1 Pain as a Public Health Challenge The BIOMEDICAL Model The
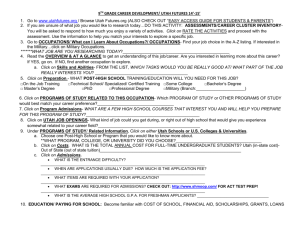
advertisement

The University Of Utah Department of Physical Therapy The Biopsychosocial Approach to Functional Improvement Julie M. Fritz “Pain represents a national challenge. A cultural transformation is necessary to better prevent, assess, treat, and understand pain of all types.” Professor, University of Utah Clinical Outcomes Research Scientist Intermountain Healthcare Salt Lake City, Utah, USA The University of Utah Department of Physical Therapy Pain as a Public Health Challenge The BIOMEDICAL Model • Affects at least 116 million American adults • Significant reductions in quality of life • Costs to society $560–$635 billion annually Pain as a sensory event reflecting underlying disease or tissue damage • For many pain prevention, assessment, and treatment are inadequate. • Need to improve provider education in a manner consistent with current pain science. Injury/ Nocioception Tissue damage Pain The University of Utah Department of Physical Therapy The BIOMEDICAL Model Pain is solely explainable in biological or medical terms Mental or emotional problems may result from chronic pain, p but the pain p itself is biological g in origin Effective treatments for pain involve medical approaches (ie, address the pathoanatomical source of the pain) The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders Cognitive/ Behavioral Consequences The University of Utah Department of Physical Therapy The BIOMEDICAL Model TREATMENT IMPLICATIONS Signs and symptoms are directly proportional to the underlying pathology Identifying the underlying pathology is critical for guiding treatment Signs and symptoms should disappear when pathology is corrected The University of Utah Department of Physical Therapy 1 Increasing Rates of Back Injections The incidence of common symptoms in primary care and the proportion found to be due to organic disease. Friedly J. Spine 2007;1754-1760 Adapted from Kroenke and Mangelsdorff, 2001) The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Chronic LBP Prevalence by Age Category The BIOPSYCHOSOCIAL Model 18 16 Clinical expression of pain encompasses numerous aspects besides physical dysfunction: 14 percentage 12 10 8 Over 70% increase in medical di i d expenditures over same period 1992 2006 Social & Vocational Environment Behaviour Emotional Distress Emotional distress Attitudes & Beliefs Attitudes and beliefs 6 The social environment 4 Illness behavior of patient PAIN 2 0 >65 The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Evidence for the Biopsychosocial Model The BIOPSYCHOSOCIAL Model The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders No disability Henschke et al. BMJ (2008) 0.4 ye ar 1 on th s m 6 m on th s 0.2 w ee k m s on th s 1 ye ar 0.2 0.6 3 Cumulative probability of still having pain 0.4 0.8 6 0.6 m on th s Outcomes of treatment depend on management across domains of the model 0.8 m on th s Knowledge of cause of pain is not sufficient to determine its impact (or legitimacy). 1.0 1.0 9 Pain (particularly when chronic) is rarely the only presenting symptom (although may be the only one recognized). Follow up at 6 weeks, 3 months, and 12 months Cumulative probability of still having disability The relationship between tissue damage and pain is variable and unpredictable Inception cohort study of 973 patients presenting to primary care with LBP < 2 weeks duration 6 MANAGEMENT IMPLICATIONS 9 55-64 6 45-54 w ee k m s on th s 35-44 3 21-34 Freburger et al, Arch Int Med, 2009 Pain-free The University of Utah Department of Physical Therapy 2 Yellow flags Yellow Flags (adverse prognostic factors) Inappropriate attitudes and beliefs about back pain Older age (e.g, belief that back pain is harmful or potentially severely disabling or high expectation of passive treatments rather than a belief that active participation will help) More intense pain Longer g duration of low back pain p Patient reports feeling depressed Patient believes pain is likely to persist Work related problems or compensation issues (e.g., poor work satisfaction) Emotional problems (e.g, depression, anxiety, stress, tendency to low mood and withdrawal from social interaction). Compensable low back pain The University of Utah Department of Physical Therapy Henschke et al. BMJ (2008) Inappropriate pain behaviour (e.g., fear-avoidance behaviour and reduced activity levels) More days of reduced activity MANAGEMENT IMPLICATIONS SCREENING From van Tulder et al, 2006: European guidelines for the management of acute nonspecific The University of Utah low back pain in primary care Department of Physical Therapy Early identification of patients more likely to develop persistent disabling symptoms could help guide decisions regarding follow-up and management. Because individual risk factors are relatively weak, risk prediction instruments could be more helpful than individual yellow flags for predicting outcomes. More research is needed to understand the clinical usefulness of risk prediction instruments for identifying high-risk patients and the optimal strategies to decrease the likelihood of chronic disabling back pain. The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Multi‐Construct Screening Tools for Individuals at Risk of Persistent LBP Distress and Risk Assessment Method Vermont Disability Prediction Questionnaire Örebro Musculoskeletal Pain Questionnaire (Acute Low Back Pain Screening Questionnaire) StartBack Screening Tool 9-item tool comprising modifiable prognostic factors of both physical and psychosocial constructs Stratifies risk for developing future disabling LBP –Low Risk (few barriers to recovery) –Medium Risk (predominantly physical barriers to recovery) –High Risk (psychological barriers to recovery) The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders The University of Utah Department of Physical Therapy 3 FEAR AVOIDANCE ANXIETY Psychological Barriers to Recovery CATASTROPHIZING High Risk Psychologically-Informed Therapy DEPRESSION Physical Barriers to Recovery BOTHERSOMENESS Medium Risk Physical Therapy Minimal Barriers to Recovery Low Risk Advice and Reassurance The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Clinical Journal of Pain Clinical Journal of Pain Objective – Evaluate agreement between clinicians and the SBST’s risk allocation ll ti Methods: – 12 patients: video recorded clinical exam including SBST – Video reviewed and independent risk allocation 3 General Practitioners 3 Physical Therapists Results – Interrater agreement: Fair (k = .28) – Observed agreement with SBST 17/36 (weighted k = .22) Conclusion – Clinicians make inconsistent risk estimates – Little agreement with formal tool 3 Pain Management Specialists The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy 858 patients with LBP in primary care Randomized to receive: – Stratified management based on SBT – Usual Care (control) High Enhanced Physiotherapy Medium risk Physiotherapy Low risk GP/best practice care The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders 4 average lost work days 14 12 10 8 6 4 2 0 Control Intervention Low Risk Medium Risk High Risk From an economics perspective, the stratified management approach was associated with improvements in health-related quality of life (QALYs), a reduction in health-care use, and fewer days off work related to back pain. What is Psychologically‐Informed Practice? Main C J , George S Z PHYS THER 2011;91:820-824 Educational Interventions Proposed theoretical framework for the management of low back pain by physical therapists – Advantages of remaining active – Favorable expectations – Problem-solving/coping strategies Cognitive Behavioral Strategies: –Graded Exposure to worrisome activities –Graded Activity Goal setting Positive reinforcement The University of Utah Department of Physical Therapy MESSAGES MATTER “Back Pain: Don’t Take It Lying Down” Disability from LBP is a public health problem In Victoria, Australia back pain accounted for… 25% of all claims account for workers –25% workers’ compensation –40% of long-term disability claims –Nearly 50% of the total costs of all claims Compensation costs for LBP had tripled in the past 10 years The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders The University of Utah Department of Physical Therapy “Back Pain: Don’t Take It Lying Down” Attitudes and beliefs about LBP influence the development of long-term disability Societal beliefs may perpetuate maladaptive attitudes towards LBP – Both provider and patient beliefs contribute to the problem SOLUTION – public media campaign – Campaign was designed to alter the public’s beliefs about back pain, influence medical management, and ultimately reduce disability and compensation claims. The University of Utah Department of Physical Therapy 5 “Back Pain: Don’t Take It Lying Down” “Back Pain: Don’t Take It Lying Down” Campaign was based on the messages of The Back Book. – Unambiguous advice to stay active, avoid rest for prolonged periods and remain at work – Emphasized that the spine is strong, self-coping is important, imaging is usually not helpful, and surgery is usually not the answer. MEDIA MESSAGES Positive advice to stay active and exercise, not to rest for prolonged periods, and to remain at work; Encourage patients to take responsibility for getting better and coping; Advice that physical activity and work won’t cause harm Education that imaging may not be helpful and surgery is usually not the answer The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Maladaptive Provider Beliefs Assessed physical therapists on their biomedical vs biopsychosocial orientations towards non-specific LBP. Therapists with biomedical orientation viewed daily activities as more harmful for LBP patients Steeper declines in days and costs per claim for LBP vs. other complaints Absolute reduction in medical costs was 20% per claim Houben et al. European J. Pain 9 (2005) 173–183. The University of Utah Department of Physical Therapy Patient Education – Key Considerations Encourage maintenance of activity (hurt vs. harm) Reassure that serious pathology has been excluded Decrease patient’s focus on pain, shift to focus on function Cognitive‐Behavioral Therapies Integrated therapy that combines cognitive therapy (changing self-defeating thinking) with behavior therapy (changing behavior) Therapeutic strategies aimed at: Avoid “medicalizing” explanations, emphasis on need for imaging investigations – reducing maladaptive behaviors and increasing adaptive behavior Specific interviewing skills to identify potential psychological barrier – modifying maladaptive beliefs, attitudes, and expectations The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders The University of Utah Department of Physical Therapy 6 Cognitive‐Behavioral Therapy Goal-setting Patients with LBP (< 8 wks) Receiving Physical Therapy – short-term goals – long-term goals Shaping – Successive approximations – Gradual exposure to fearful activities Reward for goal attainment The University of Utah Department of Physical Therapy Biomedical Group Biopsychosocial Group • Classification-based management • Classification-based management • Exercise prescription based on limits of pain • Exercise prescription based setting goals and quotas • Education in anatomy and pathology of spine (Handy Hints pamphlet, reinforcement of message in clinic) • Education to remain active (Back Book pamphlet, reinforcement of message in clinic) The University of Utah Department of Physical Therapy Patient Education Biomedical group –Handy Hints pamphlet –Reinforce Reinforce this message in clinic Biopsychosocial group –Back Book pamphlet –Reinforce this message in clinic The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders 7 The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Exercise Progression Exercise Prescription Biomedical group Biopsychosocial group Specific to individual patient presentation – Based on pain intensity – Based on quota Exercise program components – Record initial pain intensity – Establish initial quota –Aerobic A bi – Perform exercise prescription – Perform exercise prescription –Flexibility – Record final pain intensity –Strength – Progress when pain intensity is the same or decreased – Progress when patient met pre-defined exercise quota Time limit = 1 hour The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Feedback Biomedical group Biopsychosocial group OSWESTRY SCORES 45 – Base explanations on anatomical model – Encourage positive expectations – Pain = pathology – Avoid anatomical explanations of pain 40 35 – Pain is a sign to limit activities – Interventions are a “progression” 30 25 – Regularly review clinic performance 20 15 – Positive feedback 10 Traditional Fear-Avoidance 5 0 Baseline The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders 4 weeks 6 months The University of Utah Department of Physical Therapy 8 Biopsychosocial group Traditional group Summary Movement from Biomedical to Biopsychosocial Model has been a “revolution”. The potential of the Biopsychosocial model to improve outcomes and reduce suffering has yet to be recognized. recognized Providers must revolutionize their own thinking and approach. This is a system problem Screening and targeting are critical to effective management. The University of Utah Department of Physical Therapy The University of Utah Department of Physical Therapy Thank You The University of Utah Department of Physical Therapy EMGO Institute - Common Mental Disorders 9