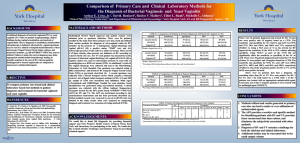
Nucleic Acid Amplification Testing (NAAT) for CT/GC
advertisement

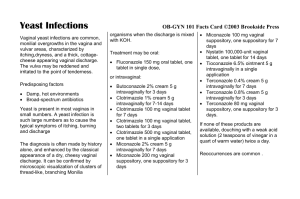
Bacterial Vaginosis, Vulvovaginal Candidiasis, and Trichomoniasis Society of Armed Forces Medical Laboratory Scientists (SAFMLS) March 28-31, 2011 New Orleans, Louisiana Richard Steece, Ph.D., D(ABMM) DrRSteece@aol.com Objectives • To describe the etiology and epidemiology of bacterial vaginosis (BV), trichomoniasis, and vulvovaginal candidiasis • To discuss the new STD Laboratory Treatment Guidelines related to of bacterial vaginosis (BV), trichomoniasis, and vulvovaginal candidiasis • To provide a summary of the current clinical and laboratory diagnostic procedures for bacterial vaginosis (BV), trichomoniasis, and vulvovaginal candidiasis Vaginitis • Vaginitis – vaginal irritation and discharge – >10 million clinic visits annually – >$500 million in health care annually • Causes of Vaginitis – Mechanical – Chemical – Infections • >90% of cases caused by 3 “agents” • >3 million clinic visits annually Vaginitis • Causes of Infectious Vaginitis – Bacterial Vaginosis (40%-45%) • Polymicrobial infection – Prevotella sp., Mobiluncus sp., Ureaplasma, Mycoplasma, and Gardnerella vaginalis • G. vaginalis as a marker, not sole etiology – Candida albicans (20%-25%) – Trichomonas vaginalis (15%-20%) Vaginitis Differentiation Normal Symptom presentation Vaginal discharge Clear to white Clinical findings Trichomoniasis Candidiasis Bacterial Vaginosis Itch, discharge, 50% asymptomatic Itch, discomfort, dysuria, thick discharge Odor, discharge, itch Frothy, gray or yellowgreen; malodorous Thick, clumpy, white “cottage cheese” Homogenous, adherent, thin, milky white; malodorous “foul fishy” Cervical petechiae “strawberry cervix” Inflammation and erythema Vaginal pH 3.8 - 4.2 > 4.5 Usually < 4.5 > 4.5 KOH “whiff” test Negative Often positive Negative Positive Lacto-bacilli Motile flagellated protozoa, many WBCs Few WBCs Clue cells (> 20%), no/few WBCs Saline wet mount KOH wet mount Pseudohyphae or spores if nonalbicans species Bacterial Vaginosis (BV) • Characterized by: – Vaginal discharge • Grey, thin homogeneous discharge – Vulvar itching – Irritation – Odor • Fishy amine odor when KOH is added to discharge: “Whiff test” Bacterial Vaginosis (BV) • Caused by: overgrowth of bacterial species normally present in the vagina with anaerobic bacteria • BV correlates with a decrease or loss of protective lactobacilli: • Vaginal acid pH normally maintained by lactobacilli through metabolism of glucose/glycogen – produce lactic acid • Hydrogen peroxide (H2O2) is produced by some Lactobacilli,sp. • H2O2 helps maintain a low pH, which inhibits bacteria overgrowth • Loss of protective lactobacilli may lead to BV Bacterial Vaginosis - Epidemiology • Most common cause of vaginitis • Prevalence varies by population: – 5%-25% among college students – 12%-61% among STD patients • Widely distributed Bacterial Vaginosis - Epidemiology • Linked to premature rupture of membranes, premature delivery and low birth-weight delivery, acquisition of HIV, development of PID, and post-operative infections after gynecological procedures • Organisms do not persist in the male urethra Bacterial Vaginosis - Epidemiology • Risk Factors – African American – Two or more sex partners in previous six months/new sex partner – Douching (prior 6 months) – Absence of or decrease in lactobacilli – Lack of H2O2-producing lactobacilli Bacterial Vaginosis - Epidemiology • Transmission – Currently not considered a sexually transmitted disease, but acquisition appears to be related to sexual activity • 15% of women with no history of sexual intercourse were + for BV Bacterial Vaginosis – Clinical Presentation and Symptoms • 50% asymptomatic • Signs/symptoms when present: – 50% report malodorous (fishy smelling) vaginal discharge – Reported more commonly after vaginal intercourse and after completion of menses Bacterial Vaginosis Associated Medical Complications • Pregnancy – Miscarriage – Premature labor and delivery – Post-caesarean delivery endometritis • Non-pregnant – PID – Increased risk of other STD’s (HIV) – Endometritis Bacterial Vaginosis – Treatment CDC - Recommended Regimens: • Metronidazole 500 mg orally twice a day for 7 days, OR • Metronidazole gel 0.75%, one full applicator (5 grams) intravaginally, once a day for 5 days, OR • Clindamycin cream 2%, one full applicator (5 grams) intravaginally at bedtime for 7 days Bacterial Vaginosis – Treatment Alternative regimens: • Tinidazole 2 g orally once daily for 2 days, OR • Tinidazole 1 g orally once daily for 5 days, OR • Clindamycin 300 mg orally twice a day for 7 days, OR • Clindamycin ovules 100 g intravaginally once at bedtime for 3 days Bacterial Vaginosis Treatment in Pregnancy • Pregnant women with symptomatic disease should be treated with – Metronidazole 500 mg orally twice a day for 7 days, OR – Metronidazole 250 mg orally three times a day for 7 days, OR – Clindamycin 300 mg orally twice a day for 7 days • Asymptomatic high-risk women (those who have previously delivered a premature infant) – Insufficient information to make recommendations at this time Bacterial Vaginosis - Diagnosis • Clinical Criteria (Amsel’s Diagnostic Criteria) Vaginal pH >4.5 Presence of >20% per HPF of "clue cells" on wet mount examination Amsel Criteria: Must have at least three of the following Positive amine or "whiff" test findings: Homogeneous, nonviscous, milky-white discharge adherent to the vaginal walls Bacterial Vaginosis - Diagnosis • Wet Prep • pH • KOH • Gram Stain (Gold Standard) – Nugent Score • Lactobacilli (i.e., long Gram-positive rods), Gramnegative and Gram-variable rods and cocci (i.e., G. vaginalis, Prevotella, Porphyromonas and peptostreptococci), and curved Gram-negative rods (i.e., Mobiluncus) Organism Scoring Per Field and Interpretation (Nugent Criteria) • • • • • • Type Number seen/OPF None <1 1-5 5-30 >30 Lac 4 3 2 1 0 GVC 0 1 2 3 4 Mob 0 1 2 3 4 BV Scored Gram Stain Method (Nugent NP. 1991. JCM. 29;297 • 0-3 = Normal • 4-6 = Intermediate – may indicate trichomoniasis, GC or CT – abnormal gram stain, but not consistent with BV • 7-10 = Consistent with Bacterial Vaginosis • Reports suggest a 89% sensitivity for BV and an 83% specificity using the scored gram stain Bacterial Vaginosis - Diagnosis • Pip Activity Test Card – Quidel • OSOM BVBlue test • Does not require Microscope • 88% sens; 95% spec vs. Nugent • 88% sens and 91% spec vs Amsel – Bradshaw, Cs et al. JCM 2005; 43: 1304-8. • Affirm VP III – Becton Dickinson – DNA Probe Vulvovaginal Candidiasis (VVC) • Characterized by: – Vulvar pruritis is most common symptom – Thick, white, curdy vaginal discharge ("cottage cheese-like“) – Erythema, irritation, occasional erythematous "satellite" lesion – External dysuria and dyspareunia – Symptoms are not specific for VVC Source: Health Canada, Sexual Health and STI Section, Clinical Slide Gallery Vulvovaginal Candidiasis (VVC) • Etiologic agent – Candida species are normal flora of the skin and vagina – VVC is caused by overgrowth of C. albicans and other non-albicans species – Yeast grows as oval budding yeast cells or as a chain of cells (pseudohyphae) – Symptomatic clinical infection occurs with excessive growth of yeast – Disruption of normal vaginal ecology or host immunity can predispose to vaginal yeast infections Vulvovaginal Candidiasis (VVC) • Candida species are normal flora of skin and vagina and are not considered to be sexually transmitted pathogens Candidiasis - Epidemiology • Affects most females during lifetime – Estimated 75% of women will have >1 episode per lifetime, 40%-45% >2 • Most cases caused by C. albicans (85%90%) • Second most common cause of vaginitis (20%-25%) • Estimated cost: $1 billion annually in the U.S. Candidiasis - Treatment • Recommended regimens • Over-the-Counter Intravaginal Agents: – – – – – – – – – • Prescription Intravaginal Agents – – – – – • Butoconazole 2% cream, 5 g intravaginally for 3 days Clotrimazole 1% cream 5 g intravaginally for 7-14 days Clotrimazole 2% cream 5 g intravaginally for 3 days Miconazole 2% cream 5 g intravaginally for 7 days Miconazole 4% cream 5 g intravaginally for 3 days Miconazole 100 mg vaginal suppository, 1 suppository for 7 days Miconazole 200 mg vaginal suppository, 1 suppository for 3 days Miconazole 1,200 mg vaginal suppository, 1 suppository for 1 day Tioconazole 6.5% ointment 5 g intravaginally in a single application Butoconazole, 2% cream(single dose bioadhesive product), 5 g intravaginally for 1 day Nystatin, 100,000 unit vaginal tablet, one tablet for 14 days Terconazole 0.4% cream 5 g intravaginally for 7 days Terconazole 0.8% cream 5 g intravaginally for 3 days Terconazole 80 mg vaginal suppository, 1 suppository for 3 days Oral agent: – Fluconazole 150 mg oral tablet, 1 tablet in a single dose Note: The creams and suppositories in this regimen are oil-based and may weaken latex condoms and diaphragms. Candidiasis - Diagnosis • Clinically – History, signs and symptoms • Direct Observation – Visualization of pseudohyphae (mycelia) and/or budding yeast (conidia) on KOH or saline wet mount – pH normal (4.0 to 4.5) • If pH > 4.5, consider concurrent BV or Trichomonas – Cultures may be useful in symptomatic women with negative wet mount – Gram Stain PMNs and Yeast Buds Saline: 40X objective Folded squamous epithelial cells PMNs Yeast buds Source: Seattle STD/HIV Prevention Training Center at the University of Washington Yeast Pseudohyphae 10% KOH: 10X objective Masses of yeast pseudohyphae Lysed squamous epithelial cell Source: Seattle STD/HIV Prevention Training Center at the University of Washington Candidiasis - Diagnosis • Clinically – History, signs and symptoms • Direct Observation – Visualization of pseudohyphae (mycelia) and/or budding yeast (conidia) on KOH or saline wet mount – pH normal (4.0 to 4.5) • If pH > 4.5, consider concurrent BV or Trichomonas – Cultures may be useful in symptomatic women with negative wet mount – Gram Stain • DNA Probe • BD Affirm VPIII Microbial ID Test Trichomonas vaginalis • Characterized by: – May be asymptomatic in women – Vaginitis • • • • Frothy gray or yellow-green vaginal discharge Strong odor Pruritus Cervical petechiae ("strawberry cervix") classic presentation, occurs in minority of cases • May also infect Skene's glands and urethra, where the organisms may not be susceptible to topical therapy Source: Claire E. Stevens/Seattle STD/HIV Prevention Training Center at the University of Washington Trichomonas vaginalis • Etiologic agent – Trichomonas vaginalis - flagellated anaerobic protozoa – Only protozoan that infects the genital tract • Possible association with – Pre-term rupture of membranes and pre-term delivery – Increased risk of HIV acquisition Trichomonas vaginalis -Epidemiology • Most common treatable STD • Estimated 7.4 million cases annually in the U.S. at a medical cost of $375 million • Estimated prevalence: – 2%-3% in the general female population – 50%-60% in female prison inmates and commercial sex workers – 18%-50% in females with vaginal complaints Trichomonas vaginalis -Epidemiology • Risk Factors – Multiple sexual partners – Lower socioeconomic status – History of STDs – Lack of condom use Trichomonas vaginalis -Epidemiology • Transmission – Almost always sexually transmitted – T. vaginalis may persist for months to years in epithelial crypts and periglandular areas – Transmission between female sex partners has been documented Trichomonas vaginalis -Epidemiology • Clinical Manifestations – May cause up to 11%-13% of nongonococcal urethritis in males – Urethral trichomoniasis has been associated with increased shedding of HIV in HIVinfected men – Frequently asymptomatic Trichomonas vaginalis - Treatment • Recommended Regimens – Metronidazole 2 g orally in a single dose OR – Tinidazole 2 g orally in a single dose Trichomonas vaginalis - Diagnosis • Direct Observation • Vaginal pH >4.5 often present • Wet Mount (50%-90%) • KOH “Wiff” Prep Trichomonas Trichomonas* Trichomonas vaginalis - Diagnosis Culture (Gold Standard – 85%-90% Sensitive) • Diamond’s, others • In-Pouch (BioMed Diagnostics) Trichomonas vaginalis - Diagnosis Point of Care Tests (POCTs) • OSOM Trichomonas Rapid Test (Genzyme) – Compared to wet mount sensitivity (94.7%), specificity (100%), positive predictive value (100%), negative predictive value (99.9%) • Campbell, et. al., J. Clin. Micro. 2008. Oct;46(10):3467-9 • XenoStrip – Tv (Xenotope Diagnostics) – Compared to wet mount 6% positive vs. 8.4% XenoStrip • Pillay et. al., J.Clin. Micro. 2004. Aug;42(8):3853-6 Trichomonas vaginalis - Diagnosis Nucleic Acid Amplification Tests (NAATs) • Gen-Probe Trichomonas Test • PCR Tests available (research sites) Trichomonas vaginalis - Diagnosis DNA Probe • BD Affirm VPIII Microbial ID Test • Trichomonas • Candida species • Gardnerella AFFIRM PROBE TECHNOLOGY • • Sample Lysis & Preparation: 10 minutes Two distinct nucleic acid probes for each organism capture probe (PAC) PAC goes in well #1 with sample color development probe (well #2) 33 minutes on instrument • Candida sp. – 1 x 10 (4) CFU/ml • Trichomonas vaginalis – 5 x 10 (3) trichomonads/ml • Gardnerella vaginalis – 2 x 10 (5) CFU/ml Reagent Casette Place Reagent Cassette On Processor & Press Run 5 3 1 2 4 6 AFFIRM VPIII vs Wet Mount N=425 AFFIRM VPIII Number POS Wet Mount Number POS Trichomonas 30 (7%) 23 (5%) Candida 45 (11%) 31 (7%) BV 190 (45%) 58 (14%) Brown HL et al. ID OBGYN 2004. 12:17-21 Why Use A Probe For Detection Of Vaginitis? • Advantages – – – – Rapidity of results Increased Sensitivity Multiple infections detected May be used in outpatient facilities – Reproducibility of testing – Less expensive than NAATs • Disadvantages – Cannot run assay for only one analyte; but we probably should look for co-infections – Few requests made to clinical laboratories: need to educate – Cost as compared to what is now done in most laboratories Summary • Infectious vaginitis is most often caused by 3 entities: – T. vaginalis – Candida sp. – Bacterial vaginosis – polymicrobial • Sexually Transmitted Diseases Treatment Guidelines, 2010 – Recommendations for treatment – http://www.cdc.gov/std/treatment/2010/default.htm • Various clinical observations/tests are available – BD Affirm is an economical, sensitive, and specific test which is able to detect all three causes of infectious vaginitis