UNIT THREE: GYNECOLOGY
advertisement

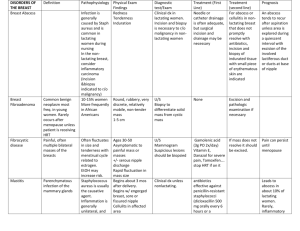
UNIT THREE: GYNECOLOGY SECTION A: GENERAL GYNECOLOGY OBJECTIVE 37: PELVIC RELAXATION AND URINARY INCONTINENCE Rationale: Patients with conditions of pelvic relaxation and urinary incontinence present in a variety of ways. The physician should be familiar with the types of pelvic relaxation and incontinence and the approach to management of these patients. The student will demonstrate knowledge of the following: A. Predisposing factors for pelvic organ prolapse and urinary incontinence B. Anatomic changes, fascial defects and neuromuscular pathophysiology C. Signs and symptoms of pelvic organ prolapse D. Physical exam 1. Cystocele 2. Rectocele 3. Enterocele 4. Vaginal vault or uterine prolapse I. Risk factors A. Vaginal delivery • Large baby • Prolonged 2nd stage of labor • Forceps • Multiparous B. Increased abdominal pressure • Obesity • Chronic constipation • Chronic lung disease C. Altered nerve function or tissue strength • Diabetes • Neurologic diseases • Aging • Collagen disorders • Hypoestrogenism • Pelvic surgery II. Anatomy A. Basic • III. Levator ani muscles • Pubococcygeuas • Puborectalis • Iliococcygeus • Viscerofascial layer • Endopelvic fascia – attaches uterus and vagina to pelvic wall • Parametria – cardinal and uterosacral ligaments B. Fascial defects C. Neuromuscular pathophysiology Signs and symptoms of pelvic organ prolapse A. Symptoms – prolapse • Asymptomatic • Vaginal pressure heaviness (>90%) • Vaginal pain • Sensation of tissue protruding from the vagina (>90%) • Abdominal pain • Low back pain • Dyspareunia/impaired coitus (37%) • Vaginal dryness • Ulceration • Bleeding • Urinary incontinence (33%) IV. V. B. Symptoms – urinary incontinence – unexpected loss of urine • Stress incontinence – involuntary loss of urine with increased abdominal pressure (valsalva, cough, laugh, sneeze) • Urge incontinence – involuntary loss of urine associated with overwhelming urge to void Physical exam (definitions) A. Cystocele • Defect where the bladder and anterior vaginal wall protrudes through the vaginal introitus • Secondary to attenuation or rupture of the pubovesical cervical fascia • Note anterior relaxation with urethral inclination • Mobility of bladder base and urethra with valsalva maneuver B. Rectocele • Protrusion of posterior vaginal wall and anterior rectal wall • Look for bulging of posterior vaginal wall with valsalva maneuver • Insert a finger in rectum and, if vaginal and rectal tissue are jauxtaposed = rectocele C. Enterocele • Elongation of posterior cul-de-sac along rectovaginal septum • 50% are diagnosed intraoperatively • Physical exam (patient standing) – palpate enterocele sac and small bowel D. Uterine/vaginal vault prolapse • Uterine – descent of uterus and cervix into the vaginal canal • Exam – patient upright, valsalva • Look and fell for prolapse • Grade based on location from hymeneal ring • Vaginal vault – loss of support of vagina beginning at apex Methods of diagnosis A. Urine culture • Rule out urinary tract infection • > 105 organisms B. Voiding diary • Normal bladder capacity (up to 60cc) • Normal frequency (<8 voids/day) • Accidents/leaking with physical activity • Amount and type of intake C. Standing stress test – note urine loss with cough or valsalva D. Q-tip test • Looks for hypermobility of the urethrovesical junction • VI. Resting position -30o or a change of greater than 30o is hypermobile E. Filling cystometrogram – examines the bladder during filling and storage • Post-void residual < 100cc • First urge - 100 – 200 mL • Maximum capacity – 400 – 500 mL • Resting bladder pressure < 10 – 15 cm of H2O F. Cystocopy Nonsurgical and surgical treatments A. Pessary • Oldest effective treatment • If pelvic floor muscle damaged, they cannot be held in place • Adjunctive treatment – estrogen B. Medications • Stress incontinence • ∂ Antagonist to increase smooth muscle tone (phenylpropanolamine) • Estrogen to increase urethral resistance • Urge incontinence – anticholinergics to decrease spasm of the detrusor muscle (oxybutynin, tolterodine) C. Pelvic floor muscle exercises • Kegels – voluntary contraction of the pelvic floor • Vaginal cones • Electrical stimulation D. Surgery • Hysterectomy – vaginal or abdominal (route depends on other surgical interventions) • For anterior wall prolapse (cystocele) • Vaginal approach - Anterior colporrhaphy (central defect) - Paravaginal repair (lateral defect) • Abdominal approach – paravaginal repair • For apical defect • Vaginal approach - Sacrospinous ligament fixation - Uterosacral colposuspension • Abdominal approach - Abdominal sacrocolpopexy - Uterosacral colposuspension • For posterior defect – posterior colporraphy • For enterocele Obliterate cul-de-sac with purse string suture in endopelvic fascia • McCall culdoplasty Colpocleisis (LeFort procedure) For stress incontinence • Vaginal approach - Pereyra - Raz - Stamey - Tensionless vaginal tape (TVT) • Abdominal approach - Marshall-Marchetti-Krantz (MMK) - Burch colposuspension • Intrinsic urethral sphincter dysfunction - Suburethral sling - Bulking injections (with collagen) to improve urethral coaptation (for patients without urethrovesical junction hypermobility) - Artificial sphincter • • • References American College of Obstetricians and Gynecologists Technical Bulletin #214. Pelvic Organ Prolapse. ACOG: Washington DC 1995. American College of Obstetricians and Gynecologists Technical Bulletin #213. Urinary Incontinence. ACOG: Washington DC 1995. Mischel DR, ed., Comprehensive Gynecology 3rd ed., Mosby, St. Louis, MO, 1997. Adapted from Association of Professors of Gynecology and Obstetrics Medical Student Educational Objectives, 7th edition, copyright 1997