X - School of Medicine
advertisement

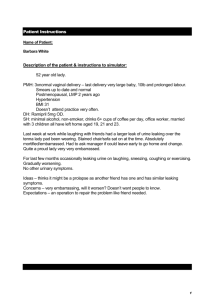
Urinary Incontinence and Pelvic Organ Prolapse UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series Division of Urogynecology/ Reconstructive Pelvic Surgery Objectives Describe normal pelvic anatomy and pelvic support Describe screening questions to elicit signs and symptoms of urinary incontinence Differentiate the types of urinary incontinence Describe the anatomic changes associated with urinary incontinence and pelvic organ prolapse Describe medical and surgical management options for urinary incontinence and pelvic organ prolapse Rationale Patients with conditions of pelvic relaxation and urinary incontinence present in a variety of ways. The physician should be familiar with the types of pelvic relaxation and incontinence and the approach to management of these patients. Definition of Urinary Incontinence International Continence Society Involuntary urine loss Severe enough to constitute a social or hygiene problem Leakage is objectively demonstrable Questions for Patients Do you leak urine when you cough, sneeze, laugh, or exercise? Do you leak on the way to the bathroom? Do you know the locations of bathrooms when you are shopping or travelling? Do you leak during intercourse? Stress or Urge Incontinence? Epidemiology Estimates of prevalence vary Bias in sample surveys Patient under-reporting Differences in definitions, populations studied and methods used ~ 13 million Americans are incontinent 10-35% of adults Economics in Urinary Incontinence Direct health care costs > $15 billion/yr Indirect health care costs Incontinence products Loss of work/productivity Classifying Urinary Incontinence Stress Loss of bladder support -> leak with cough/sneeze/valsalva Urge Overactive bladder spasms -> leak with urge Mixed Both of above Overflow Hyposensitive bladder -> leak when reach capacity Other Functional – can’t make it to bathroom (physical or cognitive impairment) Unconscious or Reflex – hyperreflexia of detrusor Fistula – tract between bladder and vagina Tenants of Effective Management Assessment of patient Risk factors and reversible causes Treatment of reversible conditions Education Treatment options QOL improvement Management plan Risk Factors Gender Immobility Environmental Barriers Altered Cognition & Delirium Medications Smoking Collagen Disorders Neurologic Disease Diabetes Stroke Menopause Childbirth Increased Abd Pressure Obesity Chronic Constipation Chronic Cough High Impact Physical Activity Patient Evaluation History Physical Exam Laboratory Tests Urodynamic Testing Voiding Diary History HPI Mental Status Evaluation Functional Assessment Environmental Assessment Social Factors Voiding Diary HPI # Incontinent episodes Triggers Stress +/- Urge Volume of urine loss Difficulty starting stream (hesitancy) Sensation of incomplete emptying Straining to empty Number of pads/day Frequency Urgency Nocturia Enuresis Dysuria Hematuria Post-void dribbling* *Sign of what? PMH Parity Birth trauma Length of labor, especially 2nd stage Previous gynecologic and/or incontinence surgery Back injury Medical History MS, DM, CVA, Parkinsons Medications Alpha-adrenergic Cholinergic Retention Bladder irritability Alpha-blocking Anti-cholinergic sphincter tone Retention b b b a TCA’s are both anticholinergic and alpha adrenergic Diet Caffeine Citrus Foods & Drinks Cranberry Juice! Spicy Foods Alcohol Functional and Environmental Assessment Manual Dexterity Mobility Patient toilet unaided? Access Distance to toilet or bedside commode (BSC) Chair/bed transfers Voiding Diary Date and Time Fluid consumption w/ type and volume Voiding episodes w/ volume Leaking episodes Urgency Physical Examination General GU Neurologic Direct Observation of Urine Loss Post-Void Residual Q-Tip Test Physical Examination: Gynecologic External Genitalia: excoriation, erythema Vaginal Introitus and Mucosa: caliber, atrophy Anterior Vagina: urethral diverticulum Lateral Vaginal Sidewalls Posterior Vagina Uterine or Vaginal Cuff: procidentia, prolapse Urethra: caruncle Anus and Rectum: rectal prolapse, sphincter integrity Physical Examination: Neurologic S2 - S4 Sharp and dull touch Perineum and buttocks Reflexes Bulbocavernosus Anal Wink Physical Examination: Q-tip Test Assesses bladder neck mobility Sterile technique Anesthetic gel + 30o = UVJ hypermobility SUI often has hypermobility Hypermobility not necessarily SUI - 20o Urodynamics Uroflowmetry Cystometrogram Leak Testing Electromyography Micturition Study Urethral Pressure Profile Videocystourethrography Cystoscopy Urodynamics Male or Female? Laboratory Testing Urinalysis and Culture Bacterial mucosal irritation Unsuppresible detrusor activity Endotoxin inhibition of alpha-adrenergic receptors in urethra Treatment Options Treating Reversible Conditions Behavioral Therapy Medications Devices Surgical Reversible Conditions UTI Atrophic urethritis/vaginitis Stool Impaction Dietary Medications Inadequate/Excess fluid intake How many mL/day? Reversible Conditions Delirium Psychological Restricted Mobility Treatment: Detrusor Overactivity Dietary Toileting Habits Scheduled Toileting +/- BSC Urge Strategies Pelvic Muscle Exercises Biofeedback Electrical Stimulation Treatment: Detrusor Overactivity Bladder has muscarinic receptors (M3) Medications Ditropan Detrol Sanctura Vesicare Enablex Imipramine Side Effects Dry mouth Dry eyes Constipation Cognitive dysfunction Surgical Treatment: Detrusor Overactivity Refractory cases InterStim Device Percutaneous Tibial Nerve Stim (PTNS) Augmentation Cystoplasty Many associated complications Last resort procedure Treatment: Stress Incontinence Burch Retropubic Urethropexy Pubovaginal Sling Mesh or Fascial Urethral Bulking Transurethral injection Non-Surgical Treatment: Stress Incontinence PESSARY Low morbidity Requires regular care Managed by patient Fem-Soft When to Refer? Failed trial of conservative therapy Pronounced anatomic defect Persistent infection Desire or need for surgery Associated problems Bottom Line Concepts Insert other bottom line concepts here. Investigation of the incontinent patient History Physical Exam Urinalysis and Culture +/- Urodynamic Testing Despite high prevalence and cost, less than 50% of people with urinary incontinence seek help! So ASK your patients about it! Definition: Prolapse ANTERIOR Anterior Wall Defect AKA Cystocele POSTERIOR Posterior Wall Defect AKA Rectocele Small Bowel Herniation AKA Enterocele LATERAL WALLS Paravaginal Defect APICAL Uterine Prolapse Vaginal Vault Prolapse Etiology Childbirth Increased Intra-abd Pressure Lifting Coughing Obesity Constipation/Straining Neurologic Injury Genetic Predisposition Connective Tissue Abnormalities Estrogen Deficiency Normal Pelvic Anatomy What is Prolapse? - loss of support of vaginal walls Vesicovaginal septum Rectovaginal septum Symptoms of Prolapse Pressure Bulging Vaginal irritation/Ulcers PAIN IS NOT A PRESENTING SYMPTOM Compartment-Specific Prolapse Symptoms ANTERIOR Stress urinary incontinence Incomplete bladder emptying Possible increased frequency of UTIs POSTERIOR Incomplete stool evacuation Splinting to assist defecation Consequence of Prolapse Prolapse Diagnosis: Pop Q Prolapse Therapy Conservative Therapy Pelvic Floor Muscle Exercises Pessary Surgical Therapy Based on location of prolapse Anterior, Posterior, Apical, Uterine Pelvic Organ Prolapse Repair Anterior Compartment Weakness of vesicovaginal septum Pelvic Organ Prolapse Repair Anterior Colporrhaphy Reinforcement and repair of vesico-vaginal supportive tissue Non-permanent plication sutures Pelvic Organ Prolapse Repair Posterior Compartment Weakness of rectovaginal septum Denonvillier’s “fascia” Pelvic Organ Prolapse Repair Posterior Colporrhaphy Reinforcement and repair of rectovaginal septum Non-permanent plication sutures Pelvic Organ Prolapse Repair Lateral Compartments Detachment of lateral walls of vagina from Arcus Tendinius Fascia Pelvis “White line” Pelvic Organ Prolapse Repair Lateral Compartments Reattachment of vaginal supportive tissue to white line Pelvic Organ Prolapse Repair Apical Compartment Uterosacral ligaments to … Uterus/cervix Vaginal cuff Cervical Os Pelvic Organ Prolapse Repair Apical Compartment Attachment of uterosacral ligaments to vaginal cuff Pelvic Organ Prolapse Repair Apical Compartment Attachment of vaginal cuff to anterior longitudinal sacral ligament using a graft Sacrum Vagina Robotic Sacrocolpopexy Apical Compartment Robotically-Assisted Laparoscopy da Vinci® surgical system Approved in 2005 Hysterectomy Myomectomy Sacrocolpopexy Questions? Bottom Line Concepts Many types of Urinary Incontinence Stress Urge Mixed Overflow Other Functional Unconscious or Reflex Fistula Treatments include Diet Medication Biofeedback Pessary Surgery Bottom Line Concepts Prolapse is associated with pressure, but not pain Site-specific exam Assess each compartment – anterior, posterior, apical, uterine Use Q-tip and speculum to identify specific prolapse Site-specific approach to repair Anterior, posterior, apical, uterine Treatment focused on symptom improvement, not anatomical correction References and Resources APGO Medical Student Educational Objectives, 9th edition, (2009), Educational Topic 37 (p78-79). Beckman & Ling: Obstetrics and Gynecology, 6th edition, (2010), Charles RB Beckmann, Frank W Ling, Barabara M Barzansky, William NP Herbert, Douglas W Laube, Roger P Smith. Chapter 28 (p259-268). Hacker & Moore: Hacker and Moore's Essentials of Obstetrics and Gynecology, 5th edition (2009), Neville F Hacker, Joseph C Gambone, Calvin J Hobel. Chapter 23 (p276-289).