York Hospital AFFIRM Poster CVS 2010 44x92_template
advertisement
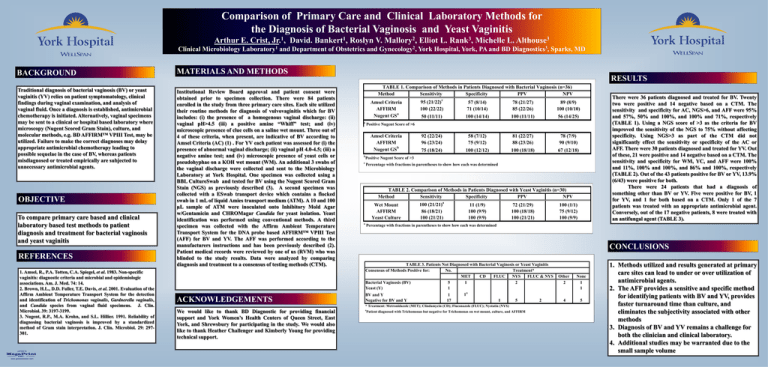
Comparison of Primary Care and Clinical Laboratory Methods for the Diagnosis of Bacterial Vaginosis and Yeast Vaginitis Arthur E. Crist, Jr.1, David. Bankert1, Roslyn V. Mallory2, Elliot L. Rank3, Michelle L. Althouse3 Clinical Microbiology Laboratory1 and Department of Obstetrics and Gynecology2, York Hospital, York, PA and BD Diagnostics3, Sparks, MD BACKGROUND Traditional diagnosis of bacterial vaginosis (BV) or yeast vaginitis (YV) relies on patient symptomatology, clinical findings during vaginal examination, and analysis of vaginal fluid. Once a diagnosis is established, antimicrobial chemotherapy is initiated. Alternatively, vaginal specimens may be sent to a clinical or hospital based laboratory where microscopy (Nugent Scored Gram Stain), culture, and molecular methods, e.g. BD AFFIRM™ VPIII Test, may be utilized. Failure to make the correct diagnoses may delay appropriate antimicrobial chemotherapy leading to possible sequelae in the case of BV, whereas patients misdiagnosed or treated empirically are subjected to unnecessary antimicrobial agents. OBJECTIVE To compare primary care based and clinical laboratory based test methods to patient diagnosis and treatment for bacterial vaginosis and yeast vaginitis REFERENCES 1. Amsel, R., P.A. Totten, C.A. Spiegel, et al. 1983. Non-specific vaginitis: diagnostic criteria and microbial and epidemiologic associations. Am. J. Med. 74: 14. 2. Brown, H.L., D.D. Fuller, T.E. Davis, et al. 2001. Evaluation of the Affirm Ambient Temperature Transport System for the detection and identification of Trichomonas vaginalis, Gardnerella vaginalis, and Candida species from vaginal fluid specimens. J. Clin. Microbiol. 39: 3197-3199. 3. Nugent, R.P., M.A. Krohn, and S.L. Hillier. 1991. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of Gram stain interpretation. J. Clin. Microbiol. 29: 297301. printed by www.postersession.com MATERIALS AND METHODS Institutional Review Board approval and patient consent were obtained prior to specimen collection. There were 84 patients enrolled in the study from three primary care sites. Each site utilized their routine methods for diagnosis of vulvovaginitis which for BV includes: (i) the presence of a homogenous vaginal discharge: (ii) vaginal pH>4.5 (iii) a positive amine “Whiff” test; and (iv) microscopic presence of clue cells on a saline wet mount. Three out of 4 of these criteria, when present, are indicative of BV according to Amsel Criteria (AC) (1) . For YV each patient was assessed for (i) the presence of abnormal vaginal discharge; (ii) vaginal pH 4.0-4.5; (iii) a negative amine test; and (iv) microscopic presence of yeast cells or pseudohyphae on a KOH wet mount (WM). An additional 3 swabs of the vaginal discharge were collected and sent to the Microbiology Laboratory at York Hospital. One specimen was collected using a BBL CultureSwab and tested for BV using the Nugent Scored Gram Stain (NGS) as previously described (3). A second specimen was collected with a ESwab transport device which contains a flocked swab in 1 mL of liquid Amies transport medium (ATM). A 10 and 100 µL sample of ATM were inoculated onto Inhibitory Mold Agar w/Gentamicin and CHROMagar Candida for yeast isolation. Yeast identification was performed using conventional methods. A third specimen was collected with the Affirm Ambient Temperature Transport System for the DNA probe based AFFIRM™ VPIII Test (AFF) for BV and YV. The AFF was performed according to the manufacturers instructions and has been previously described (2). Patient medical records were reviewed by one of us (RVM) who was blinded to the study results. Data were analyzed by comparing diagnosis and treatment to a consensus of testing methods (CTM). ACKNOWLEDGEMENTS RESULTS TABLE 1. Comparison of Methods in Patients Diagnosed with Bacterial Vaginosis (n=36) Method Sensitivity Specificity PPV NPV Amsel Criteria AFFIRM Nugent GSa a c 95 (21/22) 100 (22/22) 57 (8/14) 71 (10/14) 78 (21/27) 85 (22/26) 89 (8/9) 100 (10/10) 50 (11/11) 100 (14/14) 100 (11/11) 56 (14/25) 92 (22/24) 96 (23/24) 58 (7/12) 75 (9/12) 81 (22/27) 88 (23/26) 78 (7/9) 90 (9/10) 75 (18/24) 100 (12/12) 100 (18/18) 67 (12/18) Positive Nugent Score of >6 Amsel Criteria AFFIRM Nugent GSb b Positive Nugent Score of >3 c Percentage with fractions in parentheses to show how each was determined TABLE 2. Comparison of Methods in Patients Diagnosed with Yeast Vaginitis (n=30) Method Sensitivity Specificity PPV NPV Wet Mount AFFIRM Yeast Culture a a 100 (21/21) 86 (18/21) 100 (21/21) 11 (1/9) 100 (9/9) 100 (9/9) 72 (21/29) 100 (18/18) 100 (21/21) 100 (1/1) 75 (9/12) 100 (9/9) Percentage with fractions in parentheses to show how each was determined CONCLUSIONS TABLE 3. Patients Not Diagnosed with Bacterial Vaginosis or Yeast Vaginitis Consensus of Methods Positive for: No. Treatment* MET CD FLUC NYS FLUC & NYS Bacterial Vaginosis (BV) 5 1 2 Yeast (Y) 1 1a BV and Y 1 Negative for BV and Y 17 1 5 2 * Treatment: Metronidazole (MET); Clindamycin (CD); Fluconazole (FLUC); Nystatin (NYS) We would like to thank BD Diagnostic for providing financial support and York Women’s Health Centers of Queen Street, East York, and Shrewsbury for participating in the study. We would also like to thank Heather Challenger and Kimberly Young for providing technical support. There were 36 patients diagnosed and treated for BV. Twenty two were positive and 14 negative based on a CTM. The sensitivity and specificity for AC, NGS>6, and AFF were 95% and 57%, 50% and 100%, and 100% and 71%, respectively (TABLE 1). Using a NGS score of >3 as the criteria for BV improved the sensitivity of the NGS to 75% without affecting specificity. Using NGS>3 as part of the CTM did not significantly effect the sensitivity or specificity of the AC or AFF. There were 30 patients diagnosed and treated for YV. Out of these, 21 were positive and 14 negative based on a CTM. The sensitivity and specificity for WM, YC, and AFF were 100% and 11%, 100% and 100%, and 86% and 100%, respectively (TABLE 2). Out of the 43 patients positive for BV or YV, 13.9% (6/43) were positive for both. There were 24 patients that had a diagnosis of something other than BV or YV. Five were positive for BV, 1 for YV, and 1 for both based on a CTM. Only 1 of the 7 patients was treated with an appropriate antimicrobial agent. Conversely, out of the 17 negative patients, 8 were treated with an antifungal agent (TABLE 3). a Patient diagnosed with Trichomonas but negative for Trichomonas on wet mount, culture, and AFFIRM Other 2 None 1 1 4 5 1. Methods utilized and results generated at primary care sites can lead to under or over utilization of antimicrobial agents. 2. The AFF provides a sensitive and specific method for identifying patients with BV and YV, provides faster turnaround time than culture, and eliminates the subjectivity associated with other methods 3. Diagnosis of BV and YV remains a challenge for both the clinician and clinical laboratory. 4. Additional studies may be warranted due to the small sample volume