CERVICITIS AND VAGINITIS PREVENTION Advise patients to limit
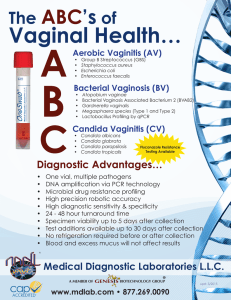
advertisement

CERVICITIS AND VAGINITIS PREVENTION • Advise patients to limit the number of sexual partners and to use barrier methods of contraception to decrease the risk for acquiring gonorrhea, chlamydia, and trichomoniasis. • Treat all sexual partners of women with gonorrhea, chlamydia, and trichomoniasis. SCREENING • All sexually active women aged 24 years or younger for chlamydia annually • Women with new or multiple sexual partners, history or current symptoms of STDs, or history of inconsistent condom use for gonorrhea and chlamydia. • Do not screen asymptomatic women for bacterial vaginosis. • Screen and treat women for bacterial vaginosis who are about to undergo gynecologic surgery. • Include a serologic screening test for syphilis in populations at high risk for syphilis. Screen pregnant women. First prenatal visit - Gonorrhea and Chlamydia - Syphilis, hepatitis B, and HIV Third trimester - Repeat Chlamydia if age 25 or younger and multiple sexual partners - Syphilis, hepatitis B, and HIV- if high risk ( use illicit drugs, have STDs during pregnancy, multiple sex partners, live in areas with high prevalence of these infections ) Treat bacterial vaginosis in symptomatic women to reduce the risk for infectious complications. Evaluate and treat pregnant women for trichomoniasis only if symptomatic DIAGNOSIS Most common cause of vaginitis symptoms - Bacterial Vaginosis (40% to 50%) - Trichomonas (15% to 20%) - Candidiasis (20% to 25%) Distinguish between vaginitis and cervicitis. • Vaginitis refers to inflammation of the vagina and is caused by infections such as candidiasis and trichomoniasis or by noninfectious conditions such as atrophic vaginitis or vaginal irritation. • Cervicitis, or cervical inflammation, is caused by different infectious diseases, including gonorrhea and chlamydia. Obtain a sexual history and inquire specifically about: • Vaginal discharge - bacterial vaginosis or trichomoniasis • “Watery” discharge helps rule out candida • Odor, including odor after intercourse - may be present in bacterial vaginosis or trichomoniasis • Irritation and pruritus may be associated with candidiasis or trichomoniasis • Dysuria • Inquire about douching, which has been associated with bacterial vaginosis. • The presence of abdominal pain or abnormal uterine bleeding may indicate upper genital tract infection. Understand that patient report of symptoms which are similar to prior yeast infection symptoms is not predictive of candida. Pelvic and abdominal exam Assess for Vulvar excoriations or vaginal lesions, which can be seen with candidiasis. Vaginal discharge and mucus from the endocervix • Candidiasis: curdy, white • Trichomoniasis: frothy, yellow, brown • Bacterial vaginitis: milky, homogenous Endocervical mucus - confirms the diagnosis of cervicitis; positive swab test is a yellow color on endocervical swab. Easily induced endocervical bleeding also may occur. Cervical motion or adnexal tenderness - indicates upper genital tract involvement - PID Lab testing Sample - vaginal walls and endocervix in all patients suspected of having vaginitis or cervicitis. - urethra for gonorrhea and chlamydia or use urine for nucleic acid amplification testing in women who have had a hysterectomy. - Vaginal pH - usually normal (<4.5) in candidiasis and high (>4.5) in bacterial vaginosis and trichomonas - “Whiff” test - fishy odor results when KOH is added to vaginal secretions( bacterial vaginosis ) - Wet mount for vaginitis and potassium hydroxide prep to visualize fungal elements - Endocervical specimen for gonorrhea and chlamydia verification for cervicitis Recognize that more than one etiologic agent may be present. CONSULTATION - Consult with a gynecologist for women with recurrent or recalcitrant vaginitis or cervicitis. - If recalcitrant trichomoniasis is suspected, choose a consultant who has access to laboratory testing, such as culture and sensitivity for T. vaginalis. - For suspected upper genital tract disease or association with systemic illness. THERAPY VAGINITIS For candida vaginitis: • Treat with topical imidazoles for 1 to 7 days, or • With single-dose oral fluconazole 150 mg • Consider treatment of sexual partners For bacterial vaginosis • Topical metronidazole for 5 days, or • Oral metronidazole, or • Topical clindamycin For trichomonas, treat with one of the following: Single-dose oral metronidazole (2 g), or Tinidazole, or Oral metronidazole for 7 days (alternative therapy) No topical treatment Treat sexual partners Consider cost and patient preference in deciding whether to use oral or intravaginal medication for yeast infections and bacterial vaginosis. CERVICITIS Consider empiric therapy at the time of initial evaluation: • For chlamydia in women aged 25 or younger or with high-risk sexual behaviors (e.g., multiple partners, unprotected intercourse) • For gonorrhea in addition to chlamydia if local prevalence is high • For both chlamydia and gonorrhea if follow-up is uncertain For gonococcal cervicitis: • Single IM injection of ceftriaxone, 250 mg • Use oral cefixime, 400 mg, as an alternative only if ceftriaxone is unavailable • Note that quinolone therapy is not recommended by the CDC to treat gonococcal disease For chlamydial cervicitis, one of the following: • Single-dose azithromycin, 1 g • Doxycycline, 100 mg, twice daily for 7 days • Note that alternative agents include erythromycin, levofloxacin, ofloxacin, and spectinomycin, 2 g intramuscularly Treat patients with gonococcal cervicitis for chlamydial infection as well, as co-infection is common. • Recommend treating sexual partners, limiting the number of sexual partners, and using barrier contraception. • Inform patients that non-drug therapies, such as povidone-iodine douches, yogurt, and vaginal acidification (Acigel), are of no benefit. • Note that probiotic therapy may be helpful in patients with bacterial vaginosis. COUNSELING Recognize that patients with an STD are at increased risk for acquiring HIV or having other complications such as tubal infertility, preterm labor, and peripartum infections. • Counsel about risks associated with STDs and how to prevent contracting them. • Encourage safer sex practices. • Provide the patient with condoms. • Offer educational brochures. • Inform patients about the American Social Health Association hotline for STD-related questions (919-361-8488). • Recommend HIV testing. • Recommend early evaluation for infertility and close obstetric follow-up. Advise patients of the importance of partner notification, and encourage the prompt treatment of partner(s). FOLLOW UP • Be aware that bacterial vaginosis is often a recurrent problem. • Be aware that, although recommended therapies should result in a cure, patients can be reinfected by an untreated sexual partner. • Consider partner noncompliance with treatment in cases of apparently refractory trichomoniasis or cervicitis. • Consider follow-up testing in situations in which compliance is in question. • Be aware that ELISAs or PCR/LCR may remain positive for several weeks after successful therapy. • Consider testing for HIV, syphilis, and hepatitis B in patients with recurrent disease (e.g., high-risk patients). • Encourage HIV counseling and testing for patients with an STD. Report all cases of gonorrhea and chlamydial infection to the state health department.