cochrane
Collaboration; Issue 1. Oxford: Update Software; 1998. Updated Quarterly.