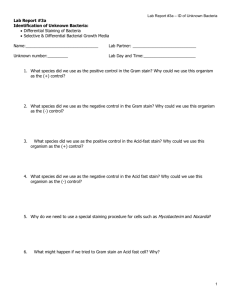
GRAM STAIN REAGENT TEST KIT
advertisement

GRAM STAIN REAGENT TEST KIT FOR THE DIFFERENTIAL STAINING OF BACTERIA IN PRIMARY SPECIMENS AND FROM CULTURE INTENDED USE The Curtiss Gram Stain Reagents and kits are recommended for the differential staining bacteria in primary specimens and from culture. SUMMARY AND EXPLANATION The Gram stain is well established as an important aid in the differentiation and identification of isolated microorganisms. A correctly performed and interpreted Gram stain of certain clinical specimens also can be a rapid source of presumptive diagnostic information. Numerous studies and reports have established the value and importance of this technique in the examination of sputum and transtracheal specimens, cerebrospinal and other normally sterile body fluids, uncontaminated abscess fluids and specimens from cerebrospinal and other normally sterile body fluids, uncontaminated abscess fluids and specimens from soft tissue infections, and exudates from the male urethra,1-6 The gram stain examination of uncentrifuged urine also is a procedure recommended to provide rapid preliminary information. 7 Gram stain examinations should not be used, however, as a substitute for complete and careful culture studies. The basic principle of the differential Gram stain was discovered serendipitously by Christian Gram in 1883.8 Since then, this process has been exhaustively investigated and refined.8-11 In Practice, a thin smear of bacterial cells is stained with crystal violet, then treated with an iodine-containing mordant to increase or intensify binding of this primary stain. A decolorizing solution of alcohol (or acetone or a combination thereof) is used to remove the crystal violet from cells which bind to it weakly, and a saffranin counter stain is used to provide a color contrast in those cells which were decolorized. In a properly stained smear, gram-positive cells appear blue to purple and gram-negative cells appear pink to red. PRINCIPLES OF THE PROCEDURE A variety of mechanisms have been proposed to explain the Gram reaction, but its underlying basis is still incompletely understood. There are a variety of physio-clinical differences between grampositive and gram-negative cell walls12 and cell wall permeability may be involved in the differentially retention of the crystal violet iodine complex.13 Gram reactivity also may depend upon or be influenced by the presence or absence of specific chemical compounds in the bacterial cell wall. Gram-positive cells can be made to stain gram-negative by extraction of a variety of substances, including nucleoprotein, ribonucleic acid, and polysaccharide. 14 REAGENTS Formula: Curtiss Gram Crystal Violet Solution: Gram Primary Stain, approximately 0.4% crystal violet in an aqueous alcohol solution. Curtiss Gram Iodine Solution: Approximately 0.33% elemaental iodine in 0.66% aqueous potassium iodine solution. Curtiss Gram Decolorizer Solution: Gram Stain Decolorizer, denaturedethyl alcohol and acetone, approximately three parts to one part, respectively. Curtiss Gram Safranin Solution: Counterstain, approximately 0.25% safranin in 20% ethyl alcohol. PRECAUTIONS: For In Vitro Diagnostic Use As with all techniques involving pathogenic and potentially pathogenic microorganisms, established aseptic practices should be consistently applied throughout this procedure. These reagents are harmful or fatal if swallowed and can cause eye irritation if contact is made. In the event of eye contact, flush eyes with an eye wash system or tap water for 15 minutes. Gram decolorizer solution is flammable and its vapors may be harmful, use in a well ventilated area away from open flame. Storage Instructions: On receipt, store at 15º-30ºC. The expiration date is for product in unopened bottles stored as directed. Do not open until ready to use. Product Deterioration. Some precipitation may occur in the crystal violet solution upon prolonged storage. If this appears to affect the quality of the staining, with the dispensing closure open, briefly warm the bottle or quantities, dispensed into the bottle 37ºC water bath, then close and shake until the precipitate is dissolved. The Gram Iodine Solution deteriorates especially when exposed to light and/or heat. Solution remain stable until expiration date on the bottle. It should be discarded when color loss becomes significant or when adequate results are no longer obtained (see “User Quality Control”). SPECIMEN COLLECTION AND PREPARATION The Gram Stain may be performed on smears prepared from clinical specimens or samples containing missed flora or pure cultures or on smears of microbial growth from laboratory cultures. PROCEDURE Materials Not Provided: 1. Clean microscope slide 2. Inoculating loop or needle or swabs 3. Water or saline 4. Bunsen burner 5. Blotting Paper 6. Microscope INSTRUCTIONS FOR PERFORMING THE GRAM STAIN 1. All solutions are used as presented. 2. Prepare a thin, evenly distributed smear of the material to be Gram-stained, Note: in very thick smears, decolorixation cannot be adequately evaluated or controlled: very thin smears are easily over-decolorized. 3. Clinical specimens and bacteria growing in broth culture can be applied directly to a microscope slide with a swab or inoculating loop. 4. Growth from bacterial colonies can be picked with an inoculating loop or needle and emulsified in a drop of saline or water placed on the slide. 5. Aloe the smear to completely air-dry without heat, and the heat-fix quickly passing the slide through the (low) flame of a Bunsen burner 2-3 times (the slide should be just hot to the touch for correct smear fixation; if exposed to excess heat, bacteria may not stain properly). 6. Cover the smear with crystal violet solution and allow the stain to act approximately one minute. 7. Remove excess stain by briefly rinsing the slide with tap water. 8. Shake off the excess water, flood the smear with Iodine Solution, and allow to stand for one minute or longer. 9. Rinse off the iodine solution with tap water and carefully apply decolorizer solution just until no more color is being washed from the smear. Quickly rinse off any remaining decolorizer with tap water. Note: Do not Over-Decolorize. 10. Shake off any excess water and apply the safranin for approximately one minute. 11. Wash slide in tap water, blot dry, and examine microscopically. User Quality Control: As a test of both reagent integrity and correct reading and staining technique, the daily performance of quality control is recommended. This is especially important when clinical specimens are being examined to provide presumptive diagnostic information or a guide for antimicrobial therapy. Overnight 18-24 (h) cultures of Escherichia coli (gram-negative) and Staphylococcus aureaus (gram-positive) are suitable control organisms. More subtle deficiencies in reagent quality and techniques can be detected by the use of weakly reactive bacteria such as Bacillus subtitis (gram-positive) and Moraxella (Branhamella) catarrhalis (gram-negative)15 RESULTS When the differential Gram procedure is performed correctly, organisms which retain the primary stain-mordant complex will appear microscopically blue to purple and are termed “grampositive”, organisms which are decolorized and therefore take up the counterstain, microscopically will appear pink to red and are termed “gram-negative”. LIMITATIONS OF THE PROCEDURE Gram reactivity is not an absolute characteristic and is influenced by several factors. The age of a culture affects its degree of Gram positivity, in general, cells from young actively-growing cultures retain the crystal violet-iodine complex more avidly than cells from older cultures. Although the optimum age for staining may vary from species to species.16 It is general practice to examine 18-24-h cultures. When experience or special conditions dictate, younger or older cultures also should be tested. Different species of bacteria may not be equally sensitive to deleterious effects of heat-fixation, but over-heating, because it may cause gram-positive bacteria to stain gram-negative, should be avoided. AQntimicrobial agents also may make gram-positive organisms more susceptible to decolorization17.18 this fact should be kept in mind when examining clinical specimens, especially from treated patients. The Gram stain should be used only to provide supplementary diagnosis or taxonomic information; it is not intended, and should not be used, as a substitute for more comprehensive tests. REFERENCES 1. Spengler, M.S., G.T.Rodeheaver, L. Righter, M.T.Egerton, and R.F.Edlich, 1978. The Gram Stain-The most important test of infection. J.Am.College Emergency Physicians, 7:434 -438. 2. Washington, J.A. 1979. Use and Abuse of the Gram-Stained smear. Clin.Microbiol.Newsl. 1:4-5. 3. Riles,K., M.E.Levinson and D.Kaye. 1975 Transtrachael aspiration in pulmonary infection. Arch.Interm,Med. 133:453458. 4. Heineman, H.S., J.K.Chawla and W.M.Lofton. 1977. Misinformation from sputum cultures without microscopic examination. J.Clin.Microbiol, 6:518-527. 5. Marshall, K.A., M.T.Egerton and G.T.Rodeheaver, 1976.Quantitative Mirobiology: ites application to hand injuries. Am.J.Surg. 131:730-733. 6. Jacobs, N.F., and S.J.Kraus, 1975. Gonococcal and nongonococcal urethritis in men. Clinical and laboratory differentiation.Ann.Interm.Med. 82:7-12. 7. Barry, A.L.,P.B.Smityh and M.Turck. 1975. Cumitech 2, Laboratory diagnosis of urinary tract infections. Coordinating ed., T.L.Gavan. American Society for Microbiology, Washington, D.C. 8. Bartholomew,J. T.Mittwer. 1952. The Gram Stain. Bacteriol.Rev.16:1-28. 9. Mittwer, T., J.W.Bartholomew and B.J.Kallman. 1950. The Mechanism of the Gram Reaction, II. Stain Technol. 25:169179. 10. Bartholomew, J.W. and T.Mittwer. 1951. The Mechanism of the Gram reaction, III. Stain Technol. 26:231-240. 11. Hendrickson, D.A., and M.M.Krenz. 1991. Reagents and Stains, p.1289-1314. In A.Balows, W.J.Hausler, Jr., K.L.Hermann, H.D.Isenberg and H.J.Shadomy (ed), Manual of Clinical Biology, 5th ed. American Soc. For Microbiol., Wash. D.C. 12. Lamanna, C., and M.F.Mallette. 1965. Basic bacteriology, 3rd ed., p.162-176. The Williams & Wilkins Co., Baltimore. 13. Salton, M.R.J., 1964. The Bacterial cell wall, p.29-36. 14. 15. 16. 17. 18. Elsevier, Amsterdam. Biswas, B.B., P.S.Basu and M.K.Pal. 1970. Gram Staining and its molecular mechanism. Int. Rev. Cytol 29:1-27. Russell, R.L. 1974. Quality Control in the Microbiology laboratory, p.866. In E.H.Lennette, E.H.Spaulding and J.P.Truant (ed), Manual of Clinical Microbiology, 2nd. Ed. American Society for Microbiology, Washington, D.C. Hucker, G.J., and H.J.Conn. 1927. Further studies on the methods of Gram Staining. N.Y. (Geneva) Agr.Exp. Tech.Bull. 128:1-34. Dufrenoy, J., and R.Pratt. 1947. Cytochemical mechanisms of penicillin action. J.Bacteriol. 54:283-289. Catlin, B.W. 1975. Cellular elongation under the influence of antibacterial agents: way to differentiate coccobacilli from cocci. J.Clin.Microbiol. 1:102-105. WARRANTY Curtiss makes no warranty of any kind, either expressed or implied, except that the material from which its products are made are of standard quality. If any materials are defected, Curtiss will provide a replacement product. Buyer assumes all risk and liability resulting from the use of this product. There is no warranty of merchantability of this product, or of the fitness of the product for any purpose. Curtiss shall not be liable for any damages, including special or consequential damage, or expense arising directly or indirectly from the use of this product.