24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
ALS Treatment
ALS Medical Team………………………………….……
33
Drugs and Supplements…….………..………….……….
36
Managing Depression…….……………………….……..
38
Muscle Spasms…………….…………………….………
40
Constipation……………….……………………….….…
43
Managing Neck Muscle Weakness….………………..…
46
Range of Motion Exercises…………………….….…….
52
Managing Saliva ………………………………………..
61
Swallowing Problems (Dysphagia)……………………..
64
Strategies for Safer Swallowing………………..………
67
About Feeding Tubes……………………………………
70
BiPap/Ventilation………………..……………………….
78
32
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
The ALS Medical Team
Living with ALS is a challenge for patients and families, however, there are ways to make living
with ALS easier and be able to manage the symptoms related to the disease. It is very important to
meet with health care professionals who specialize in the field of ALS. The team is made up of
physicians and allied health professionals who work together to meet the needs of patients and
families living with ALS. They work to streamline the referral process; share information with
other agencies and healthcare personnel; communicate and work with primary care physicians, case
managers, and insurance companies to ensure comprehensive care; research treatments and
procedures to find the best options for treating the symptoms of ALS; and participate in drug trials
and research. The following are the disciplines that participate at the ALS Center.
•
•
•
•
•
•
•
•
Physical therapy
Occupational therapy
Respiratory therapy
Nursing
Registered dietitian services
Ph.D. psychology or psychiatry
Speech and language pathology
MSW social work services
Description of ALS Medical Team Specialties
Neurologist - The initial role of the neurologist is the medical evaluation of the patient and
diagnosis or confirmation of diagnosis. Subsequently the neurologist becomes the key ALS team
contact and monitors clinical function, initiates treatment programs as needed, and provides overall
support to the patient and family. Information is provided regarding the latest developments in ALS
research and the patient is offered the opportunity to participate in clinical research trials if specific
entry criteria are met
Nurse - A nurse coordinator is the main contact between the different ALS team members and the
patients and their families. The nurse also provides a multitude of services, including monitoring of
vital signs and weight, maintaining the medical records for each clinic visit, assessing general health
problems and providing practical solutions, and testing functional changes in the patient's clinical
status. In addition, research nurses coordinate the different clinical drug studies for patients
attending the clinic.
Pulmonologist - The role of the pulmonologist is to carefully evaluate respiratory status and initiate
prompt intervention to treat respiratory dysfunction when needed. This includes monitoring
33
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
respiratory function and capacity and the corresponding blood oxygen and carbon dioxide levels.
This may include a cessation of smoking program, instruction in maintaining nutrition and
prevention of aspiration, flu and pneumonia vaccinations, introduction of respiratory support (bipap
or ventilation) and medications to decrease the work of breathing. If oral secretions become
excessive, drugs that decrease saliva production or suction devices to remove secretions may also be
prescribed.
Respiratory Therapist - The role of the respiratory therapist is to obtain measurements of
respiratory function and instruct the ALS patient and family in the use of therapeutic measures such
as breathing exercises and assistive coughing and in the use of equipment prescribed by the
pulmonologist.
Physical Therapist - The role of the physical therapist is to assist the patient in the areas of
exercise, equipment, and safety. This includes patient and caregiver instruction in stretching and
range of motion exercises to help maintain flexibility and reduce cramping. The physical therapist
may also recommend devices and equipment such as an ankle-foot-orthosis, a cane, a wheelchair, a
neck brace to help in maintaining mobility and independence. Instruction in proper methods for
moving, transferring and lifting patients and recommendations for safety equipment including aids
for transfers, lifts, grab bars and shower chairs are also provided. The goal is to promote the highest
level of possible function, for as long as possible while avoiding fatigue.
Occupational Therapist - The role of the occupational therapist is to provide the ALS patient with
options, resources, and information for maintaining independence in activities of daily living. The
occupational therapist assesses the patient's functional abilities (range of motion, muscle strength,
daily activity levels, and mobility) and performance in activity areas such as dressing, feeding,
hygiene, and in the work environment. Adaptive devices such as rocker knives, button hooks,
handwriting aids, book holders, zipper pulls, key holders, reachers and grab bars may be
recommended to assist weakened muscles, reduce fatigue, promote safety, and enhance life quality.
Speech Pathologist - The role of the speech pathologist is to assess the ALS patient’s speech and
communication skills, implement strategies to enhance communication, provide patient/family and
assure that ALS patients can express their feelings, thoughts, and needs. If there is muscle weakness
in the lips, tongue, or palate, the patient may not be able to move their mouth precisely or fast
enough, which results in slurred speech. Instruction in the use of compensatory strategies (such as
slowing the rate of speech, separating the syllables, and over-enunciating the speech sounds) can be
helpful. These strategies can also be augmented by communication devices such as magic writing
slates, alphabet boards, picture boards, eye scanning boards, electronic devices with voice output,
and even high-tech computerized devices.
Social Worker - The role of the social worker is to assess the impact of recent physical, emotional,
and financial changes in the patient with ALS and how the patient and family are coping. Current
and future needs are addressed, as well as the personal and community resources that may be
available to help meet those needs.
34
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Psychologist - The role of the psychologist is to assess and address coping strategies, signs of
depression, maladaptive means of coping, communication style, quality of relationships, and the
nature of family dynamics. A diagnosis of ALS changes everything not only for the patient, but for
family and friends. The goal of the psychologist is not to change people, but to meet them where
they are in the adaptation process, provide a supportive relationship and assist them in finding
internal resources to help in coping with ALS. Successful coping strategies include the ability to
articulate needs and wants, the willingness to share feelings with others, the ability to be a good
listener, and the openness to look at new ways of communicating with loved ones and health
professionals.
Dietitian - The role of the dietitian is to devise an individual program to provide adequate nutrients
in the context of the patient's swallowing ability. ALS may cause weakness of the muscles involved
in chewing and swallowing, which can result in coughing and choking episodes. The objective is to
provide adequate nutrients while preventing aspiration of food or liquids into the lungs, which could
lead to infection and pneumonia. This is typically accomplished by modifying the consistency and
texture of foods and liquids or by recommending the use of alternative feeding methods.
Gastroenterologist - The role of the gastroenterologist (an expert in the stomach, intestines and
colon) is to provide support of the ALS patient regarding problems associated with the digestive
system. This specialist is typically consulted as swallowing problems result in the need to consider
a feeding tube.
35
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Drugs and Supplements
Treatment of ALS is primarily a process of managing symptoms. As PALS get weaker, their
symptoms change, their needs change, and consequently their treatments are always being modified.
Treatment involves managing ALS symptoms through drugs, therapies, nutrition, dietary
supplements, and adaptive equipment. Before taking medication, vitamins, or supplements patients
should always speak with their neurologist.
FDA approved drugs to slow ALS progression
Rilutek (available by prescription) is the only drug approved by the Food and Drug Administration
for treatment of ALS patients. Two randomized and placebo-controlled trials performed in both
Europe and North America found a difference of about 2 to 3 months in the time to tracheostomy or
death in favor of patients treated with Rilutek as compared to those receiving placebo. However,
there was no statistical significant difference in mortality at the end of the trial. Measures of muscle
strength and neurological function did not show improvement. Potential side-effects include fatigue,
nausea, dizziness, diarrhea, anorexia, vertigo, and somnolence. While the effect of Rilutek is
modest, it is a significant development in that it is the first ALS drug proven to be effective in over
130 years of research. Because the effect is modest, one must weigh the financial cost versus the
benefit when electing to use Rilutek. Rilutek is expensive, over $800 for a 30 day supply, but it is
covered under most health insurance policies. The National Organization for Rare Disorders
(NORD) may be able to assist you with purchasing Rilutek if you do not have insurance.
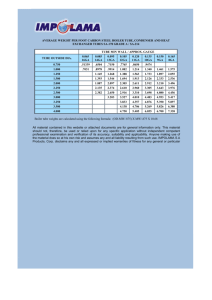
Prescription and OTC Drugs for ALS Symptoms
Condition
Spasticity (stiffness)
Potential Treatment Drugs - Generic (Brand Name)
Baclofen (Lioresal), Tizanidine (Zanaflex), Memantine,
Tetrazepam, Carisoprodol (Soma), Dantrolene, Marinol
Fasciculations (twitching) and Quinine Sulfate, Baclofen (Lioresal), Clonazepam (Klonopin),
Muscle Cramping
Carbamazepine (Tegretol), Phenytoin (Dilantin), Magnesium,
Verapamil (Calan)
Depression
Fluoxetine (Prozac), Sertraline (Zoloft), Paroxetine (Paxil),
Amitriptylene (Elavil), Imipramine (Tofranil), Nortriptyline
(Pamelor), Fluvoxamine (Luvox)
Pseudobulbar Emotionalism
(excessive laughing/crying)
Amitriptylene (Elavil), Fluvoxamine (Luvox), Lithium; LDOPA
Gastric Reflux (heartburn)
Pepcid, Ranitidane (Zantac)
Thick Phlegm (mucus)
Guaifenesin, Robitussen, Propranolol (Inderal), Metoprolol
(Toprol)
36
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Condition
Sialorrhea (drooling or
excessive salivation)
Potential Treatment Drugs - Generic (Brand Name)
Amitriptylene (Elavil), Trihexyphenidyl Hydrochloride
(Artane), Clonidine (Catapres), Propantheline (Pro-Banthine),
Benztropine (Cogentin), Glycapyrrolate (Robinul), Transdermal
Hyoscine (Scopolamine), Benadryl, Atropine (Sal-Tropine)
Bulk-forming fiber laxative (FiberCon, Citrucel, Metamucil,
etc.), Docusate Sodium (Correctol, Colace, Dulcolax),
Lactulose (Constulose, Duphalac, Chronulac, Constilac)
Toterodine (Detrol)
Flu vaccine, Pneumonia vaccine
Morphine (Roxanol), Lorazepam (Ativan), Midazolam
(Versed)
Constipation
Urinary Urgency
Breathing (early stages)
Breathing (latter stages)
Drugs/Supplements Commonly Taken by ALS Patients
Vitamin E
Vitamin
Vitamin C
Vitamin
Rilutek
Prescription Drug
Creatine
Supplement
CoEnzyme Q10
Supplement
Vitamin A / Betacarotene
Vitamin
Vitamin B Complex
Vitamin
Grape Seed Extract
Supplement
Vitamin B12
Vitamin
Alpha Lipoic Acid
Supplement
Selenium
Supplement
Zinc
Supplement
Ginko Biloba
Supplement
OPC / Pyncogenol
Supplement
Magnesium
Supplement
NAC
Supplement
DHEA
Supplement
Melatonin
Supplement
Ginseng
Supplement
37
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Managing Depression in ALS
By Pamela A. Cazzolli, R.N.
People with amyotrophic lateral sclerosis (ALS) face ongoing changes and losses as the disease
progresses, resulting in unavoidable grief and depression. Struck by shock and disbelief at first,
awareness of losses eventually becomes a reality. Some persons are overwhelmed by thoughts that
life will never be the same, thoughts that may lead to hopelessness, helplessness and despair.
Grief and depression are normal reactions to functions that are permanently lost. Each new loss is
usually experienced as a first. Sadness and crying commonly follow awareness of changes.
Although ALS individuals may perceive that crying is a loss of control or weakness, crying is a
therapeutic strategy, an important emotional release. Grieving allows one to “let go” of what can no
longer be. Lingering grief and depression, however, can lead to chronic sorrow, a pervasive sadness
that never goes away.
Because depression can slow body movement, producing fatigue (similar to symptoms of ALS),
signs of depression may by overlooked. If undetected, depression will remain unmanaged,
compounding life’s misery. Furthermore, depression is like a contagious disease, infecting an entire
household. By recognizing signs of depression, strategies can be implemented for alleviating
unbearable grief, enhancing the ability to adapt to losses.
Common signs of depression include: loss of energy, disinterest in activities, lack of desire to
interact with family and friends, wishing not to be bothered, crying spells, slowed thinking,
forgetfulness, difficulty concentrating and making decisions, sleep disturbances, unkempt
appearance and loss of appetite.
Signs of severe depression include: staring into space for long periods, no desire to do anything,
communicating only to answer a question, poor concentration or memory, confusion, refusal to eat,
weight loss, gastric disturbances, difficulty sleeping or excessive sleep, feeling that there is no
reason to go on living and thoughts of suicide.
STRATEGIES FOR MANAGING DEPRESSION:
1.
Express your feelings. Talking about losses is very important in working through grief
precipitated by loss. If speech is impaired, find an effective means of communication.
2.
Focus on your abilities rather than your disabilities. Use assistive devices to enhance
mobility. Do not resist a wheelchair if needed. Modify your home environment for easier
accessibility.
3.
Set new goals that are achievable. Maintain a purpose in living, despite physical limitations.
38
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
4.
Have something to do and to look forward to everyday. Keep your mind busy. Plan for
pleasurable experiences and achievements.
5.
Maintain social interaction with others. Avoid loneliness. Plan enjoyable activities with
family or friends. Find accessible methods for leaving your home, going in and out of your
vehicle, and visiting others. If traveling is difficult, encourage family and friends to visit with
you at home.
6.
Maintain control of your life and decision-making. Being in control reduces feelings of
powerlessness and helps to prevent giving up.
7.
Strive to maintain a positive self-concept. Getting dressed daily and looking one’s best can
help people to overcome a negative self-image.
8.
Seek spiritual care. Faith in God, scriptural meditation and prayer provide peace of mind,
joy and hope for tomorrow, despite trials and tribulations.
Signs of unresolved depression may warrant treatment or professional counseling. Seek help if
needed. By understanding strategies that may assist in adjusting to loss, people with ALS may help
overcome agonizing grief and depression. The goal is to change from focusing on what was lost in
the past to focusing on what is here to enjoy now and the days ahead.
Revised: August 2000
© 2000. Pamela A. Cazzolli, R.N., Canton, Ohio USA. All Rights Reserved.
Reprinted with permission by Pamela A. Cazzolli, R.N., ALS Nurse Consultant in Canton, OH.
39
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Muscle Spasms
By PALS Diane Huberty, CNRN
(reprinted by permission)
There are three main "muscle things" that occur with ALS: Spasticity, cramping and fasciculations.
All three are uncomfortable and spasticity and cramping can be very painful. It is helpful to
determine just which is causing the pain in order to get the right medication. Medications that work
for spasticity don't necessarily work for muscle cramps and vice-versa.
Spasticity is an upper motor neuron problem and is present to some degree in ALS. For some
patients it is minimal, for others extreme. Spasticity can actually be helpful in maintaining function
as the rigidity helps replace normal muscle strength, but it causes jerky, hard to control movements.
Spasticity causes a tightening of muscles that results in a stiffening of that part of the body in an
exaggerated reflex. It is actually triggering both the muscles to flex and the muscles to extend that
part of the body at the same time. It can occur in any muscles - the arms, legs, back, abdomen, or
neck. A simple touch can trigger it and it may last only a moment or persist indefinitely. Spasticity
isn't always painful but it can be, especially if it triggers muscle cramps that add to the pain.
Muscle cramps are very common in ALS, probably due to muscle fatigue or irritability from
screwed up nerve impulses. They can be terribly painful and can occur in any muscle - feet, legs,
arms, abdomen, chest, back, and (my all time favorite for sheer pain!) the neck and jaw. They can
be in small muscles or affect big ones -- good old-fashioned charlie horses. As the muscles are
affected by ALS, cramping is noted in that area. The cramping becomes less severe with time
because the weakening muscles simply can't work up a good cramp anymore. They tend to be
repetitive - once something starts cramping up, it does so over and over for a miserable hour or so.
They tend to occur more if you have overdone exercise, if the muscle is cold, or if circulation is
decreased. Holding a book up to read in bed on a cool night will just about guarantee some
whopping good hand cramps and result in interesting finger gestures!
Fasciculations (muscle twitching) are probably due to nerve irritability. They occur in smaller
muscle bundles inside large muscle bundles and can be observed as well as felt. Fasciculations are
not so much painful as irritating. It can feel as if someone is popping corn inside your legs! They
can be incredibly persistent and keep you from sleeping.
Is it Spasticity or Cramping?
Spasticity tends to affects larger areas of the body - arm, leg, trunk, neck. All the muscles in the area
tighten up and the entire area may be so tight it hurts. Muscle cramps are generally limited to a
single muscle and the pain, although intense even in small muscles, is limited in area.
40
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Spasticity often begins with an odd sensation, sometimes described as a quiver, rushing and
spreading through the area and becoming painful as they tighten the muscles and more so as the
muscles tire. Muscle cramps start out painful and just get worse as they tighten up.
Spasticity in the legs generally causes them legs to stiffen out. In the trunk, back or neck it causes
your body to arch a bit. In the arms it may flex or extend the arm.
Spasticity is often most striking when you first wake up or start to move after sitting still for a while
and can often be connected to a sensory trigger. Of course that trigger can be as mild as a gentle
touch so the connection may not be made.
Muscle cramps often affect the hands and feet making fingers and toes curl incredibly tightly.
Spasticity is more widespread, less likely to affect just those muscles, and more likely to stiffen
them out than to curl them.
Medications
Spasticity can usually be helped by medication but sometimes is a very stubborn problem. One
consideration in treating spasticity is to find a balance between relieving excessive and painful
spasticity and maintaining a certain level of spasticity which can be helpful by replacing muscle
strength. The meds for spasticity are primarily Baclofen, Dantrium and Zanaflex.
Although Baclofen is often listed under meds for cramping and prescribed for it, the indications say
"Clinically, baclofen is used to treat spasticity." In my experience, Baclofen did not reduce
cramping at all. However, if spasticity is triggering the cramping, Baclofen may reduce cramping
by reducing the spasticity. Some patients experience weakness or tiredness while taking it but these
problems can often be reduced if the dosage is decreased. In 1996 the FDA approved the use of
Baclofen, delivered by an implanted pump, for the treatment of spasticity due to spinal cord injury
and this is now being tested on ALS patients.
Zanaflex is the most recent medication approved by the FDA for treatment of spasticity. Zanaflex is
less likely to cause weakness but may cause sleepiness. This can often be minimized by starting
with a low dose and gradually increasing it until spasticity is relieved.
Dantrium has been used for spasticity, but because of its potential for causing liver problems, is
less frequently used since other meds are now available. It does seem to still be used for bladder
control problems caused by spasticity however.
Quinine is a drug long used for muscle cramping but in 1995 the FDA said studies showed it lacked
effect for "nocturnal leg cramps" and it is no longer sold for this purpose. Well, I don't know about
"nocturnal leg cramps" - I had cramps all over at all hours of the day and quinine worked very well
for me! I took it twice a day, morning and late afternoon or evening. (I have few muscle cramps
these days - not much left to cramp up - so I no longer use it.) I would certainly recommend asking
your doctor about trying quinine. I do not recall what dose I took, but do know that too large a dose
will cause weakness. I am told the smallest tablet made is 260mg. I would recommend beginning
with half a tablet and increasing to a whole one if it is ineffective. It is also available in 200 mg
41
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
capsules. It is much less expensive than the other drugs prescribed and, in my experience, the most
effective. Like any drug, it does have some potential side effects (and cannot be taken by pregnant
women) but it does not cause physical and psychological dependence as Valium does in long term
use. Aside from the weakness when I took the larger dose, I noticed no other immediate side effects.
After more than 5 years of daily use, I did notice sweet foods started to loose any sweet taste,
especially chocolate. Quinine is very bitter so I assumed it was the culprit since I wasn't on any
other meds at the time. It was a minor problem and when I did stop taking quinine, I found the
ability to fully enjoy an Oreo was gradually restored!
Valium and other muscle relaxants may be tried for spasticity but are probably better used for
muscle cramps. However, their side effects and cost make them a second choice to quinine in my
opinion.
I have not heard of anyone having any real success in reducing the fasciculations (muscle twitching)
with any medication.
About the Author
Diane Huberty is a retired RN. She worked general Med-Surg units, then 5 years in Critical Care
where she began specializing in Neuro and earned Neuro Certification (CNRN). Diane was
diagnosed with ALS in 1985 at the age of 37. When her hospital opened a Neuro Unit, she was
selected for the position of Neuroscience Educator. She was able to continue working in that
position until 1995, when arm weakness and fatigue made it too difficult to continue and she retired.
Through the Internet, Diane communicates daily with other ALS patients and keeps up on research,
treatments and care issues.
42
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Constipation
By PALS Diane Huberty, CNRN
(reprinted by permission)
What is constipation?
That may sound like a foolish question, but many people think of constipation as having infrequent
bowel movements. It is actually defined as having dry, hard stools that are hard to pass. Many
people have only a couple of bowel movements a week, but if they do so without straining, they are
not constipated.
Normally food is liquefied in the stomach by digestive juices and moves through the small intestine
in liquid form. Nutrients are absorbed in the small intestine. Waves of muscle contraction called
peristalsis move the remainder along into the large intestine. In the large intestine, water is
reabsorbed from the left over waste product, leaving just fecal material (stool), which is moved
along and passed out of the body in a bowel movement.
Anything that changes the speed with which foods move through the large intestine interferes with
the reabsorbtion of water and causes problems. Rapid passage causes diarrhea, slowed passage
allows too much water to be reabsorbed, leaving hard, dry stool that doesn't move easily through the
bowel. Many medications affect this but constipation is common for anyone with poor mobility,
lack of activity and exercise slow bowel mobility. Long delays in getting to the bathroom further
complicates the problem by keeping the stool in the large intestine longer where it becomes dryer
and harder. In ALS swallowing problems make getting a good diet and sufficient fluids difficult
and the problem gets worse. Breathing problems make it difficult to take a deep breath and bear
down, something we don't even realize is important in having a bowel movement until we cannot do
it. Because so many things contribute to constipation in the ALS patient, the solution may change
over time.
Although we joke about constipation, it is a miserable experience and should never be taken lightly
in the ALS patient. Loss of appetite from frequent constipation leads to weight loss, weakness and
dehydration. It can progress to nausea and vomiting, very dangerous for a person who cannot turn
over when lying on his back. The blockage can become so severe as to require hospitalization to
correct.
Diet
The first - and best - way to approach constipation is by improving your diet. Eat lots of high fiber
foods. (Check with your doctor if you have other digestive or bowel problems or are on a special
diet.) There are many high fiber cereals available and granola bars are convenient and easy to
handle when feeding yourself begins to be difficult. Raw fruits and vegetables are also easy to eat
sources of fiber if swallowing is not a problem. Drink lots of fluids. If you are using tube feeding,
43
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
fiber is added to most tube feedings formulas and high-fiber formulas are available. When diet
alone isn't quite enough, try the old remedy of prunes or prune juice. It really does work!
Laxatives
Remember that everyone's bowel pattern is different. Very few people need to have a daily bowel
movement. Every other day or every third day is probably most common. Insisting on a daily
bowel movement and using laxatives to try to attain it is asking for trouble!
There are basically 3 types of laxatives:
•
•
•
Bulk or Fiber Laxatives supply the fiber necessary to add bulk which holds water and makes it
easier to move the stool through the bowels.
Stool Softeners also keep the water content of the stool higher which keeps it softer and allow it
to move more easily through the bowels.
Stimulants increase the muscle contractions (peristalsis) of the bowel which moves the stool
along. These are available as pills that generally result in a bowel movement in 6-12 hours and
as suppositories that work within an hour.
Generally the first laxative recommended is a high fiber laxative such as Metamucil or Citracel.
Fiber laxatives are available as a powder, (which is mixed with water or juice and generally needs
to be drunk fairly quickly before it thickens) a tablet, or a chewable tablet. Fiber laxatives are very
slow acting are generally taken daily to prevent constipation rather than for relief once constipation
is making you uncomfortable. For the ALS patient there are two concerns with this type of laxative.
First, it is essential that fluid intake be very good. Taking fiber laxatives without enough fluid can
cause intestinal blockage. Second, they are not to be used when swallowing problems begin.
Failure to drink enough water to wash down the fiber might allow it to begin to swell in the
esophagus and this requires immediate medical attention. Fiber laxatives can safely be given
through a feeding tube, but the fiber needs to be promptly followed by flushing the tube with water
to prevent clogging.
Stool softeners are often ideal for ALS patients. Not only do they help when fluid intake is difficult,
but they also are very helpful when breathing problems make it difficult to bear down and push.
The longer stool remains in the digestive tract, the more water is removed from it. As the stool
becomes dryer, it becomes harder and more difficult to move along. Stool softeners prevent the
drying and allow the stool to move through with normal peristalsis. They do not cause cramping or
urgency but greatly reduce the amount of straining needed to have a bowel movement. Stool
softeners are generally taken daily as a preventative measure. Stool softeners are available in pill or
liquid form.
(Note: I don't know about other brands, but Colace liquid needs to be diluted in juice or it burns all
the way down!) If the stool softener alone isn't sufficient, they are also available combined with a
stimulant laxative.
44
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Stimulant laxatives increase the normal peristalsis to move the stool quickly and forcefully along.
Most are intended to be fairly gentle result in a bowel movement within 6-12 hours, but even these
can cause cramping. If constipation is already making you uncomfortable, suppositories will
provide relief within an hour but are likely to cause cramping. Stimulant laxatives should be
reserved for occasional use until other methods fail.
Frequent use of stimulant laxatives can actually aggravate constipation because the bowels become
dependent on them for the stimulation for even normal peristalsis. Stool softeners and stimulants
are available in combination and may be needed when stool softeners alone are not effective.
Enemas are all right for occasional use but are generally the last resort as a routine method of bowel
management. The repeated distension of the bowel can eventually cause loss of bowel tone which
aggravates the problem. This "eventual" problem is not a concern for the ALS patient who does not
plan on going on a vent, but should be considered when planning a bowel program for long term
use.
Daily Routine
Few people need to have a daily bowel movement but having a routine time when you can spend a
longer period of time on the toilet is helpful. Although choosing a time is probably going to be more
a matter of convenience for your caregiver, if you already have a certain time of day you are more
likely to have a bowel movement, try to arrange for that time. If having a bowel movement at a
consistent time of day is important because you don't always have the necessary help to get to the
toilet the rest of the day, you can encourage that schedule. Begin by using a suppository or stimulant
laxative to promote bowel movements on the scheduled day at the chosen time. After a week or
so, use the laxative only if you can't have a bowel movement on your own. Within a week or two,
you should be able to reduce the stimulant laxative use to very infrequently.
An unrushed and private bathroom trip is ideal, but safety and security need to be assured. Having
some type of buzzer or doorbell type button (available from Radio Shack) to call for help works
well. Sitting upright and as comfortably as possible is also important. Armrests and a seatbelt
might be necessary for safety. (The correct and safe angle for a seatbelt is diagonal as they are in
cars: The belt is around the hips and anchored lower. A belt anchored behind you at stomach level
will allow you to slide down through it and end up tight around your chest.) A padded toilet seat
can be a lifesaver! If you have a high-rise toilet, using a footstool and leaning forward over a pillow
can help provide the necessary push. Drinking a cup of coffee or other hot beverage before or while
in the bathroom will often help.
45
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Managing Neck Muscle Weakness
Based in large part on an article written by
Pamela A. Cazzolli, R.N.
Some people with ALS develop muscle weakness of the neck. This may cause limited mobility of
the head. Turning the head from side to side or holding the head upright may be difficult, as the
neck supports the head that weighs about 20 pounds. Limited head movement can contribute to a
stiff neck, a poor head posture, and severe pain if these problems are not managed. In fact, neck
muscle weakness can lead to a vicious cycle of limited head mobility and a stiff neck (resulting in
pain and impairing head mobility ever further), causing more pain with emotional distress.
Emotional stress can also compound muscle tightness and cause pain.
People with neck muscle weakness are vulnerable to injury. If the head suddenly flops backward,
forward, or sideways, this can cause muscles and ligaments in the neck to tear. It can also cause
serious injury to the cervical spinal cord or vertebrae in the neck. Such injuries may be a result of
"overstretching" due to a sudden excessive force that propels the neck forward, backward, or to one
side or another. Hyperextension (backward) or hyperflexion (forward bending) injuries may be
referred to as a "whiplash."
This can occur, for example, when a person is transferring in or out of a bed or a chair and the neck
is jarred. For some people, even a slight jerk of the head can cause a torn muscle in a weak neck.
Injuries to the neck can be very painful, especially when turning the head, raising and lowering into
bed and rolling over when in a lying position. Besides causing pain and injury to the neck, poor
head posture can aggravate breathing, swallowing and communication.
Through effective management of neck muscle weakness, complications of pain and injury can be
prevented or treated. Finding the best methods for supporting the head in an upright position to
protect against injury is essential.
Strategies for improving the head posture and promoting head/neck mobility, comfort and
safety
1. Achieve and maintain a good body alignment when sitting to promote an upright head position.
Use of a cushion, pillow, or rolled towel behind the lumbar region of the low back not only helps to
align a slumped posture, but will help keep the head and shoulders from slouching forward. If
sitting in a high back chair, placing a rolled towel behind the neck also improves the head posture
and helps prevent or alleviate discomfort in the neck. Placing a pillow under each arm or on top of
each armrest of the chair helps promote an upright head position, and provides maximum comfort
when sitting for a long time. Proper alignment of the head, neck, and body allows the lungs to
expand for better breathing.
2. Wearing a soft collar or a neck brace, called a cervical collar, is an effective method of holding
up the head if this is difficult. A collar supports the head when the person is walking or being
46
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
transferred from one sitting position to another. To protect against injury from sudden motion,
people with advanced neck weakness should wear a collar when they are moving or being
transferred from one seat to another, when walking, or riding in the car. Use of a collar to hold up
the head when walking permits a better sight line and may reduce the risk of falling.
3. Identify and use the appropriate cervical collar(s) that will best meet your needs. Most people
with neck weakness are unable to tolerate wearing a collar all the time, especially one that can lead
to skin breakdown and discomfort. A variety of comfortable collars are available. Cervical collars
can be obtained at most medical suppliers, and the cost is usually covered by health insurance if
ordered by the physician.
4. To promote comfortable use of head support, alternating the use among several collars may be a
solution to reducing pressure points on the skin of long-term collar wearers.
5. Leaning back in a reclining chair is another method to support the head and to help keep the head
from falling forward. This may include a reclining wheelchair with a high back or one on which a
headrest can be attached. Power lift chairs also recline, and with a push of a button they can recline
back exactly to the desired angle. People with excessive oral secretions might have difficulty
reclining backward. To help prevent choking on oral secretions, the head can be positioned to the
side and propped with a pillow.
6. Using a wheelchair head support system can position the head in an upright position by a band
across the forehead that attaches to an adjustable headrest that mounts to a chair. Some head support
systems include the use of an elastic band. Head support systems usually can be obtained from a
medical supplier who specializes in wheelchair accessories. People who need maximum support in
holding up the head and who cannot tolerate long term use of a cervical collar might benefit from
intermittent use of a head support system.
7. When in bed, avoid sleeping on a pillow that is too high. This will not only strain the neck, but
may cause wakefulness at night. A rolled towel placed underneath the back of the neck with the
head resting on a low pillow can provide support and comfort of the neck and head when sleeping.
In addition, people who have trouble keeping their head upright might try lying in bed a few times
during the day to relieve the neck muscles.
8. Stretching exercises of the neck muscles can help promote mobility of the head, alleviate stiffness
of the neck, and help prevent and treat neck pain. To avoid injury, evaluation and training of other
exercises by a physical therapist or a visiting nurse may be warranted. Two exercises can be done
safely:
• Slowly turn your head to the right as far as possible, hold, and return to the center. Do the
same to the left.
•
Tilt your head straight over towards the right ear, hold, and return it to the center. Do the
same on the left side.
47
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
9. People who have unresolved neck pain or difficulty holding up their head should consult with
their physician who may prescribe physical therapy for treating their problems. A physical therapist
is specially trained to evaluate the neck, help relieve neck pain, make recommendations for
supporting the neck and head, and provide education on reducing the risk of neck injuries. Some
methods of treatment may include the use of moist heat, massage and exercises that stretch the neck
to alleviate stiffness and to enhance mobility and comfort. Life should not have to be a "pain in the
neck."
Choosing a Neck Support for Patients with ALS
ALS patients usually wear neck supports only for specific activities (i.e. walking, reading, riding in
a car or airplane, writing, or dressing). At other times, wheelchair head rests or high back chairs
provide the needed head support. Neck supports should not be worn while eating. Neck supports
that immobilize weakened neck muscles are usually rigid, uncomfortable, and may inhibit speech
and swallowing. It may be difficult to find a collar that will meet all the needs of an individual
patient and the type of support needed will change if weakness progresses. The therapist or
physician will need to test the strength of the neck and upper body muscles to determine the degree
and type of support required.
The patient should take an active role, with the help and advice from the medical team, in choosing
the neck support that best meets their individual needs. Most patients prefer the least "restrictive"
collar as possible, but one that will also provide adequate support. The proper amount of support,
combined with appropriate seating, postural training, and exercise, can improve comfort, function,
and independence for most ALS patients. Important questions to ask when selecting a collar
include:
1. Does the collar provide adequate support?
2. Does the collar cause sweating or friction?
3. Does the collar cause a "choking" sensation?
4. Is it affordable?
5. Is it cosmetically acceptable?
48
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
The following is a listing of collars that have been successfully used for patients with ALS.
Soft Collar
These collars are inexpensive and can be purchased from most
medical supply companies. They are used when there is very mild
neck weakness to prevent fatigue and strain. When significant neck
weakness occurs, these collars are not adequate to support the
weight of the head. Since they tightly encircle the neck, they may
feel restrictive and uncomfortable and therefore, they usually are
worn only for brief periods of time. Soft collars are available with
or without a vinyl stabilizing panel and in various contours, foam
densities (medium, firm) and heights (2", 3", 4", 4.5") to fit wide
range of patient neck sizes.
Headmaster Collar (Adjustable Wire Frame Cervical Collar)
This collar is lightweight, open, and is comfortable in warm
climates. It is easily formed by hand to fit snuggly under the chin. It
is made of a specially tempered wire frame which is liberally padded
with foam rubber covered in a soft, washable fabric and uses a
velcro closure strap attached to cushioned back piece. It is very
helpful for patients with weak neck extensors to prevent the head
from falling forward. However, if weakness is present in rotation
and/or lateral flexion (i.e. when shaking the head "no" or touching
the ear to the shoulder), it will not be adequate and more support is
needed.
Symmetric Designs Ltd. Toll Free Phone (Canada & USA): (800)
537-1724. Website: http://www.symmetric-designs.com/
49
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Executive Collar
Similar in general design to the Headmaster Collar, this collar is
made of a comfortable, lightweight Kydex frame and has an open
neck design. An occipital pad (back piece) attached to hook 'n pile
strap can be positioned to fit any neck circumference. Available in
small (4" height), medium (4½ height) and large (5" height) sizes.
As with the Headmaster, it is very helpful for patients with weak
neck extensors to prevent the head from falling forward. However, if
weakness is present in rotation and/or lateral flexion (i.e. when
shaking the head "no" or touching the ear to the shoulder), it will not
be adequate and more support is needed.
Aspen Collar
This collar (formerly called the Newport collar) encircles the neck,
is somewhat open, and provides motion restriction without creating
pressure points that lead to skin breakdown. It is extremely rigid,
yet flexible at its edges to conform to each patient's anatomy. Pads
& shells are removable and washable. This is the best style of collar
for ALS patients who have neck weakness in both flexion and
extension (up and down) as well as in lateral flexion and rotation
(side to side).
Aspen Medical Products, Inc. Toll Free Phone: (800) 295-2776.
Website: http://www.aspencollar.com/
Miami J Collar
This collar is similar in style to the Aspen collar. Its polyethylene
shell provides rigid support and immobilization. Contact pressure
is evenly distributed, and all contact points are padded. Sorbatex
padding absorbs and wicks moisture away from skin. Pads & shells
are removable and washable.
Jerome Medical. 305 Harper Drive, Moorestown, NJ 08057-3239.
Toll Free Phone: (800) 257-8440.
Website: http://www.jeromemedical.com/
50
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Philadelphia Collar
Constructed from high-density polyethylene plastic this collar
features removable Orthowick™ foam padding. The contoured back
of this collar provides support at the back of the head. The front
tends to restrict motion and confine the throat. If needed, an
extension can be used for more support, but results in additional
restriction. This collar is recommended when less restrictive collars
are unable to provide enough support.
Philadelphia Cervical Collar Company. Mid Atlantic corporate
center 1414 Metropolitan Ave. P.O. Box 566, Thorofare, NJ 08086.
Toll Free Phone: 800-923-9760.
Website: http://www.phillycollar.com/
PRO-DFS Wheelchair Head Support System
The PRO-DFS system provides wheelchair mounted head support. It
is especially designed to provide light anterior support for the
individual who has difficulty keeping his/her head in an upright
position. It uses a patented pulley system allows the forehead strap
to actually move safely with the user. An assortment of strap styles
are available.
Whitmyer Biomechanix, Inc. 1833 Junwin Court, Tallahassee, FL
32308. Toll Free Phone: (877) 944-8246.
Website: http://www.whitbio.com/
Reprinted with permission by Pamela A. Cazzolli, R.N., ALS Nurse Consultant in Canton, OH.
51
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Range of Motion Exercises
Range of Motion (ROM) exercises are done to preserve flexibility and mobility of the joints on
which they are performed. These exercises reduce stiffness and will prevent or at least slow down
the freezing of your joints as the disease progresses and you move less often. Range of motion is the
term that is used to describe the amount of movement you have at each joint. Every joint in the
body has a "normal" range of motion. Joints maintain their normal range of motion by being moved.
It is therefore very important to move all your joints every day. Stiff joints can cause pain and can
make it hard for you to do your normal daily activities. Each person with ALS needs a program
of exercise tailored to his or her individual needs and abilities. With a prescription your
doctor can either send you to an outpatient clinic to see a Physical Therapist or have one come to
your home to help you design a personalized exercise program. The therapist will see you until you
or your caregiver are independent with a home exercise program that you can follow through with
daily. It is important to remember that as the disease progresses, the type of ROM exercises you will
need will change. It is important to be proactive when this occurs and ask your doctor to write you
another prescription to see a therapist so your home exercise program can be modified.
There are different kinds of ROM exercises. There are stretching exercises you can do yourself
when you still have the muscle strength to move your joints through their complete ranges. These
are called Active ROM exercises. There are Self-ROM exercises, which involve using a stronger
arm to assist a weaker arm to perform the exercises, eliminating the need for caregiver assistance.
Then there are Passive ROM exercises, which are done for a weaker PALS by a caregiver. Often a
combination of the types of ROM exercises above will be used. For instance if a PALS has strong
arms but very weak legs, he would use an active ROM program for the arms independently and a
passive ROM program for the legs. Even within a limb the type of exercise used can vary
depending on the strength of the different muscle groups. PALS with increased muscle tone
(spasticity) will also need to learn techniques to decrease the tone before exercising. What type of
ROM exercises are most effective for an individual is best determined by a therapist who can
evaluate your own muscle strength and tone.
It is important to realize that these exercises will not strengthen muscles that have been weakened
by ALS. Once the supply of motor neurons that control a particular muscle has degenerated, it
cannot be regenerated by exercise. It is important that all exercise be performed in moderation.
Fatigue will only increase your weakness and rob you of energy that you need for your daily
routines and the activities you enjoy. If you find that your prescribed set of exercises tires you, talk
to your therapist. Changes can be made that will eliminate the risk of fatigue. Similarly, none of
your exercises should cause you pain. If you do experience pain when exercising, stop that exercise
and talk to your therapist. It may be that you are not doing the exercise correctly, or perhaps some
modification to your exercise program must be made.
If your joints are very painful and swollen, move them gently through their range of motion. These
exercises should be done slowly and steadily. It is important with ROM exercises not to force
movements and to stop a movement if it causes you pain. Damage to the joint space can occur if too
52
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
much force is applied. Joint range of motion is done on one joint at a time. Stabilize with one hand
just above the joint and place your other hand below the joint to move the part through its full range
of motion. Your physical therapist will tell you how many times to do each one.
General instructions:
•
•
•
•
•
•
•
Ideally, these exercises should be done once per day.
Do each exercise 3-5 times or move to the point of resistance and hold for 30 seconds.
Begin exercises slowly, doing each exercise a few times only and gradually build up to more.
Try to achieve full range of motion by moving until you feel a slight stretch, but don't force a
movement.
Move only to the point of resistance. Do not force the movement.
Keep limbs supported throughout motion.
Move slowly, watching the patient's face for response to ROM.
Lower Extremity Passive ROM Exercises
Lower extremity passive exercises are for someone else to stretch your hips, legs, and knees if you
are unable to do this yourself. These exercises should be done slowly and gently while you are lying
on your back. Each exercise should be done ten times on each leg each day.
Hip and Knee
Flexion
Cradle the leg by placing one
hand under the bent knee.
With the other hand, grasp
the heel for stabilization. Lift
the knee and bend it toward
the chest, with the kneecap
pointed toward the ceiling.
Do not allow the hip to twist
during this movement. The
foot should stay in a straight
line with the hip and not
swing in or out.
53
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Hip Rotation
Place one hand on the thigh
and other hand just below the
knee. Bend the knee halfway
to the chest so that there is a
90-degree angle at the hip
and knee. Pull the foot toward
you and then push it away.
Remember, do not go beyond
the point of resistance or
pain. Lower leg to starting
position.
Hip Abduction
Cradle the leg by placing your
hand under the knee and
holding it. Place the other
hand under the heel to
stabilize the hip joint.
Keeping the knee straight,
move the leg along the
surface of the bed, toward you
and away from the other leg,
to approximately 45 degrees.
Then bring the leg back to the
other leg.
Ankle Rotation
With the knee straight and
one hand holding the ankle
steady, place the other hand
around the foot and turn foot
inward, then outward.
54
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Toe Flexion and
Extension
With one hand, stabilize the
foot just below the toes. With
the other hand, gently move
each or all of the toes forward
and backward.
Heel-Cord
Stretching
Cups or cradle the heel with
your hand and place your
forearm against the ball of the
foot. Push the ball of the foot
forward, bending the foot
toward
the
knee
and
stretching the muscles in the
back of the leg.
Cup the heel of the foot into
the palm of your hand. Gently
push the foot down to “point
the toes.” Do this with knee
bent, then repeat with knee
straight.
55
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Lumbar Rotation
Bend knees up and keeping
them together, lower than to
one side as far as they
comfortably go. Repeat to the
other side.
Hamstring Stretch
With the knee and heel
supported slowly raise the leg
up, keeping the knee straight.
Return to starting position.
56
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Upper Extremity Passive ROM Exercises
Upper extremity, passive ROM exercises teach someone else how to stretch your arms if you are
unable to move your arms by yourself. These exercises should be done slowly and gently, and can
be done with the person sitting in a chair or lying down. Do each exercise three to five times.
Elbow Flexion and
Extension
Hold the upper arm with one
hand and forearm with the
other hand. Bend the arm at
the elbow so that the hand
touches the shoulder. Then
straighten the arm all the way
out.
Shoulder Flexion
and Extension
Hold the wrist with one hand.
With the other hand, grasp the
elbow joint to stabilize it.
Turn the palm inward, facing
the body, and keep the elbow
relatively straight. Move the
arm from the side of the body
over the head.
57
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Shoulder Internal
and External
Rotation
Place one hand under the
elbow. With your other hand,
hold the forearm. Bring arm
out to the side to shoulder
level. Turn arm so that the
hand points to the ceiling.
Then turn arm back down so
that hand points to floor and
the upper arm is twisting in
the shoulder joint.
Horizontal Shoulder
Abduction
Place hands behind or above
head. Gently touch elbows to
bed and hold as tolerated.
Stretch felt in chest.
Pull arm across chest. Stretch
is felt in back of arm and
shoulder.
58
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Neck Rotation
Turn head slowly to look over
left shoulder then turn to look
over right shoulder, touching
the chin to the shoulder if
possible.
Neck Flexion
Tilt head slowly toward left
shoulder and then toward the
right shoulder, touching the
ear to the shoulder if possible.
Thumb Flexion and
Extension
Move thumb to little finger.
Then bend and straighten the
thumb out to the side to
stretch the "web space"
59
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Finger and Wrist
Flexion and
Extension
Hold the forearm above
the wrist with one hand
and grasp the fingers with
your other hand. Holding
the hand in this way, bend
the wrist back, about 90
degrees, while
straightening the fingers
out. Then bend the wrist
the opposite direction,
about 90 degrees, while
curling the fingers into a
fist.
60
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Managing Saliva and Phlegm in ALS
The build-up of saliva is a common problem among people with ALS who have tongue and throat
muscles that are weak and not able to automatically swallow the saliva that builds up in the mouth.
A tenacious mucus can also build up in the mouth, compounding the problem. This build-up of
saliva can cause choking and disrupt sleep. Relief may come from home remedies, over-the-counter
products, prescription drugs and, in extreme cases, even surgical procedures.
Saliva is needed to moisten the mouth cavity and to help with swallowing and digesting food. It is
poured in copiously (at about a fivefold increase) when we smell, taste, chew and swallow food.
Saliva is normally secreted by three major pairs of salivary glands and numerous minor glands in
the mouth cavity. Some secretions also come up through the respiratory tree, as part of the
protective mechanisms that we all have. Saliva comes in two parts —thin, watery secretions and
thick, mucus-containing secretions.
In ALS, there is no problem with saliva production. Saliva production is normal; it's the handling of
saliva that is not normal. In ALS, you can have weak muscles around the mouth, tongue, throat and
so forth which can compromise the handling of saliva in the mouth and the swallowing mechanism.
Some people have a lot of drooling, also called sialorrhea. Others complain more of phlegm sitting
in the throat. They can't swallow it, and they can't cough it up because of weak muscles. Sensation
is normal in ALS, so patients know that secretions are sitting in the mouth and building up, and that
they're drooling.
Managing Saliva
The first step in treating sialorrhea is typically to prescribe medications to reduce the production of
saliva. For example, many patients are on antidepressants and doctors will commonly try to give
them antidepressants that have the side effect of dryness of the mouth. This side effect is notable
with the tricyclic type of antidepressants such as amitriptyline (brand name Elavil), imipramine
(brand name Tofranil) and clomipramine (brand name Anafranil). In some patients, doctors use a
scopolamine patch (brand name Scopoderm), which is usually used for motion sickness. The patch
is applied to the skin. Other medications that are often prescribed include atropine sulfate (brand
name Sal-Tropine), clonidine (brand name Catapres) and propantheline (brand name Pro-Banthine).
All these agents block the action of acetylcholine, which comes from the nervous system and
normally gives a "kick" to the salivary glands to produce saliva. Acetylcholine is a neurotransmitter,
a chemical that carries signals between the nervous system and other organs. The glands are still
intact, and not all the saliva is gone. Up to approximately half the saliva production is knocked
down in patients who can tolerate these medications. These are mild drugs, and their side effects are
mild.
If tricyclic antidepressants, scopolamine or these other medications are not effective, the next step is
to go to more potent drugs like glycopyrrolate (brand name Robinul). These drugs block
acetylcholine wherever it is in the system, and they can cause constipation, urinary hesitancy and
61
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
impaired potency. Drugs such as Robinul can also worsen glaucoma in those that already have it,
can increase urinary obstruction if people have an enlarged prostate gland and can worsen
confusion in people with memory loss. Patients in a humid environment may also feel a little more
discomfort because of decreased sweating. All these symptoms are from the blockade of
acetylcholine. Some patients have more side effects than others. Some people don't tolerate these
medicines because of side effects, and in some people they're just not effective.
If medications like Robinul are not effective, the next step is the injection of botulinum toxin (brand
name Botox or Myobloc), which comes from the bacterium Clostridium botulinum. It works in the
same way as the medications, by blocking acetylcholine release from nerve endings, but only at or
near where it's injected. Typically the botulinum toxin is injected into each parotid gland. The
parotids are the major glands for the thin, watery part of the saliva. The problem with botulinum
toxin is that if it's injected at the wrong site or if it travels, it can block muscles in the area and
increase dysphagia (difficulty swallowing) and dysarthria (difficulty speaking). It takes a week to
10 days for the maximum effect to be seen. In about two weeks, you know whether or not it has
worked. If it hasn't, after about three weeks, a little more of the botulinum toxin can be injected on
both sides. Depending on the response, the botulinum toxin can be injected a second or third time.
Typically saliva production is knocked down by about 50 or 60 percent in about half the patients.
With a second or third injection, it's usually effective in about 75 percent of patients.
Three major, paired glands - the parotids,
submandibulars and the sublinguals - and
numerous minor glands throughout the
mouth (not shown) normally produce saliva.
Injecting botulinum toxin (brand name
Botox or Myobloc) into the parotid glands is
one of a number of strategies used for
reducing saliva and controlling drooling in
ALS.
In a few patients, radiation of the salivary glands has been used as a last option. The idea is to
damage the gland and to induce scarring which takes several weeks or months. The idea is not to
knock down saliva totally but to decrease it to relieve drooling. The problem with radiation is that
it's irreversible. There are also reports in the medical literature of surgeries that can be done on the
salivary glands, but this is not generally done in ALS.
62
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Dealing with Thick Phlegm
At some point many ALS patients may experience problems with the thick mucous or phlegm that
accumulates in the back of the throat. This is often exacerbated during or after meals or liquid
intake. Coughing it up can be a tiring and arduous process, and take it's toll on the patient and the
caregiver. It also has a tendency to block airways or make food stick in the throat, so coughing it up
is essential.
There really isn't a good treatment for the mucus secretions, because those don't have a major nerve
supply that can be blocked. Adequate fluid intake is the first essential step in prevention. Sips of
cold carbonated drinks, hot tea with lemon, Rose's Lime Juice, and apple, pineapple or papaya juice,
all available at most supermarkets, may help. These may be kept in the fridge and used on a swab
for the mouth if the patient is unable to swallow. Meat tenderizer mixed with a little water can also
be used to coat the tongue or can be placed under the tongue. Some patients have found that 12-hour
allergy medications such as Zyrtec, Claritin or Allegra significantly reduce the amount of mucous
produced.
For PALS who face unresolved problems with phlegm, contacting your physician and requesting an
order for a suction pump and a visiting nurse to educate and demonstrate safe and effective airway
secretion clearance is a good idea. Often times, doctors or clinics only think of suction machines for
use with trach patients, so it's important for you to tell your doctor this is something you need. Also,
request two types of suction catheters if you have feelings of phlegm stuck in the throat. While
physicians may order only Yankauer suction tubes (often referred as Tonsil Tips), those tubes
cannot reach secretions or phlegm effectively down in the throat. Therefore, a French suction
catheter (such as a size 14) is always good to have on hand. This is a long narrow, soft and flexible
plastic tube. Because training on suction techniques is a skilled nursing procedure, expenses for
home visits by a registered nurse are covered by Medicare, Medicaid and most health insurance
companies. However, be sure to request that ONLY a registered nurse with respiratory care
experience be sent out to demonstrate how to use it safely and effectively to suction the mouth and
the throat.
The Cough Assist machine (also know as a Coffalator or In-Exsufflator) may be effective for
selected individuals, although not everyone may have insurance coverage for it or adapt to its use
(particularly those with advanced bulbar impairment). However, PALS who do use the device will
usually also need a suction pump with appropriate suction catheters to clear phlegm and secretions
from the throat and mouth. A portable suction pump provides a means for quick secretion clearance,
and thus, helps to serve as a safety precaution. However, all suction machines need to be checked
regularly to be sure they are working properly and have adequate "suck power." Be sure to always
keep portable units charged and ready to use. Some portable units have a tendency to lose their
power after a period of time. Therefore, ask your respiratory equipment supplier about your unit and
how to check and see if the pressure settings are adequate.
63
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
It's best to order and start using a suction machine (and Cough Assist) early on, while the ALS
patient still has the ability to cough. This way he/she can help force the phlegm to the top of their
esophagus and where the "yankheur" tool can easily reach to suction it away. It is helpful to suction
the roof of the mouth, back of the throat (watch out for the uvula, you don't want to suck that up) to
reduce the stream of mucous. Make sure to ask that your physician prescribes a portable suction
machine rather than a table top unit. A portable suction machine is lightweight and maneuverable.
The portable machines generally have a battery backup, as well as a removable AC cord and many
come with a carrying case and a DC converter, which allows you to plug it into a cigarette lighter. A
portable unit allows the caregiver to bring the relief to the patient rather then vice versa. It also
allows you the luxury of bringing it with you when going out. Suction machines are considered
durable equipment, so your Medicare or insurance should provide for its purchase.
Swallowing Problems (Dysphagia)
Adults swallow about 2400 times a day. We swallow many times during every meal, and regularly
throughout the day and night to clear saliva from our mouths. We do it so automatically that most
people never think about how it happens. It is, in fact, a complex series of movements. Five or six
major central nervous system nerves and about 23 muscles are involved in swallowing. This is why
people with medical conditions like ALS, that affect the nerves or muscles of the face and neck,
have swallowing problems. Swallowing can be disrupted if the muscles of the mouth or throat are
weak or uncoordinated. Difficulty in swallowing is known as dysphagia (dis-FA-je-uh).
Many ALS patients suffer from dysphagia or difficulty in chewing or swallowing. Signs of
dysphagia include choking on foods or liquids, drooling, trouble swallowing medications, increased
length of mealtimes, a wet gurgling sound to the voice, coughing and frequent clearing of the throat,
weight loss, need for the Heimlich maneuver, or pneumonia. Complications can be severe and
include aspiration pneumonia, dehydration, malnutrition, weight loss and increased muscle wasting
due to decreased calorie and protein intake. If you are experiencing any of these symptoms it is
important that you discuss these with your physician. A referral can be made for an evaluation by a
speech pathologist and dietician. The dietician and speech pathologist can work with you to learn
techniques to make swallowing easier, safer and keep you eating by mouth longer.
The Swallowing Process
Swallowing occurs in the oral cavity, pharynx, and the esophagus. Below is a cross-sectional view
of the head and neck showing the structures and muscles that are used during the swallowing
process.
64
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
The purpose of swallowing is to get food from the mouth, through the throat (pharynx), to the
stomach, without allowing it to come out the nose or go down the windpipe (trachea). The throat is
essentially a tube of muscle, and it is the common pathway for air, food and drink, branching
midway down the neck. The throat (pharynx) divides into two near the top. The tube at the front is
the windpipe (trachea), which goes to the lungs. At the top of the airway is the voice box, or larynx
- you can feel it as the Adam's apple in your neck. Behind the larynx is the gullet, or esophagus, the
tube that takes food to the stomach. When we swallow the muscular soft palate (the back part of the
roof of the mouth) lifts to close off the nasal cavities and stop food going upwards. The muscular
throat then squeezes the food downwards into the esophagus. To stop the food going the wrong
way, the larynx does two things: It acts as a valve to close off the airway; and it tips forward, out of
the way - you can see this movement in the Adam's apple.
Before swallowing food is chewed and held in the mouth. There is nothing in the throat, the
windpipe is open and breathing occurs. When you swallow, the food is pushed into the throat, and
the windpipe closes off. Food then slips down the tube at the back leading to the stomach. Because
the windpipe is closed, you momentarily stop breathing. Once the food has passed through the
throat, the windpipe opens up again and breathing can resume.
If you have any food or drink in your throat when your windpipe is open and you are breathing,
there is a chance it could fall into the windpipe. This is experienced as 'going down the wrong way'
and coughing usually ensues. Aspiration is when liquids or food do go down the wrong way and are
not removed by coughing. A cough is the body's response to 'foreign bodies' entering the airway or
windpipe. It is our way of protecting our lungs from getting clogged up and interfering with
breathing. Unfortunately, in addition to swallowing problems, ALS symptoms also often include
weak respiratory function resulting in an inadequate 'protective' cough.
65
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Difficulties in eating and/or swallowing can develop for a variety of reasons. The problem is best
understood by looking at the three different stages involved in swallowing, and associated
behaviors, separately.
1. Oral Preparation Stage - The lips, tongue, teeth and cheeks break up food, mix it with
saliva and form a soft ball that can be swallowed. In the case of liquids, it is a question of
control. The food or liquid is then gathered into the center of the tongue by using a sucking
movement of the tongue, lips, and cheeks. The tongue forms a cupped shape around the
liquid and holds it ready for swallowing. The entire bite or sip (bolus) is then pushed by the
tongue to the back of the mouth, or oral cavity.
2. Pharyngeal Stage - The tongue squeezes the food or liquid to the back of the mouth and
the swallow reflex is triggered. As the food is being pushed to the back of the mouth, the
larynx rises and the vocal folds close to keep food out of the lungs. The soft palate rises to
close off the nasal passage. This begins the involuntary portion of swallowing. The bolus is
moved by muscles through the pharynx, past the closed larynx, and into the esophagus.
Muscles in the wall of the throat assist movement of food/drink downwards to the stomach
by wave like movements called peristalsis.
3. Oesophageal Stage - This is the movement of food from the lower part of the throat,
through the gullet (oesophagus) to the stomach, assisted by a continuation of the peristaltic
wave.
Problems with swallowing in ALS patients can arise at any of these stages, either in isolation or in
combination. Muscle movements may become slow or uncoordinated; the swallow reflex can
become delayed or incomplete; or the coordination of all three stages can become unbalanced.
Diagnosis
First, an initial assessment and screening process is conducted by a physician. It is often beneficial
to maintain a diary of the swallowing difficulties observed, including the setting in which the
symptoms occurred, and with which foods or liquids. This will make the swallowing evaluation
more thorough and the recommendations more specific to your needs. Then if the physician feels it
is needed, a speech pathologist does a thorough evaluation.
In this evaluation the speech pathologist goes through the patient's medical history, interviews the
patient and family, and performs a swallowing assessment to see if there is a disorder. The
swallowing assessment is where a speech pathologist gives a patient a variety of items including
liquids, pureed foods (an eatable substance between solid and liquid), and solid foods in different
consistencies to swallow. The speech pathologist observes the patients swallowing and determines
if there is a problem.
66
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
If the speech pathologist feels the patient requires further evaluation, he/she will perform a swallow
study. The objective is to show exactly what is happening when a patient swallows a variety of
different consistencies and amounts. The speech pathologist takes the information from the
swallowing study and determines the nature of the problem and what needs to be done. Swallowing
studies can be performed using variety of techniques including:
•
•
•
Videofluoroscopy. This is an x-ray recorded on video tape. For this test you drink different
volumes and viscosities of barium solution.
Endoscopy. A thin, flexible instrument called an endoscope is passed through your nose and
down into your throat. An endoscope consists of a fiber optic tube with a miniature
television camera on the end of it which is used to look inside the body.
Manometry. A small tube is inserted into your esophagus and connected to a pressure
recorder. This measures the muscle contractions of your esophagus as you swallow.
Strategies for Safer Swallowing
Below are listed some common strategies and tips used to facilitate safe swallowing. It is, however,
recommended that the advice of a speech language pathologist who specializes in swallowing
disorders be sought, as recommended strategies will vary according to the stages of the swallow
affected and the client. Other professionals, such as a dietician or occupational therapist may also
need to be involved. Ways to promote safe eating that may be suggested by a speech and language
therapist include:
Swallowing Tips
•
•
•
•
•
•
•
•
•
•
•
Sit upright, preferably in a chair, during meals.
Eliminate distractions such as television or conversation during meals.
Concentrate on maintaining a slow, steady rate of feeding.
Make sure the mouth and throat are clear of excessive secretions/saliva prior to eating or
drinking
Avoid taking too large a bite, drinking too rapidly or placing more than one bite in your
mouth before swallowing
Maintain the head in a slightly chin tucked position when eating or drinking. If you put your
head back to drink you are opening up the airway more making it is easier for food and
drink to go down the wrong way.
Swallow two to three times to make sure all food has cleared your throat.
Alternate swallowing food and liquids to assist with clearance of drier or more textured
foods..
Moisten food with sauces and gravy.
Take small mouthfuls of food and small sips of drinks.
Use a straw to drink liquids to enable you to keep your chin down.
67
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Changes in Diet
Special diets (soft or puree), merely avoiding certain foods, or preparing them differently can make
a big difference. There are also cookbooks available for those who have difficulty swallowing.
Foods that may present difficulty for someone with a swallowing problem include:
•
•
•
•
•
•
•
•
Items of mixed consistencies or textures such as cold cereal and milk, chicken noodle or
vegetable soups and fruit cocktail. These items should be blended into one consistency.
Highly textured foods such as red meats and raw vegetables.
Dry foods such as rice, pretzels, potato chips, crackers and cookies.
Stringy textures such as bacon, celery and string beans.
Floppy textures such as lettuce and cabbage.
Sticky foods such as mashed potatoes and peanut butter.
Small, hard textures such as peanuts and corn.
Dairy products, which often have a tendency to make secretions thicker.
Changes in Food Preparation
•
•
•
•
•
Consider changing to soft, moist foods such as canned fruits or cooked vegetables, fish and
chicken, complemented with gravies and sauces.
Cooking food longer so it becomes softer. Mashing it with the back of a fork or liquefying it
in a blender can help.
Thickening fluids to yogurt consistency may help as they are easier to control. Thicken
liquids with a commercial thickener (such as Thick-It, Thicken-Up, etc.), potato or banana
flakes, or fruit purees.
The use of nutritional supplements such as Ensure, Slim Fast and Carnation Instant
Breakfast if necessary.
Crushing medications or using a syrup form may be easier for someone with a swallowing
problem but seek advice from your doctor or pharmacist as some tablets need to be taken
whole.
General Suggestions
It is important to maintain good oral hygiene.
•
•
•
•
•
•
•
A portable suction machine may be of value to assist with clearance of secretions.
Drinking more fluids will help keep secretions thin.
Your physician may have suggestions for medications to thin or reduce secretions.
Avoid medications that dry up secretions, making them thick and more difficult to manage.
It is important that the caregiver be educated in the use of the Heimlich maneuver.
Monitor the patient for dehydration and for weight loss.
Be alert to the signs of pneumonia, including increased chest congestion, chronic low grade
fevers and increased cough.
68
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
•
•
The use of nutritional supplements may be of value to increase caloric intake quickly and
easily.
Supervision during all meals is always a good idea.
Alternate Feeding Methods
Sometimes the strategies noted above may be insufficient to ensure an adequate dietary intake. If
you find your intake of food and supplements is inadequate to maintain your weight or nutritional
status or is just too risky because of choking, then it may be the time to consider alternative methods
of eating. After discussion with your physician, speech pathologist and dietician it may be decided
that feeding via a tube directly into the stomach is the best and safest option. This is called a feeding
or PEG tube, and it can be used in conjunction with eating small amounts orally, or can be used
alone. This is a very personal decision and should be discussed at length with family members and
physicians. A feeding tube will provide adequate nutrition; however, it will not entirely eliminate
the risk of aspiration. It is important that you consider this option early to prevent unnecessary
complications. Studies suggest that early placement of the feeding tube can be utilized to
supplement oral intake and allow you to eat more for pleasure.
Food and eating is central to living in terms of pleasure and socializing as well as survival, therefore
eating and swallowing problems have a major impact both on the person directly affected and those
caring for them. It is possible to compensate for many difficulties, and support and guidance from a
speech pathologist can make the difference.
69
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
About Feeding Tubes
As ALS progresses, throat/muscle control over swallowing commonly become impaired. As it
becomes increasingly difficult to swallow, meal times become longer and longer and choking
episodes become more common. This can result in food or liquids entering into the lungs instead of
the stomach (aspiration), thereby increasing the risk of pneumonia, and in inadequate intake of
liquids and/or calories resulting in dehydration and weight loss. Additionally, although the patient’s
appetite typically remains good, the effort involved with eating can consume a tremendous amount
of energy from the patient and caregiver. For patients who tire from the efforts to chew and swallow
food and/or caregivers who spend an excessive amount of time feeding the patient, tube feeding can
result in a significantly improved quality of life. Not only does it give you more free time for
enjoyable activities or to just relax with one another, it enables the patient to get the proper
nutrition/fluids they could not consume.
From a medical standpoint, a feeding tube is recommended when the ALS patient is no longer able
to ingest sufficient liquids to prevent dehydration and/or sufficient calories to maintain body weight.
A feeding tube should be suggested by the physician after swallowing tests have determined the
patient can no longer safely eat sufficiently to maintain their body. A swallowing study is typically
performed by X-Ray technicians and commonly includes video taping the patient swallowing
various consistencies of liquids/foods. If a feeding tube is recommended, it is then the
patient/caregiver's responsibility to make the determination whether or not they want to have this
procedure done in order to maintain life.
The decision to get a feeding tube is a personal decision. It should be made by the patient (or their
caregiver based on their knowledge of the patient's wishes) in concert with their physician, and
should be heavily influenced by the patient's quality of life. If the patient no longer has a will to
live, compounded by overwhelming physical deterioration, then the choice to die a peaceful death
can be honored by not providing fluids or nutrients through a tube. A normal, healthy body will
typically die within 14 days from the lack of liquids and food and someone with a serious illness
can succumb sooner than that. Most medical professionals agree that it is a very painless choice in
dying.
Like any decision though, deciding whether or not to get a feeding tube should be an informed
decision. The ALS patient, their family and their caregivers should understand what is involved so
they know all the pros and cons of deciding whether or not to proceed with getting a feeding tube.
The following will, hopefully, provide some information on feeding tubes which will help enable
the ALS patient to make an informed decision.
G-Tube Types and Placement
What does a G-tube look like?
There are various different types. The two main ones are a PEG (Percutaneous Endoscopic
Gastrostomy) and button. The PEG is a length of tubing with a valve at the end, which protrudes
several inches from the incision area. Sometime this is put in first until the stoma site has healed
70
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
well. It can then be replaced with a button. A button looks very much like the small valve that is
used to inflate a child's beach-ball. It is made of clear, soft plastic and sits right next to the skin and
is flush to the body. A length of tubing is connected at feeding times.
Moss Tubes, Inc.
PEG Tube
Kimberly Clark (Ballard)
MIC-KEY Button Tube
Kimberly Clark (Ballard)
PEG Tube
Kimberly Clark (Ballard Medical Products) - http://www.kchealthcare.com/
Moss Tubes, Inc. - http://www.mosstubesinc.com/gastro.html
How do they put in a G-tube?
This depends on each individual. The medical team will decide the best way depending on how old
the person is, how good their breathing is and what sort of tube they are going to have. The
placement of a feeding tube is a relatively simple procedure. As with any surgery, patients are more
likely to experience complications if they are smokers, obese, use alcohol heavily, or use illicit
drugs. In addition, some prescription medications may increase risks associated with anesthesia.
The most common procedure for fitting the G-tube is called percutaneous endoscopic gastrostomy
(PEG) tube placement. It is typically a short surgical operation that lasts about 20-30 minutes which
is usually done with mild sedation given in the vein and a local anesthetic. The doctor will guide an
endoscope through your mouth and into your stomach. An endoscope is a long, narrow tube with a
camera and light on the end of it. It lets your doctor look into the inside of your stomach showing
the surgeon where to make the hole. During the surgery, a hole (called the stoma) about the
diameter of a small pencil, is cut in the skin and into the stomach just below the lower ribs. The
stomach is then gently attached to the abdominal wall. The G-tube is then fitted into the stoma. It is
a special tube held in place by a disc or water filled balloon that has a valve inside allowing food to
go in, but nothing to come out.
The patient is observed in a recovery area for about an hour, and then moved to their hospital room.
Depending on their level of health prior to having the PEG installed, their stay could be 1 to 2 days
for observation of acceptance of the feedings. The stomach and abdomen will usually heal in 5 to 7
days.
71
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Will it hurt?
There may be some discomfort from gas/air or adjusting to the liquid foods. There will be slight
discomfort at the incision site after the operation but this can be dealt with using ordinary
painkillers. Once it has healed you will hardly feel it is in there.
Will people know that I have a G-tube?
The tube is very small and is hidden by clothing, so nobody will notice it unless you show them.
Care and Maintenance
How much time will it take to care for the G-tube?
Usually G-tubes need very little maintenance. They need to be kept clean but a bath or shower does
most of this for you.
What is the stoma?
The stoma is the surgical hole into which the G-tube is placed.
What does a "good" stoma look like?
Ideally, the site should be flat, dry and not tender or excessively red. If the site is red, oozing
profusely or has a foul odor, you might have an infection. Consult your physician.
How should I clean my stoma?
The first week there is more care than afterwards since surgery has been performed. Sterile gloves,
gauze etc., must be used to clean the area thoroughly around the wound. The nurses and doctor will
instruct you in this procedure and will usually give you a booklet to take home with you. The
incision will heal but of course remains open since the tube is through it. Afterwards the incision
has healed; daily care of the G-Tube site is simple. The area around the stoma and under the tube
flange should be cleaned daily with warm tap water and a tissue or gauze. A mild soap can be used
to remove any small crusts. Allow it to dry completely. Some people carefully use a hair dryer to
speed drying. There is no need to use saline (salt water) or sterile liquids - clean tap water is fine.
What sort of dressing should be used?
Ideally, none. The site thrives on fresh air and a daily shower or bath.
Will it leak?
Occasionally the tube may pull away from the abdominal wall resulting in leakage around the
insertion site. Most G-tubes leak a small amount but this is easily taken care of with a little damp
cotton. The fluid that leaks out from the stomach can irritate the skin around the tube so it is
important to clean any leaks. If skin irritation is noticed apply a little protective cream or a
prescription skin barrier for protection. Normally, the degree of leakage is very small and it will not
be enough to mark or stain clothes. Leakage may also occur if the stoma site (incision) enlarges in
72
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
the patient with poor nutrition A tube that leaks more than a little, probably needs replacing because
the balloon is leaking or it is not the correct size.
What is proud flesh?
Occasionally the development of what is referred to as granulation tissue or "proud flesh" will
occur. This is basically skin that grows around and sticks out from the stoma site. The use of
hydrogen peroxide to clean the stoma site can lead to the growth of granulation tissue. Treatment is
simple and painless. When it becomes bothersome, you can get rid of most of it by cauterizing the
flesh with silver nitrate. This devitalizes or burns away the tissue and in a few days, it sloughs off.
Your Gastroenterologist prescribes the silver nitrate in the form of a caustic pencil or applicator
sticks that look like long matchsticks.
What other complications might there be?
Occasionally, the skin around the stoma can become sore or infected, or it can get a bit hardened. It
is therefore important to look at the stoma when cleaning it and let your nurse/doctor look at it if
you are concerned. Stomach ache, bloating or diarrhea can also occur if too much food is put into
the stomach too quickly. This may happen if the stomach is not used to large volumes. A feeding
regime should be discussed with your doctor or a dietician so that tolerance can be gradually built
up.
Does the feeding tube ever need to be replaced?
The feeding tube does not last a lifetime. They typically have a life span of about 6-12 months so it
is important to understand they may have to have it pulled out and a new one inserted. If there is
substantial drainage but flushing can be easily done, there is a good possibility a replacement tube is
needed.
What happens if the tube comes out?
This is unlikely as the tube is secured either by a little water filled balloon or a small plastic disc. As
the hole is only a fraction of this size, the tube cannot pull out until the balloon is deflated, which is
only normally done to renew the tube. If the tube ever does come out - don't panic. Place a clean dry
towel over the stoma to absorb drainage. If there is an extra on hand, replacement of a button can
often be done at home if the caregiver has received training. Otherwise calling a doctor or visiting
the hospital emergency room is in order. In either case, it is a good idea to have an extra tube on
hand. Remember though, the key to quick and easy replacement of a button of any variety is speed!
It only takes a few short hours for the stoma to close up. If this happens, surgery may be required to
reopen the stoma.
What if the tube becomes plugged?
This is most often caused by the build-up of formula residual in the lumen (internal space or
opening that exists within the gastrostomy tube). Tube blockage may be prevented with the routine
practice of flushing the tube after each use. The tube should be flushed at least once daily. Although
water is good, coke or other carbonated beverages are even better. If blockage occurs the tube
should be irrigated using a large bulbed syringe. Be careful to avoid excessive force while irrigating
73
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
because the tube could rupture. Milking the tube may help dislodge the obstruction. Should these
attempts to remove the obstruction fail, notify the physician immediately.
What about oral hygiene?
Good mouth care is imperative in preventing problems, especially with patients who are provided
with total nutritional support through the PEG tube. Daily brushing of the patient's teeth, gums and
tongue should be done. Mouthwash may be used with patients who retain a gag reflex. The patient's
lips should be moistened with water and, if necessary, lubricated with petroleum jelly to prevent
cracking.
Food and Medications
What kind of food is fed through the g-tube?
Commercial food: It is usually recommended that a commercially available prepared (canned)
formula and water for hydration be fed through the tube. This will provide a balanced diet including
all the essential vitamins and minerals needed. Some of these formulas contain fiber so that regular
bowel movement can be maintained even if you are unable to eat fruit, vegetables and other high
fiber foods. It is important to understand that nutrition is a very critical to the continued well being
of the ALS patient. Because of the need to make commercial brands of food supplements taste good
to the public, they are high in fat and sugar content. Over a prolonged period of time excessive fat
and sugar are not good for the human body. If the patient is getting the bulk or all of their nutrition
from supplements, it is suggested that you work with a dietitian to find a high content formula. The
best formula is likely one that is not commercially available through retail outlets. The formula
comes commercially prepared or in powder form which requires dilution with water. Common
brands, typically with or without fibers, include Ensure, Jevity, NuBasics, Boost, and Isocal among
others. Most come in 8 oz. cans and contain 250 calories.
Table Food: Table foods may be blenderized according to instructions from the physician. Many
people use homemade formulas prepared from cooked, blenderized foods but caution should be
used to prevent clogging the tube in the stoma itself. Most tubes are roughly the size of a straw in
diameter. Therefore food would have to be liquidized to prevent clogging the tube. Old foods left in
tubing and other apparatus can lead to infection, therefore adequate cleaning is necessary. Specific
advice with respect to the type of food and the quantity required should be provided by your doctor
or a dietician.
How much formula should be given?
This is determined by your medical advisors and is dependent on many factors. The physician will
advise the patient/family on the type of food, methods of feeding, frequency and rates.
How do you take medications?
Medications may be administered through the tube utilizing the bolus feeding method. The
physician or pharmacist should be asked for liquid medication where possible verses pills or
74
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
capsules. If liquid medication isn't possible, certain tablets and pills may be dissolved in 30cc to
50cc's of water. Formula, juice or milk may be used if the medication does not dissolve in water.
Highly viscous liquids (sticky, gummy, gelatinous liquid like CO-Q10) should be diluted with water
prior to administration. It is recommended that a physician or pharmacist be consulted for questions
regarding medications and/or the administration of medications, as certain medications should NOT
be crushed or dissolved. Following the administration of any medication, the tube must be flushed
with 30cc to 50cc of water. DO NOT give bulk laxatives through the tube without consulting with
the physician first as some laxatives may obstruct the PEG tube.
Feeding
Will I use the g-tube at normal mealtimes?
The g-tube can be used at anytime that suits the individual. The feed can be given by attaching a
syringe to the tube and pouring in the feed or by using an electric pump, so that feeds can be given
without the person or helper needing to do anything during the meal. Some people choose to stick to
regular mealtimes, while others use a pump and continuous feed to allow feeding to be done mainly
at night. Some families find that it is nice to sit down to eat together even though one of them is
getting their main meal through the g-tube. The person can sometimes be having a light snack at the
same time or just a drink. Each person's routine is individual and is decided on with all their needs
in mind.
Can I eat some normal food or drink by mouth?
It depends on why the tube was inserted. If it was because of slow mealtimes or poor weight gain
only, it is OK to continue eating and drinking as usual. In this way your mealtimes can be as long or
short as you wish as you know you can top up enough calories via the tube. Some people use the gtube mainly as "insurance" so that the person can always be sure of getting food and drink even if
they don't feel like eating by mouth.
However, if the reason for having the tube is that the person has swallowing problems and aspirates
on food or drinks, it is important to have advice on what is safe to take by mouth. The team may
recommend that only certain amounts or types of food or drink are safe by mouth. Sometimes it is
the safest option to stop taking food by mouth altogether. This is not a forever decision and the
swallowing will be monitored so alterations can be made as things change.
What if I am thirsty?
In some cases it is OK to drink normally. If the team has said that you cannot drink by mouth then
fluids added via the g-tube will reduce thirst.
What will it feel like while I'm being fed?
Most people don't notice anything at all. If an attempt is made to feed a person too quickly they will
soon complain of feeling sick, just as they would if they ate too much, too quickly. If this happens,
then the rate of feeding is easily reduced or stopped.
Will I still feel hungry, and then full after a feed?
75
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Yes. The stomach will still fill and empty in the normal way, giving the usual sensations of hunger
and satisfaction.
How should food or formula be handled?
The caregiver should thoroughly wash their hands with soap and water before preparing
formula/food and having contact with the patient. Formula should be given at room temperature
(too hot or cold would make patient uncomfortable). Unused formula and blenderized foods should
be refrigerated. Refrigerated formula and blenderized food should be warmed to room temperature
over a 30 minute period before feeding. NEVER heat the solution as this could increase the growth
of bacteria. In hotter climates, ice may be placed in the outside pocket of the full canister or bag for
overnight feeding, but be conscious of the discomfort caused to the patient, as some people with
buttons find cold fluid going into their stomach quite uncomfortable.
In what position should the patient be fed?
The patient should be fed in an upright position (at least 30 degrees) and remain in an upright
position for 30 to 60 minutes following the feeding. This minimizes the possibility of aspiration
(inaling food into the lungs) and its inherent complications (pneumonia). Overdistention, where the
abdomen becomes superinflated, should be avoided by careful attention to the rate of feeding flow
and the development of abdominal bloating. The doctor will recommend the measurement of
feeding and the flow to be used.
What is Bolous Feeding?
Bolous feeding is where the food is poured into the tube slowly verses by machine. Bolous feeding
allows you more freedom in that you can give feedings anywhere, which is nice when you leave the
house. Bolous feeding allows for rapid feeding of formula over a relatively short period of time.
Formula may be instilled using a bulbed or piston syringe or through the use of gravity flow. The
feeding usually consists of no more than 250 cc's to 500 cc's per feeding and is given to the patient
every 4 to 6 hours. Never FORCE fluids through the PEG tube. Infuse the formula slowly and
carefully to prevent abdominal cramping, nausea and vomiting, gastric distension (inflated stomach)
or diarrhea. If the formula is not infused (poured) slowly, the patient is placed at a high risk for
aspiration (fluid into the lungs) and the complications of pneumonia.
What is Continuous Feeding?
This method is preferable for many patients because it allows for better regulation of the amount
and rate of food. The feeding pump (a machine) is set up and the tubing connected to the PEG tube.
The formula is infused over the prescribed period of time into the patient. Using a feeding pump to
control the rate is normally better for digestion and causes fewer problems. Typically the slower the
rate of intake, the better the tolerance. The risk for aspiration is also decreased because less formula
is given during the prolonged period of infusion.
What is the purpose of the alarm on the pump?
The alarm may sound to let you know the pump is running on the battery instead of the power point.
It also warns of a blockage in the flow (check to make sure the clamp and roller brake are off), a
76
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
kink in the tube (check under the patient, also the tube between the canister and where it enters the
pump), and that the canister is empty of formula.
How do I clean the equipment?
After each feeding, flush the tubing with lukewarm water to clear the tubing and wash away any
particles that might clog the tube. Remember, don't flush the tubing with chilled water. If you use a
canister type apparatus to hold the formula, scrub the inside with a brush and warm sudsy water.
Plastic bags such as those for the Kangaroo pump (and similar pumps) are designed to be used for
24 hours then thrown away. Some people clean them thoroughly then use them for another 24 hours
but caution must be exercised when doing this, as the threat of infection exists. Flushing the tubing
with boiling water helps get rid of stubborn particles (after the tubing is removed from the patient!).
Some people advocate the use of a carbonated drink such as Coca Cola to clean the tubing. Running
a small amount through the tubing may help remove crusted formula.
What can be done about abdominal gas?
Trapping of gas in the stomach is sometimes a side effect of tube feeding. Massaging of the
abdomen can sometimes help, as can bending the knees up to the chest. Also try rolling onto one
side or other to allow the gas to be dispersed. Should the patient experience bloating prior to or
following any feeding, the patient's stomach and intestinal tract should be decompressed.
Decompression is easily accomplished by removing the feeding adapter cap from the tube and
allowing the PEG tube to be open to air. Encouraging the patient to cough will expedite the removal
of excessive air. It is a good idea to put the bolous tube into the PEG before the patient cough's or
burps to prevent the contents from splattering out all over.
Summary
The care of the tube and the feeding sound like a lot of work, but it really isn't. At first you swear
you will never remember all of the steps necessary for each procedure!! It is a good idea to take
notes and develop a checklist to use for the first week or so but you will find that you will quickly
be able to do it from memory.
77
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
BiPAP/Ventilation
Assistance for Breathing Problems
Pulmonary health is a significant issue. It is important for ALS patients to learn about mechanical
ventilation by getting good information and talking to peers. Then, when the situation presents
itself, a person can make an informed decision. This report presents the identifying signs of
pulmonary insufficiency and a variety of available options.
The Respiratory System
The primary functions of the respiratory system are to bring oxygen into the lungs, transfer the
oxygen to the blood, to expel the waste product called carbon dioxide, and to help regulate acidbase balance. Oxygenated blood travels from the lungs through the pulmonary veins and into the
left side of the heart, which pumps the blood to the rest of the body. Oxygen-depleted, carbon
dioxide-rich blood returns to the right side of the heart and is pumped through the pulmonary artery
to the lungs, where it picks up oxygen and releases carbon dioxide.
Because the lungs have no muscles of their own, the work of breathing is done primarily by the
diaphragm and, to a lesser extent, by the intercostal muscles (between the ribs). During forced or
labored breathing, other muscles in the neck, chest wall, and abdomen also participate. As the
diaphragm contracts, it moves down, enlarging the chest cavity. This reduces pressure in the chest
and air rushes into the lungs to equalize the pressure. The diaphragm then relaxes and moves up; the
chest cavity contracts and raises the air pressure. Air is pushed out of the lungs because of their
elasticity. The intercostal muscles participate in this process, especially if breathing is deep or rapid.
When everything is working well a person hardly notices that he is breathing.
Symptoms
Breathing problems can sneak up on ALS patients because they may not be easily identified. Is your
answer “Yes” to any of these questions?
•
•
•
•
•
•
Are you experiencing increased fatigue?
Do you frequently awaken with a headache?
Are you having problems sleeping?
Do you need to use additional pillows when sleeping?
Do you sleep better in a recliner or chair than in your bed?
Do you have a poor cough or difficulty clearing secretions?
If your answer was “Yes” to any of these questions, then it is probably time for a breathing
evaluation. If your answer to all of the questions was “No”, it is still important to educate yourself
about possible breathing difficulties in ALS patients so that you will be able to recognize a problem
if it does occur.
78
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
Self-Help
It is critical to have an effective cough. The strength of a person's cough can be assessed with a
Peak Flow Meter (cost $15-$30). The individual takes a deep breath and then coughs forcefully into
the Peak Flow Meter. A “peak cough flow” reading of less than 180 liters/min. indicates a weak
cough, according to John R. Bach, MD. A cough can be improved by:
•
•
•
•
Using huff coughing (not the high force cough, but repeated gentler huffs to bring up secretions)
Using the breath stacking technique (while using a mechanical breathing aid, hold your breath
after one or more inspiration cycles and add the air from the next inspiration cycle), or with frog
breathing (GPB). Examples of mechanical devices used for this are an Ambu-type resuscitator
bag and a volume ventilator.
Manual cough assistance methods (having someone push on your upper abdomen as you cough)
Devices to improve cough and clearance of secretions, such as Emerson's CoughAssist device,
formerly known as the In-Exsufflator [J.H. Emerson Co., Cambridge, MA (800) 252-1414]
If breathing muscles are weak because of ALS do not use up your energy on exercising to improve
their strength. It is unlikely to help. However, the ability of the lungs to expand should be
maintained. Using a chest inflation machine, learning how to take a deeper breath, and
glossopharyngeal breathing (GPB) – sometimes called “frog breathing”, can help maintain the
ability of the lungs to expand. GPB can augment the volume of air you breathe in; it is an important
survival skill to learn if your respiratory muscles are weak.
Use of a Continuous Positive Airway Pressure (CPAP) machine may also require increased work
for the expiratory breathing muscles. The CPAP was developed during the 1980s to keep airways
open for people with sleep apnea. During the 1990s cyclical inspiratory pressure was added to this
equipment and the Bilevel Positive Airway Pressure (BiPAP) came into use. The BiPAP assists
inspiration. Bilevel equipment is made by a number of manufacturers. When respiratory muscles are
weak due to PPS, a bilevel device would usually be better and safer than CPAP even if a sleep study
shows sleep apneas.
Avoid poor nutrition. Unless your muscles get the required amount of nutrition as well as oxygen,
they will function less effectively and any weakness will become increasingly noticeable. If a
person has lost weight and become frail, finding ways to build up his nutritional status will help, in
terms of his immune status and muscle function, as long as he doesn't become overweight.
Sleep Study
Sleep aggravates weak breathing muscles and developing respiratory failure. Thus more breathing
problems occur at night. If daytime breathing tests are within normal range, a simple over-night
oximetry study can be done at home (this continuously records pulse and oxygen saturation).
Sometimes a more expensive and elaborate over-night sleep study is needed. During this procedure
a patient is connected to many measuring devices and when indicated, assistive breathing
equipment may also be used to decide its effectiveness and to determine the proper settings. During
REM sleep (deep “rapid eye movement” sleep) accessory breathing muscles and other voluntary
79
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
muscles become so relaxed they are sometimes referred to as paralyzed. That is why breathing
problems are first noticed during REM sleep because at that time breathing becomes completely
dependent upon the patient's diaphragm, which may be weak due to ALS.
Bulbar Impairment
When an ALS patient has bulbar impairment there is a triple threat: weak respiratory muscles, a
poor cough (which can lead to development of infection and pneumonia), and the risk of food
aspiration.
Choices
Choosing Home Mechanical Ventilation (HMV) is conditional upon:
•
•
•
•
•
Quality of life is worthwhile.
Physician presents the options.
Resources are available (particularly care giving).
Social support is available for HMV (hand in hand with medical support).
Benefits outweigh the burdens.
Most people in the United States think of a ventilator as evil equipment. So without any advance
education most would choose to withhold using a ventilator when deciding in advance. However,
95% of those who are already on HMV, want to remain on it. So it is important for everyone to
learn about HMV by getting good information and talking to peers. Then, if the situation presents
itself later, a person can make an informed decision. An ALS patient who is having breathing
problems has four choices:
1.
2.
3.
4.
He/She can decline assisted ventilation and use only palliative care.
He/She can use only non-invasive Nasal Positive Pressure Ventilation (NPPV), such as BiPAP.
He/She can use assisted ventilation only for acute episodes such as pneumonia.
He/She can use whatever ventilation support is needed for long-term survival, including trach
positive pressure ventilation if needed.
By providing experience with noninvasive ventilatory equipment (such as BiPAP) before a crisis
occurs, the patient will then have the ability to survive an acute respiratory infection if it does
develop. And, this also provides a “hands on” trial of the equipment to help decision-making (like a
“test drive”). The goals of HMV are to integrate the individual back into the community, avoid
creating a hospital ICU environment, and avoid technological entrapment.
80
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
When should a person begin using Nasal Positive Pressure Ventilation (NPPV)?
If a person needs to use more pillows to elevate his head in bed, or prefers to sleep in a chair or a
recliner, or his legs begin to swell, these symptoms may be enough motivation to begin using
ventilatory equipment. Physiologic tests should confirm that chronic respiratory failure is
developing. Any one of the following confirmatory tests justify starting NPPV:
•
•
•
A person's vital capacity (VC) is less than 50%, although Dr. Oppenheimer said that he might
start NPPV if the VC is 60%; or
The maximal inspiratory and expiratory pressure readings are less than 50 cm. of water; or
If nighttime oximetry shows evidence of under-ventilation, with periods of low oxygen
saturation of 88% or less for at least five minutes.
The old criteria used abnormal Arterial Blood Gas (ABG) values as a determinant. Regulatory
agencies prefer tests like ABG tests which cannot easily be gamed (data manipulated to justify
NPPV equipment). But ABG values are often abnormal “too late”, just when a respiratory failure
crisis is occurring.
Oxygen
Initially the goals of NPPV are to relieve symptoms, normalize sleep, provide experience with
NPPV as hours of use gradually increase (see if you like it), prepare for the ability to survive acute
respiratory infection, and maintain blood oxygen (O2) saturation levels at 95% without added
oxygen. When the ventilation device is working properly the carbon dioxide (CO2) is eliminated
and the patient's oxygen level is high; with improper ventilation the patient's oxygen level drops. If
a person is not getting enough breathing support the CO2 level will climb and leave less room in the
lungs for oxygen, so the O2 level falls. If a person wants to monitor oxygen levels himself, Dolly
Bodine, RRT, a representative of Mallinckrodt (Puritan-Bennett) and Dr. Oppenheimer recommend
the Nonin brand's ONYX finger pulse oximeter (it is small, accurate, and less expensive): 800-3568874. Often this is not covered by health plans or Medicare.
What blood oxygen levels are normal? Readings of 95% (at sea level but lower at higher elevations)
and nocturnal desaturation episodes as low as 90% may be normal. Nocturnal oxygen saturation of
88% or less is abnormal. When blood oxygen saturation levels are below 85% you enter the danger
area; below 75% you are in the disaster area.
“Some situations may require administering oxygen, such as pneumonia due to infection or
aspiration. If this occurs in patients with respiratory muscle weakness and hypoventilation, then it is
important to provide both assisted ventilation and supplemental oxygen, and use ABGs to monitor
them.”
81
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
“Administering oxygen does not provide assistance to the weakening respiratory muscles. It gives
both the patient and the doctor the false impression that appropriate treatment is being provided,
while in fact hypoventilation is mistaken for an oxygen transfer problem. Indeed, administering
oxygen can mask the problem. Also there is a danger of causing respiratory depression by giving
oxygen. Oxygen is NOT the treatment for hypoventilation. It will improve the SaO2 (oxygen
saturation level in the blood), but not the hypoventilation and may increase the danger of dying of
sudden respiratory failure.”
After an abnormal sleep study shows decreased oxygen levels, some physicians naturally want to
prescribe oxygen. A study by Peter Gay, MD (Mayo Clinic) concluded that the use of oxygen could
turn off a person's respiratory drive (and death can occur as a result).
Care Plan for using Nasal Positive Pressure Ventilation
Considerable expertise is required to set up NPPV equipment effectively and comfortably. Frequent
follow-up is needed, similar to that of a person who has a trach. The interface (mask, nasal pillows,
etc.) should be checked and the effectiveness of assistive ventilation determined. Objective
assessment includes examining the patient, checking the equipment, making sure that the oximetry
is 95% or better (without added oxygen), and sometimes doing overnight oximetry monitoring.
Regular follow-up is important.
With a bilevel ventilator, initially the inspiratory positive air pressure (IPAP) setting on the machine
may be at 8 to 10 cm. of water, but this setting often needs to be gradually increased to between 1416 cm. Persons with scoliosis may require an even higher setting. Initial expiratory positive air
pressure (EPAP) setting will be about 3-4 cm. and usually will not be changed.
Safety issues are critical. The person using ventilatory equipment must learn all the equipment
problems that could possibly develop and know how to fix them. Regular safety drills should be
done with all caregivers so they will have the same knowledge. If these safety issues are neglected,
a person using ventilatory equipment leaves himself open to possible catastrophe. An Ambu-type
resuscitator bag should be available.
Tracheostomy?
A tracheostomy should be considered if NPPV fails, if the person has a problem with secretions
and/or prefers a trach, or when long-term survival is important. Safety may be better with a
tracheostomy when daily 18 to 24-hour ventilator life support is needed. Does a trach ventilator
provide the most effective ventilation? The BiPAP also provides effective ventilation, but neither is
perfect. Dr. Oppenheimer advises that if a trach works for you keep it, no matter what any physician
tells you. Doctors' opinions will vary on this matter. If you have a trach you should also have a good
suction machine. More suctioning may be required during the first year while the trach heals and
matures. (Medicare may cover the monthly rental charge of about $30.00 until the machine is paid
off in a year or two.)
82
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
In the Future
There are some people who function better with volume ventilators and nasal masks rather than
bilevel equipment. New equipment will be combining the advantages of both types of equipment.
Smart BiPAP machines are now being developed. These machines will have the ability to recognize
what a person needs and automatically adjust the settings accordingly. New alarm features on the
BiPAP will compare favorably to the safety features of a volume ventilator. Improved nasal and
full-face interfaces (masks) are becoming available. A straight or angled, or lipseal mouthpiece is
useful for many, and is important to have in case of nasal congestion during a common cold or
allergy.
Conclusion
There are many benefits from Nasal Positive Pressure Ventilation:
•
•
•
•
•
•
•
It provides muscle rest and recovery at night.
It helps reset the CO2 sensitivity in the respiratory control system.
It probably improves respiratory mechanics.
It helps with periods of low oxygen and helps prevent acidosis.
It improves the quality of sleep.
It can improve cough and swallowing.
It improves long-term survival.
Fortunately the outlook today for mechanical ventilation is better than it was ten years ago because
now there are more physicians and respiratory therapists who are familiar with the new noninvasive
ventilatory equipment that is available.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
This article was reprinted with permission from Edward Anthony Oppenheimer, MD, FCCP. It is
based on a report written by Mary Clarke Atwood with editorial assistance from R. Daggett, V.
Duboucheron, and E. A. Oppenheimer, MD, FCCP. Minor modifications were made to the article
so that it applies particularly to PALS, since it was originally developed for polio survivors. The
original report was based upon a presentation by Dr. Edward A. Oppenheimer, MD, FCCP, to the
Rancho Los Amigos Post-Polio Support Group on March 24, 2001. He had just returned from the
Eighth International Conference on Home Mechanical Ventilation held in Lyon, France. Dr.
Oppenheimer is Associate Clinical Professor of Medicine, University of California, Los Angeles
(UCLA). He retired after 31 years with Kaiser Permanente Medical Group where he organized and
coordinated the Kaiser home ventilator program.
83
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
When to Start BiPAP
By Edward Anthony Oppenheimer, MD
The question of when to start BiPAP is important. There are clinical research studies going on now
to get more information, and to determine if starting earlier has definite advantages (from my
experience, I believe that it is better to start earlier).
If there are respiratory symptoms due to ALS respiratory muscle weakness, and an abnormal result
of any one of the following tests, then starting noninvasive ventilation (such as BiPAP of VPAP) is
justified and advised. There are many possible respiratory-related symptoms, such as: fatigue,
shortness of breath, difficulty breathing lying down, poor cough, morning headache, etc.... The
usual practice is to measure:
•
•
•
•
Vital Capacity (VC)
Maximal Inspiratory Force (MIF)
Over-Night Oximetry. - This is the test most likely to be abnormal early, before other
tests are abnormal.
Arterial Blood Gas (ABG) - This is the test most likely to only be abnormal very late.
(possibly too late)
If any one of these tests is sufficiently abnormal, then starting bi-level ventilation is justified and
will be reimbursed by Medicare and/or most health plans/insurance programs (if there are any
respiratory symptoms present):
•
•
•
•
VC of 50% or less
MIF of 60 cm water or less
Arterial CO2 of 45 mm Hg or greater
Nighttime oximetry that demonstrates oxygen saturation less than 88% for at least five
continuous minutes, done while breathing room air (or breathing the patient's usual
added oxygen level).
Starting even earlier may be an advantage as it often takes time to learn to use the equipment and
develop comfort with it. If there is an unexpected respiratory infection (even just the "common
cold") a person skilled using this equipment can often manage to get through it safely without
hospitalization.
Dr. John Bach suggests using both the peak cough flow (PCF) and an oximeter for home
monitoring. If the PCF drops below 300 lpm (using a simple peak flow meter to measure PCF), then
training in assisted cough methods should be started. If a person is using a bi-level ventilator (such
as BiPAP or VPAP), Dr. Bach advised adjusting the setting for both comfort and to maintain the
84
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
oximetry oxygen saturation at 95% or better (without using added oxygen). You need to have a
good home equipment company with respiratory therapists experienced in this equipment and
assisted cough techniques. They need to be able to take plenty of time to set-up the equipment
properly, follow-up carefully, and stay in close contact with your doctor.
Please discuss any medical care issues with your own physicians. An email can give general
information; only your physician can give you reliable personal medical advice based on examining
you and knowing your full medical record.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
This article is based on a February, 2002 email response by Dr. Edward Anthony Oppenheimer,
MD, FCCP to a question posted to the Living-with-ALS email discussion group on Yahoo Groups.
Dr. Oppenheimer is Associate Clinical Professor of Medicine, University of California, Los Angeles
(UCLA). He retired after 31 years with Kaiser Permanente Medical Group where he organized and
coordinated the Kaiser home ventilator program.
BiPAP Setup
By Edward Anthony Oppenheimer, MD
The following would be my usual approach (to achieve an ideal outcome), adjusted to the needs of
each person. Only your physician, who knows you and has examined you, can responsibly advise
you on your care. These comments therefore are of a general nature, and not treatment advice.
In an ideal world you would have a home equipment company with respiratory therapists (RT) who
are very experienced in setting-up BiPAP equipment, and have plenty of time for initial return visits
and for regular follow-up visits. Comfort is the first priority. The interface to connect the breathing
equipment to you should be the right size and the strap tension adjusted properly for comfort and to
avoid major air leaks. I usually suggest having both a good nasal mask and the nasal pillows, so you
can alternate. Many people have to try different types of mask to find one that is really comfortable.
The initial settings are often an EPAP (expiratory positive airway pressure) of 3-4, and an IPAP
(inspiratory positive airway pressure -- this is what inflates the lung with each breath) of 8 to 12 cm
water. Again, comfort is most important and the RT should adjust the interface and the setting to be
comfortable. After you get used to the equipment, the IPAP is usually gradually increased to about
14-16 cm water over weeks or months.
The purpose of the equipment is to assist breathing, improve the lung's air exchange, relieve
respiratory muscle fatigue, and relieve respiratory symptoms; and to allow a good night's sleep. A
simple oximeter should be used to make sure that you achieve an oxygen saturation of at least 95%
on the Bipap, without added oxygen. If the oxygen saturation is below 95%, and this is not due to
airway secretions, then the IPAP usually needs to be increased. The rate can be set so that at night
the machine automatically cycles to give a comfortable normal breathing rate (perhaps about 12 to
85
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
14 breaths/minute -- whatever is comfortable) so you do not need to constantly trigger the BiPAP
with your breathing effort for each breath; however you can always take extra breaths if you wish.
The physician and the RT need to coordinate so that the equipment and settings reflect what is
comfortable and effective for you. Both an oximeter to check oxygen saturation, and a peak flow
meter to check peak cough flow, are useful (probably essential) for home monitoring. If the peak
cough flow is less that 300 lpm, then assisted cough techniques need to be learned. Respironics has
various models of the BiPAP, and ResMed has the VPAP, and there are other choices as well for
small portable home ventilation. Many people find that the first equipment advised works just fine
for them, while some find that they do much better with another similar home ventilator.
Networking with other PALS who use the BiPAPor VPAP, or similar devices, helps a lot. There are
a lot of details and resources available. It is normal to take a while to get used to the equipment, but
essential to have the right equipment - - set-up and adjusted properly.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
This article is based on a March 3, 2002 email response by Dr. Edward Anthony Oppenheimer,
MD, FCCP to a question posted to the Living-with-ALS email discussion group on Yahoo Groups.
Dr. Oppenheimer is Associate Clinical Professor of Medicine, University of California, Los Angeles
(UCLA). He retired after 31 years with Kaiser Permanente Medical Group where he organized and
coordinated the Kaiser home ventilator program.
Not Choosing Ventilation
By Edward Anthony Oppenheimer, MD, FCCP
If respiratory muscle weakness is not effectively assisted with mechanical ventilation, then the
under-ventilation results in increasing CO2 levels and decreasing oxygen levels. This acts as a
sedative and has been referred to a carbon dioxide narcosis: one essentially goes into a deep
undisturbed sleep as the end of life occurs. This can occur when:
1. no equipment (such as BiPAP or VPAP) is used;
2. when noninvasive equipment (such as BiPAP or VPAP) is no longer providing effective
ventilation;
3. when a person decides to stop using assisted ventilation;
4. when using a bilevel ventilator (such as BiPAP or VPAP) but the IPAP setting is too low, so
that under-ventilation occurs - people should monitor themselves by checking to be sure
oximeter readings are 95% oxygen saturation or better (without using oxygen) at night and
during the day.
When there is a decision that end-of-life is desired (situations such as 1-3 above), then palliative
care assistance provides additional help with medications that can be used, when needed, to be sure
86
Revised 1/30/2009
24359 Northwestern Hwy. z Suite 100 z Southfield, Michigan z 48075 phone 800.882.5764 z email alsofmi@alsofmi.org z website www.alsofmi.org
there is no discomfort from apprehension, respiratory distress, gagging, difficulty with secretions,
etc...
There are PALS who develop more severe bulbar impairment and weak ability to cough. When
bilevel noninvasive ventilation is used (such as BiPAP or VPAP), there may come a time when
inability to clear airway secretions makes this type of assisted ventilation fail. Assisted cough
techniques (manual or using the CoughAssist device) help considerably for quite some time.
However, at some point, bulbar and cough impairment become too severe to allow successful
noninvasive ventilation. This is the point when one either switches to tracheostomy ventilation or
elects palliative care (plan this well in advance of trouble, of course). At this point people can
experience respiratory and gagging distress as they try to use their bilevel noninvasive ventilation
(such as BiPAP or VPAP).
Therefore I strongly advocate preparing in advance, and if tracheostomy is not desired, have
medications and assistance available so that comfort is assured; so that distress is avoided. Do not
wait to react at the last minute, be prepared. You should have support from your physician, a
palliative care doctor, or hospice. Some people who say for a long time that they do not want to use
tracheostomy ventilation, change their mind later. And, most PALS who do use tracheostomy
ventilation (who can arrange the needed resources) say they are satisfied and would do it again, if
they had a choice to do it again.
In general, at good medical centers in the USA, about 20-30% of PALS use bilevel noninvasive
ventilation (such as BiPAP or VPAP). There is a wide range from almost zero to 40-50%; in great
part this reflects the differences in the attitude and experience of the healthcare professionals. Only
4-5% of PALS in the USA use tracheostomy ventilation; again there is a wide variation. However
most PALS decide that when BiPAP is no longer effective, that is the time to stop. These numbers
are approximate and are changing with time (more PALS use assisted ventilation today than in the
past).
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
This article is based on a February 17, 2002 email response by Dr. Edward Anthony Oppenheimer,
MD, FCCP to a question posted to the Living-with-ALS email discussion group on Yahoo Groups.
Dr. Oppenheimer is Associate Clinical Professor of Medicine, University of California, Los Angeles
(UCLA). He retired after 31 years with Kaiser Permanente Medical Group where he organized and
coordinated the Kaiser home ventilator program. Although Dr. Oppenheimer is no longer seeing
people in office practice and does not have an office referral, he will try to respond to comments
and questions emailed to him at Eaopp@UCLA.edu.
87
Revised 1/30/2009