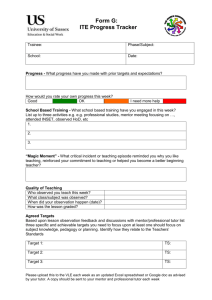
1 Introduction to the Portfolio
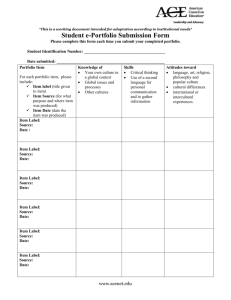
advertisement
KYN107 Faculty of Health & Social Care Introducing Professional Practice and Knowledge Guidelines for Completing the Common Foundation Programme Portfolio SUP 01592 5 *SUP015925* Copyright ª 2009 The Open University Pre-Registration Nursing Programme l 1.1 Common Foundation Programme Contents 1 Introduction to the Portfolio 5 1.1 Portfolio structure and assessment 6 1.2 How your practice is assessed 7 1.3 Programme curricular hours 9 1.4 Practice learning requirements 10 2 The Portfolio forms explained 13 2.1 Essential information 13 2.2 Self-assessment records 18 2.3 Evidence 19 3 How to complete your Portfolio 20 3.1 Types of evidence 20 3.2 Developing an evidence base 22 3.3 Guidelines on confidentiality 24 3.4 The three discussion meetings 25 3.5 Portfolio compilation and submission 29 References 32 Appendix 1 NMC outcomes 33 Appendix 2 Example of evidence written by a student based on a unit activity (UA) 41 Appendix 3 Example of testimony written by a practice supervisor (T) 43 Appendix 4 Peer testimony of student practice learning 44 Appendix 5 Example of a summary account written by a student (SA) 45 1 Introduction to the Portfolio 5 1 Introduction to the Portfolio Welcome to your Common Foundation Programme Portfolio. This is a record of your practice-based learning, underpinned by the theory you have learned during KYN100 or KYN101 and KYN107. You are responsible for the safekeeping of your Portfolio. You must at all times maintain the confidentiality of patients, clients and colleagues, and comply with current Data Protection legislation. (The government’s Data Protection website can be accessed from the Open University Library’s website.) You must ensure that your complete Portfolio is made available to each of your mentor/practice supervisors for all of your practice learning experiences. The material within your Portfolio, once submitted to the University, will be shared with relevant personnel associated with quality assurance, examination board processes and professional regulation. This information will be kept for the period of time prescribed by the Open University for assessment purposes. You must sign the declaration on the Ongoing Achievement Record in the Essential Information section of your Portfolio, indicating that you agree to share this information. Your Portfolio will contain the evidence that demonstrates that you meet the practice-based requirements of the Common Foundation Programme (CFP). It will contain records of your practice assessment as you work towards achieving the Nursing and Midwifery Council (NMC) outcomes necessary for you to progress to the branch programme of your choice. You will have an opportunity to discuss the Portfolio requirements with your programme tutor and your mentor in your practice setting. It is your responsibility to complete the Portfolio but your programme tutor and your mentor will work closely with you. You will also discuss the Portfolio with your programme tutor and your student colleagues during some tutorials. Your mentor is responsible for assessing your practice, and your programme tutor will verify whether your completed Portfolio meets the necessary criteria. This guide explains how to complete your Portfolio successfully. The forms for the Portfolio are provided as a separate item. You can photocopy and add extra sheets to any section of the Portfolio if you need to. When you submit the Portfolio do not include these guidelines; just submit the Portfolio forms indicated later in this guide. To demonstrate that you have met each NMC outcome, you need to provide supporting evidence in your Portfolio. You will collect this evidence in your Portfolio as the course progresses. You are not required to submit the supporting evidence on completion of the course, but this evidence will form the basis of each discussion meeting in which your mentor will assess your progress in achieving the required standard for completion of the CFP. At these discussion meetings, your programme tutor will sign to confirm that this discussion of your supporting 6 Guidelines for Completing the Common Foundation Programme Portfolio evidence has taken place. You should use the activities you complete in the course materials as evidence in your Portfolio. Each activity meets at least one NMC outcome and you can select which activities to include as evidence in your Portfolio. The activities also provide the foundations for your tutor-marked assignments (TMAs) and the examinable component, which you must submit at the end of the course. However, you can also provide other sorts of evidence in your Portfolio. For example, you may include sections of your journal. There is more information later in this guide about other types of evidence that can be included in your Portfolio. Each piece of evidence should have a sufficiently descriptive title so that the nature of the evidence is obvious. You should remember to give each piece of evidence a code and number (see Section 3.1) so that it can easily be located in your Portfolio by you, your mentor and your programme tutor. Note that you will also be required to produce and maintain further Portfolios during the branch programme. This will enable you to develop the necessary skills to maintain a professional Portfolio, which is a requirement of a registered nurse. 1.1 Portfolio structure and assessment The NMC divides practice into four domains within which you must achieve outcomes to enter the branch programme and standards of proficiency to complete the branch and register as a nurse. Your practice is assessed across these four domains, which are: 1 Professional and ethical practice 2 Care delivery 3 Care management 4 Personal and professional development. Your mentor will assess your performance in practice and the evidence in your Portfolio to demonstrate that you meet the NMC outcomes (Appendix 1). The assessment draws on two main sources: your coursework and your practice. Your coursework provides underpinning knowledge and understanding to inform your practice. It encourages you to become a reflective practitioner – to think about your practice in an insightful way and to learn from your reflection. You need to demonstrate your understanding of the coursework by relating it to your practice and vice versa. A good way of demonstrating this understanding is to include completed activities from the course in your Portfolio. Your Portfolio will record your assessment in practice supported by your Portfolio evidence for each NMC outcome and the summary of evidence of your practice experience and practice hours. All of this evidence, together with your successful completion of KYN100/101 and KYN107, will enable you to progress to the branch programme. Your mentor will observe your performance directly and assess it against the NMC outcomes to prove that you are developing your practice. Your mentor will also consider evidence about your performance from other sources. There is more information about this in Section 3. Each NMC outcome/standard of proficiency is sub­ divided into a number of ‘exemplars’ which illustrate how the 1 Introduction to the Portfolio 7 outcome/standard of proficiency can be met. However, please note that the NMC outcomes and standards of proficiency should only be assessed at outcome/standard of proficiency level. You must complete the Portfolio satisfactorily to pass KYN107. 1.2 How your practice is assessed Building on your previous experience, you will develop your skills, knowledge, understanding and judgement within your nursing practice. Your mentor will assess your ability to integrate theory with practice, so you must show them that relevant knowledge and theory underpin your performance in practice. This will enable you to demonstrate an understanding of the issues around your practice and your ability to contribute to holistic care. Your mentor will assess your progress towards achieving the NMC outcomes to complete the CFP, and the standards of proficiency to enter the NMC register (NMC, 2004), according to four levels of practice. These levels are based on research by Kathleen Bondy (1983). She studied the stages that students go through when developing competence. They are: Level 1 Constant supervision Level 2 Assistance Level 3 Minimal supervision Level 4 Independent practice. Table 1 (overleaf) gives the details of the knowledge and understanding, practice performance and professional development and awareness expected for each level of practice. By the end of the CFP, you must attain Level 2 in all of the NMC outcomes and provide evidence to support these achievements. You may be capable of Level 3 in some outcomes at this point. However, for the purposes of assessment, Level 2 is the requirement. Starting to work towards Level 3 in some outcomes will help you move towards this level in the branch. At the end of the branch, you must achieve Level 4 in all the standards of proficiency to enter the NMC register. Read the criteria for the four levels in Table 1 now and spend some time looking at the words which describe Level 1 more fully – ‘limited’, ‘basic’, ‘rudimentary’, ‘needs support’, etc. Check through the four levels (even though two of them refer to the branch). You will see that there is a definite sense of progress through them. At first the emphasis is on basic supported practice – ‘rudimentary’ and ‘lacks insight’. However, as you progress through the levels, there is more emphasis on insight, understanding and independence. Take some time to familiarise yourself with the levels and the demands each level will make on you. Use the levels and the description of the outcomes as a basis for discussion with your mentor, your programme tutor and your student colleagues: think about how you would distinguish between Level 1 and Level 2. Your mentor and your programme tutor can help you to identify what these differences are in practice and how you can progress from one level to another. 8 Guidelines for Completing the Common Foundation Programme Portfolio Table 1 Levels of practice Knowledge and understanding Practice performance Professional development and awareness Level 1 Needs constant supervision to deliver routine care Has limited knowledge but can identify where to locate further information Is not confident and lacks accuracy Does not adapt care to meet clients’ needs and current situation Has limited awareness of alternatives Needs constant supervision and guidance Provides basic explanation for rationale of choice selected Able to give rudimentary rationale for choice selected Needs support in organising work Does not prioritise care Lacks insight and awareness of professional self and professional behaviour Level 2 Needs assistance and can deliver routine care with some supervision Knowledge is usually accurate Performance is accurate but not always efficient and lacks confidence Adapts care to meet clients’ needs and current situation Begins to identify alternatives Needs frequent supervision and guidance Unable to deal with non-routine situations Can give rationale for actions Can prioritise care but often needs Gives standard explanations or does not qualify these or prompting explore other possibilities Level 3 Minimal supervision. Will need occasional supervision and support Applies accurate knowledge to practice Safe, accurate, and fairly efficient and confident Professional intervention or behaviour is generally appropriate for the care situation Has a limited range of alternatives Needs occasional support, supervision and guidance Rationale given for care is coherent and appropriate Begins to make judgements based on available evidence Beginning to initiate appropriate interventions Identifies need for assistance Prioritises care with minimal prompting Level 4 Able to work independently Applies evidence-based knowledge Safe, efficient and confident practitioner Shows awareness of alternatives Needs minimal advice and support Interventions and behaviour are suitable to the client and circumstances Sound judgement underpins actions Prioritises care Gives coherent, accurate and necessary information Decisions are based on current evidence Adapts to the current situation Identifies and makes appropriate referrals within multidisciplinary team (Based on Bondy, 1983) Careful, deliberate planning of care 1 Introduction to the Portfolio 9 1.3 Programme curricular hours The NMC requires pre-registration nursing programmes to comprise 4600 curricular hours equally distributed between theory and practicebased learning. Within the programme there are two categories of programme days or hours: l study days or hours l periods of supernumerary practice days or hours. Across the programme, each category is allocated a predetermined number of days or hours. Table 2 gives details of where these days or hours are located. Table 2 Allocation of curricular hours to learning activities Part of programme Study (days/hours) Supernumerary practice (days/hours) KYN100/101 80/600 0 KYN107 40/300 100/750 Total 120/900 100/750 Grand total 220 days/1650 hours CFP Course The two categories of programme days or hours are used as follows. Study days or hours The 40 days or 300 hours in KYN107 are used for attending tutorials, reading course materials and text, working on the DVDs, writing assignments and personal study. This work may be completed in your home, or a library, or wherever you find it best to study. Some of the learning activities guide you through a series of readings which will help you to understand issues important to practice situations and skills, and relevant theories. Other activities will stimulate questions and highlight issues that you will want to raise for discussion during your tutorials. Supernumerary practice days or hours The 100 days or 750 hours in KYN107 are used for sustained learning in practice as part of a care team, delivering care to clients, following client care pathways, and following through with care. This experience may be called ‘placement’ in your organisation, although the OU’s Pre-Registration Nursing Programme team prefers the term ‘practice learning’. During this time, there will be formative and summative assessment of your achievement of the NMC outcomes in practice. Your achievement of the NMC outcomes will be recorded in your Portfolio. The term ‘supernumerary’ means that you will not be counted as part of the workforce, although you will be rostered as part of the staff. This facilitates you being involved in continuity of 10 Guidelines for Completing the Common Foundation Programme Portfolio care for patients or clients and developing teamwork skills. Your supernumerary status also enables you to negotiate with your mentor opportunities to experience practice learning in other practice areas other than your work base. For example, you may want to attend home visits with clients or patients you are caring for. During practice learning time, you should be working with your mentor for the equivalent of 40 per cent of your working week. The 100 days or 750 hours of your practice learning time must be recorded in the Record of Practice Hours and Experience in your Portfolio. The course materials and learning activities will direct some of your supernumerary practice time. Their purpose is to allow you to arrange practice learning experiences which relate to what you are learning in the course. You should use supernumerary practice time to undertake the activities in the course materials. When you write up the activity, you can use this as evidence in your Portfolio. Each activity is linked to one or more of the NMC outcomes. In addition, some of the activities will provide the basis for TMAs or the examinable component at the end of the course. During supernumerary practice time, you should be supervised by your mentor or a practice supervisor. 1.4 Practice learning requirements This section gives an overview of practice learning requirements. Please note: it is important that you refer to Section 4 of your Programme Guide for detailed guidance on how to meet practice learning requirements. Common Foundation Programme (all students) To ensure that the practice learning opportunities you have in KYN107 meet the statutory body requirements of the NMC, you must have access to the following practice learning opportunities, which represent the four disciplines or branches of nursing: l Adult l Mental Health l Learning Disabilities l Child. In addition, you should: l spend one complementary and/or contrasting practice learning period outside your programme practice learning base l include exposure to community-based care l include exposure to acute patient care. l include exposure to continuing care/rehabilitation You should also experience the delivery of care across the 24 hours and seven days a week cycle. This will give you an appreciation of the diverse patient and client issues and the valuable learning opportunities that night-time presents. It is important to do night duty on a minimum of two occasions across the programme and for each occasion to consist of at least three shifts. 1 Introduction to the Portfolio 11 Adult Branch students By the end of your branch programme, you must provide evidence to your mentor and your programme tutor that your programmebased practice learning meets the European Union requirements (EU, 1977) about: l general and specialist medicine l general and specialist surgery l l l the needs of children – a requirement during the CFP (termed ‘child care and paediatrics’ by the EU) the needs of people with mental health issues – a requirement during the CFP (termed ‘mental health and psychiatry’ by the EU) care of older people (termed ‘care of the old and geriatrics’ by the EU) l community nursing (termed ‘home nursing’ by the EU) l maternity care. In addition, you must provide evidence of practice experience in: l acute care l low, medium and high levels of dependency (this will be specific to the patient or client group and to the context of care) l interprofessional working. More details and guidance are given later in this guide. Mental Health Branch students By the end of your branch programme, you must provide evidence to your mentor and your programme tutor that you have done programme-based practice learning in relation to: l care of older people l acute care l care of people with severe and enduring mental health problems l community care l care of children or adolescents (care of children is a requirement during the CFP) l care of adults (a requirement during the CFP). In addition, you must provide evidence of practice experience in: l acute care l low, medium and high levels of dependency (this will be specific to the patient or client group and to the context of care) l interprofessional working. You will need a copy of the Summary of Practice Hours and Experience form in your CFP Portfolio for your first branch Portfolio. This will provide an ongoing record of the areas and client groups you have experienced or gained insights into so far in the programme. At the end of the CFP, transfer a copy of the Summary 12 Guidelines for Completing the Common Foundation Programme Portfolio of Practice Hours and Experience form in your KYN107 Portfolio and insert it into your Branch Portfolio. You will find further guidance on how to complete your Portfolio in Section 3, and your programme tutor will also support you in doing this. The next section explores the Portfolio forms and provides details and discussion of the practice experiences described above. 2 The Portfolio forms explained 13 2 The Portfolio forms explained Your Portfolio consists of three sections: l Essential information l Self-assessment records l Evidence index. Each section contains a series of forms, each of which has a vital function in documenting your experience, progress and achievements during the CFP. As you read the following description of the components, you may want to have the relevant forms beside you. Section 3 of this guide explains in detail how to use the forms. 2.1 Essential information Student Personal Details The Portfolio starts with a form for your personal details. Fill this in straight away. Mentor/Practice Supervisor Details You should ask your mentor or practice supervisor to complete one of these forms at the earliest opportunity. They must complete and sign this form in their own handwriting, as this is required for the verification process. Remember that you must have one identified mentor, who has received mentor preparation and assesses the NMC outcomes and completes your Record of Progress at the end of your practice experience. A mentor is required to: l be a registered nurse l be registered in the same branch of nursing as the students are studying l fulfil the NMC’s requirements for mentors and mentorship. Mentors also accept responsibility for: l supporting students’ access to learning opportunities l facilitating practice learning l supervising students when they are doing programme-based practice in the practice area l liaising with colleagues and practice supervisors l assessing students’ performance and learning in practice. In the CFP you are required to undertake a minimum of one period of practice learning that complements or contrasts with your normal place of practice learning. This will broaden your learning and give you experience of different ways of delivering and managing care. During this period your practice learning will be supported by a practice supervisor. This is a nurse or other professional who fulfils the same role as your mentor but is more familiar with the 14 Guidelines for Completing the Common Foundation Programme Portfolio complementary or contrasting area than your mentor. When you arrive in your complementary or contrasting area, you should ask your practice supervisor to complete one of the forms. Record of Progress Your progress in practice is monitored through three discussion meetings with your mentor and your programme tutor. These are spread throughout the course: one near the beginning of your practice experience, one around the middle, and one towards the end. The dates for these meetings are marked on your Study Calendar. On the Record of Progress form you, your mentor and your programme tutor document your progress as you achieve the NMC outcomes. All three of you should write your signature and the date in the spaces provided. The NMC outcomes and the supporting evidence should be signed off preferably in Discussion 3, but definitely by the submission date. If you have not reached Bondy Level 2 in all NMC outcomes by Discussion 3, you will need to achieve them, provide evidence in support of this achievement, and have the forms signed off before you submit your Portfolio. Levels achieved after Discussion 3 should be signed off in the column headed ‘Final Bondy level’. You may not have the opportunity to meet your programme tutor between Discussion 3 and the submission date. In this case, ask your mentor to sign off the forms and send photocopies of them and supporting evidence to your programme tutor to enable them to verify your work, and return it to you, before you submit. If you fail to do this, you will not meet the requirements of the course. Essential Skills Clusters Record The NMC introduced essential skills clusters (ESCs) to the nuring curriculum from September 2008 (NMC, 2007). These essential skills clusters are reproduced in the Profile of Practice Skills: a formative resource. A small number of the essential skills are summatively assessed during the CFP and these are recorded on the Essential Skills Clusters Record. The Essential Skills Clusters Record should be completed at each discussion meeting with your mentor and programme tutor. The Profile of Practice Skills – a formative resource will inform your mentor’s decision regarding your achievement of each skill. You must demonstrate achievement of skills 9, 25, 27, 28, 29, 33 and 42 at Bondy level 2 by the end of the CFP. Record of Practice Hours and Experience By the end of the CFP, as well as achieving Level 2 in all the NMC outcomes as described in Section 1.2, you must have had exposure to all four disciplines of nursing: l Adult l Mental Health l Learning Disabilities l Child. 2 The Portfolio forms explained 15 Each practice period must be for a minimum of 30 days. (A day consists of 7.5 hours so, if you work longer or shorter shifts each day, you need to adjust the number of days to achieve at least 225 hours.) Across the programme you are required to learn in practice as part of the interprofessional team and experience the delivery of care for 24 hours and seven days a week, and across a range of services which provide health care and across dependency levels. So, during this period, it is important that you gain experience of services which relate to your learning practice area. For example, if you are based on, or allocated to, a surgical ward, you may follow a care pathway or patient’s journey through: l diagnostic and investigative services l out-patient departments l operating theatres l services provided by specialist nurses l multi-professional team members l community-based services. During the nursing programme, you must experience working in interprofessional teams. It is also important to get an insight into the patient’s or client’s entire experience of health care, and other services, so that you can empathise with their experiences, changing responses and support needs. To enable you to appreciate the diversity of issues or opportunities for patients or clients at night-time, you should do night duty, with the support of your mentor, at least two times during the programme. You need to gain insights into night-time for a patient or client so, preferably, you should follow them for a period of night duty (for example, three shifts on each occasion). On completing each practice period, you should fill in the Record of Practice Hours and Experience and carefully document the hours, workplace details, type of experience, core practice or client group and dependency levels. In your Portfolio, you are asked to record your practice experience and where this practice learning takes place for each period of practice learning. When recording this information in your Portfolio it is extremely important that the specific location of this experience is recorded accurately. In order to do this, you must provide a specific reference to the location in terms of the clinical areas and the hospital or community trust in which this clinical area is located. It is not sufficient to record for example ‘Elm Ward’ with no further means of identifying the location of this clinical area. This information should be recorded as: ‘Elm Ward, Anytown Hospital, Anytown Trust.’ Please ensure that before submission of your Portfolio forms you have provided this information in full for each practice area in which you have had experience. Failure to do so will result in your practice details being incomplete and may delay your registration at the end of your study of the programme. You must also experience the full range of 24-hour care and the seven-day cycle of care during the programme to ensure that your 16 Guidelines for Completing the Common Foundation Programme Portfolio experience includes the full shift pattern, with different day shifts and nights. There is an example form in the Portfolio to help you complete this record. Ask your mentor or practice supervisor to complete the summary of your performance on page 2 of the Record of Practice Hours and Experience form. This form must be signed by your mentor or practice supervisor, your programme tutor and you. You may experience all four branches of nursing in a variety of ways, such as learning through life experience (experiential learning), opportunistic learning through clients from other disciplines accessing your workplace and, where possible, learning through access to discipline-specific designated services. It is not a requirement for you to access discipline-specific designated services but take the opportunity if it arises, provided client care is not compromised. As mentioned in Section 1.4, exposure to maternity care is a requirement if you are studying the Adult Branch Programme. This experience may be gained in a range of ways, including ‘experiential’ learning, as follows. l You could produce an account of your experience of maternity care. l You could produce an account of a family member’s or friend’s experience of maternity. l Your mentor or programme tutor may be able to negotiate time with a community midwife or local community hospital which offers maternity care for ‘low or no risk’ pregnancies. l Rarely, you may be able to access maternity services within acute hospitals. l You could seek an opportunity to visit private or voluntary support groups such as NCT and La Leche. If you gain experience of maternity care during the CFP, you should record this on the Record of Practice Hours and Experience form and the Summary of Practice Hours and Experience form. The requirement for exposure to child care and paediatrics could be met in the following ways. l You could produce an account of a family member’s or friend’s experience of children’s services. l You could seek an opportunity to visit private or voluntary groups and/or contact organisations which provide services to children, for example: local playgroups, opportunity groups to gain insights into the normal development of children child health clinics, child assessment centres to gain insights into childhood health issues and health promotion activities for children’s organisations such as ‘Contact a Family’ to gain insights into the issues faced by children with lifelong or life-limiting health issues a local Red Cross group to gain insights into how to manage first aid emergencies in childhood local schools to listen to a service provider’s or children’s accounts of their experience of services provided to children – even young children can be extremely eloquent about their experience of health care services. 2 The Portfolio forms explained 17 l Your mentor or programme tutor may be able to negotiate time with a practitioner who works with children in a hospital or community setting. l Rarely, you may be able to access designated children’s services. To meet the requirements of the CFP, you must provide evidence of 750 hours of supernumerary experience on your Record of Practice Hours and Experience form. You must log the number of hours of practice learning in each practice setting. You must provide evidence of experiencing the 24-hour cycle of care. Your record must be signed by your mentor or another supervising professional. Use the Summary of Practice Hours and Experience form to help you plan your periods of practice learning. Please ensure that you record the name of the practice learning area and the type of care provided in this setting. Summary of Practice Hours and Experience This form summarises the information from the Record of Practice Hours and Experience forms which you completed at the end of each practice period. You should fill in the forms and ask your mentor and your programme tutor to complete the comments boxes on page 2 of each form. There is an example form in the Portfolio to help you complete this record. Before you submit your Portfolio, please check that you have added up your total hours correctly. If you have not completed the required practice hours, you must still submit your Portfolio by the cut-off date. You must then talk to your programme tutor and your mentor to arrange how to make up the deficit in hours. It is important to transfer a copy of this summary to your Portfolio when you move on to the branch programme on successfully completing the CFP. Ongoing Achievement Record The Ongoing Achievement Record (OAR) summarises your progress in practice throughout the programme. You should meet with your mentor within five days of commencing each practice period to identify your practice learning needs. You should identify your strengths, areas for development and how you will achieve them to enable judgements to be made on your progress. They should be recorded on the first page of the record. You and your mentor should sign the form for each practice period. Through completion of the OAR your concerns are shared and ways forward can be agreed to ensure they are addressed. At the end of each practice learning period you should discuss your progress during the practice learning period with your mentor and record this on the second page of the record. You and your mentor should sign this page of the record for each practice period, as before. Your programme tutor will sign the form at the end of the course. At the end of CFP, you must transfer a copy of the completed Ongoing Achievement Record into your Branch Portfolio. It is important that you keep a copy of your OAR to provide to your 18 Guidelines for Completing the Common Foundation Programme Portfolio ‘sign-off’ mentor to confirm your achievements at the end of your programme. Student Self Declaration of Good Health and Character The Nursing and Midwifery Council (NMC) requires that your health and character are sufficiently good to enable you to practise safely and effectively (NMC, June 2008). If at any time during your study with The Open University (both during and between courses) you become aware and/or are alerted that your health and/or character may not be sufficiently good to enable you to practise safely and effectively you must inform your programme tutor immediately. To inform your programme tutor complete and submit a ‘Student self declaration of good health and character’ form which is available on the ‘More resources’ page of your course website. In addition the NMC requires students to declare that they continue to be of good health and good character annually to the University. To support your compliance with this NMC requirement, we have included a student self declaration of good health and character form in the ‘Essential information’ section of the portfolio. This declaration must be completed and submitted as part of your portfolio at the end of each practice course. All information received will be treated in the strictest confidence. If it is believed to be in the interests of public safety, information may need to be shared with others. You will be advised who the information will be shared with and what information will be shared. Any sharing of information is strictly on a ‘need to know basis’. If you declare any concerns, your declaration will be reviewed by members of a ‘fitness to practise panel’. Failure to comply with the above requirements may place your progress through the nursing programme in jeopardy. 2.2 Self-assessment records To support your achievement and progression in the CFP, you will participate in a minimum of three practice-based discussion meetings with your mentor and your programme tutor. These three meetings are obligatory. There is further information about these meetings in Section 3. After each discussion meeting, you should complete the relevant Discussion Self-Assessment Record, which summarises the discussion between you and your mentor and your programme tutor in Discussion 1, 2 or 3 across all NMC domains. This record should highlight your strengths and learning needs and show your action plan, detailing how you plan to achieve these learning needs. You should also complete the ‘Agreed summary of discussion between student, mentor and programme tutor’ box on page 2 of the form. Once all of these statements have been agreed by you, your mentor and your programme tutor, the form should be signed by all three of you. Your programme tutor should keep copies of these forms to help them verify your Portfolio, parts of which are submitted at the end of each practice course. 2 The Portfolio forms explained 19 2.3 Evidence On this form you should list the evidence you have collected to support your achievement of the NMC outcomes at Bondy Level 2. You should clearly identify each piece of evidence and label it and indicate which outcome(s) it supports. File each piece of evidence behind the Evidence Index form in the order in which it is listed. This will help you to locate the relevant supporting evidence you have selected to demonstrate to your mentor and programme tutor your progress in achieving the NMC outcomes at each discussion meeting. 20 Guidelines for Completing the Common Foundation Programme Portfolio 3 How to complete your Portfolio The central feature of your Portfolio work is practice but you need to have evidence of it. So your Portfolio work consists of: l recording details of your practice on the ‘Essential Information’ forms l collecting supporting evidence of this practice (for example, verification by a practice supervisor, documentation, summary accounts) l three discussions in which you, your mentor and your programme tutor monitor and document your progress. The three discussions should be thoughtful and reflective, and lay the foundations for the sort of discussion about your professional practice that you should take part in throughout your career. You have already looked at the forms in the Portfolio. In this section you will look at the groundwork needed for your Portfolio. This section outlines the sequence of events for completing your Portfolio work and, in particular, explains exactly what sort of supporting evidence you can collect for your Portfolio, and the process to follow in the three discussions when your progress is reviewed. Don’t worry if it seems rather complex now; your programme tutor will talk you through it in an early tutorial. You need to be sure that you fill in your Record of Practice Hours and Experience form for each practice period and your Summary of Practice Hours and Experience form. 3.1 Types of evidence As you have seen, in each of the three discussions you, your programme tutor and your mentor must complete and sign the Record of Progress form to record your performance. Your mentor’s assessment of your achievement for each outcome will be based on three sorts of evidence: l observation of your practice (which they will verify) l discussion with you (which they will verify) l examination of a variety of other supporting evidence you present. Although you should present a wide range of evidence, you are encouraged to demonstrate how one particular piece of evidence can support more than one outcome. However, you must ensure that the quality and the depth of your evidence effectively support the particular NMC outcome that you are claiming to have achieved. Once your mentor and your programme tutor have agreed that a piece of evidence demonstrates your achievement of a particular outcome, you should use the following key to identify the type of evidence. Give each piece of evidence a code and number and record this on both the evidence itself and the Evidence Index form, so that it can be readily located by you, your mentor and your programme tutor. 3 How to complete your Portfolio 21 UA Unit activity: this includes the work you have already completed on the unit activities. When used as supporting evidence in your Portfolio, the activities provide potentially strong evidence and can reduce your workload because this is work you have already done. The unit activities often relate to practical skills development and, in many instances, this includes learning the theory underpinning the skill and then using the skill in practice. Appendix 2 shows an example of a student’s notes written about a unit activity. You could also include a summary of your learning from your coursework relating to NMC outcomes as Portfolio evidence. You may also consider using TMA contents as the basis of Portfolio evidence. If you decide to do this, write a short account indicating how the TMA supports achievement of NMC outcomes and highlight the relevant text within the TMA. C Certificated workshop or employer-led training, supported by a summary account of what you learned from the workshop or training. A certificate alone does not constitute evidence; it should be supported by an account of what you have learned. The certificate should be placed behind the evidence that refers to it. If you refer to it in more than one piece of evidence, you should cross-reference it. T Testimony of other people (written materials, letters, feedback from clients): this can include verification of your performance in practice written by your mentor or other suitably qualified practitioners. The testimony can come from your practice setting or from your complementary practice experience. It can also include verified evidence of a discussion between you and your mentor or another professional. Appendix 3 shows an example of testimony written by a practitioner. Appendix 4 gives details about the circumstances in which it may be acceptable for another Pre-Registration Nursing Programme student to provide testimony for you. SA Summary accounts: these may be after attendance at tutorials, about some practice you have observed or participated in, your understanding of a journal article, or your reading of the companion course KYN100 or KYN101. Appendix 5 shows an example of a summary account written by a student. CD/ Evidence of having worked on a DVD or an audio: this work DVD is a good source of evidence to demonstrate numeracy, information literacy and computer skills. Again, you need to show how these skills will inform your practice. P Presentation of ideas in a public forum: this might be where you have presented information in your practice setting, during a tutorial or at a seminar or a meeting. You should collect verified evidence of your contribution. PW Project work: you may decide that you want to follow up aspects of the course, perhaps through website and evidence searches. If you do something concrete and relevant like this, try to make time to discuss this work and its relevance with a qualified practitioner, and ask them to verify it. RC Resource collection: this should include some summary accounts about what you have learned from these resources. Sources should be referenced accurately. 22 Guidelines for Completing the Common Foundation Programme Portfolio PS Profile of Practice Skills: this can provide supporting evidence of your achievement of the NMC’s Essential Skills clusters and also outcome 2.8. You may use this record in discussion with your mentor and your programme tutor to demonstrate the achievement of these skills. 3.2 Developing an evidence base Section 3.1 lists some types of evidence you may collect to support your achievement of NMC outcomes. All the supporting evidence you select should clearly support your clinical experience. This can be done by explicit reference to the evidence, such as policy documents and journal articles within your practice accounts. Alternatively, you can write a short summary of a document and indicate how it has informed your practice. Similarly, certificates for the successful completion of courses that you have attended (such as moving and handling or infection control) can also be included. However, they must be accompanied by a short summary of your learning from the course and an indication of how you are using this learning to support your practice. One of the most important pieces of evidence you will acquire is verified evidence. This section looks in more detail at how to collect verified evidence of practice and discussion. You should collect evidence as you go along – don’t leave it until the three prearranged discussion meetings! Collecting relevant evidence in a timely fashion to support your practice is the key to a good Portfolio. You are not just finding qualified practitioners to ‘sign off’ the Portfolio. Instead, aim to create a picture of your developing practice and look on it as an album of your achievements. You should make sure that your Portfolio does you justice! Client consent Any evidence collected in a practice situation involving working with a client must be done with the client’s consent. This is not a case of ‘maybe’, ‘possibly’ or ‘if I’ve got time’: you must do it. It is the basis of your ethical approach to clients as a professional practitioner and must happen in your work with patients and clients on a daily basis. It must also be reflected meticulously in your Portfolio and TMAs. Your mentor and your programme tutor will certainly want to discuss this with you and can offer you support and advice. The following protocol will help you build up this aspect of your work. Patients and clients have a fundamental legal and ethical right to determine what happens to their own bodies. Therefore, valid consent to treatment is absolutely essential in all forms of health care. The Department of Health has issued a range of guidance documents on consent for examination or treatment, which can be accessed on its website. Open University student nurses are required to observe the following protocol to ensure that patients agree to have care delivered by a student nurse under supervision. Patients may withdraw their consent at any time. If a patient indicates that they do not want a student nurse to be involved in delivering their care, you must respect their views and inform your practice supervisor. 3 How to complete your Portfolio 23 Protocol for gaining clients’ consent As a student nurse, you must always ensure that patients and their carers have agreed to receive your care and, in addition, know who is responsible for supervising your practice. You must follow this protocol when you first meet a patient or their carer. 1 Introduce yourself as a student nurse and state who is supervising your practice. 2 Ask the patient or carer whether they agree to receive care from you as a student under supervision. 3 If the patient or carer asks questions, or seeks more information about the care you want to offer, explain this care and discuss it with them. 4 Ask the patient or carer whether they would like to speak to your supervisor about the care that you want to offer. If they would like to discuss any aspect of this care with your supervisor, tell them you will ask your supervisor to speak to them before you offer any care. 5 If the patient or carer does not offer complete agreement and seems confused or worried about your role, refer this to your supervisor before taking any further action. 6 If the patient or carer offers complete agreement, you may progress to offering the care agreed. Use this protocol whenever you approach a patient or carer with whom you have not previously worked. Also use the protocol if you are working with the patient or carer as a student nurse for the first time, even if you know them from a previous role you have held in that care environment. Verified evidence of practice The activities in the course materials form a framework for your practice experiences. They enable you to link your practice with the theory that underpins it. Each activity is linked to at least one of the NMC outcomes that you must achieve by the end of KYN107. Some course activities suggest that you do a piece of work under your mentor’s supervision. Others may direct you to observe or reflect on practice. When you submit course activity notes, use the key UA (unit activity) and add the block number, unit number and activity number it relates to, for example: B2/U16/A10 means Block 2, Unit 16, Activity 10. If you arrange for your mentor or another practice supervisor to watch you carry out a piece of practice, you can write a summary account about this and ask them to verify, sign and date it. Use the key SA when listing it on your Evidence Index and on the evidence itself. Alternatively, your practice supervisor could write an account or a testimony of what they saw you do in practice, then sign and date it. Use the key T (testimony) when referring to this form of evidence. The NMC outcomes beginning with ‘Demonstrate’ are all likely to require that your mentor verifies actual practice. 24 Guidelines for Completing the Common Foundation Programme Portfolio Verified evidence of discussion You should note that some of the NMC outcomes require you to be able to ‘discuss’ certain practice issues. It is a good idea to check the exact word that begins each outcome so that you are clear about the type of evidence you need to produce. Again, verification by your mentor that a discussion has taken place is central evidence. This should be listed on both the evidence and the Evidence Index as T (testimony) if it has been written and signed by your practice supervisor. If written by you, it should be listed as SA (summary account) and must be countersigned by the practice supervisor you had the discussion with. Verified evidence of courses and workshops During the programme you are expected to attend various courses or workshops organised by your employer (such as moving and handling or basic life support), in order to update your skills. Certificates from these workshops are essential pieces of evidence. Keep them and put them in your Portfolio and relate them to a relevant NMC outcome. Use the key C (certificate) on the Evidence Index. The certificate must be current and up to date and must be accompanied by a summary of what you have learned and how that relates to your practice. Issues of unsafe practice When writing about the care you have delivered, you must demonstrate an awareness of what constitutes safe and unsafe practices in care delivery. This does not mean you cannot write about unsafe practice you might have seen. For example, you may witness unsafe practice and write about it, indicating the issues arising and what changes may be required to avoid such practice in future. If you write about unsafe practice but do not identify it as unsafe practice, you will be penalised and the matter referred to the Examinations and Assessment Board. 3.3 Guidelines on confidentiality Your Portfolio evidence can draw on both your personal and your work experiences. This may mean including information about, and occasionally passing judgement on, the organisation you work for and your colleagues, patients or clients. When using such material in your Portfolio evidence, you should make sure that all information is made anonymous, for example by changing or removing the names of people or places. If you refer to a patient by name then you should change their name and explicitly acknowledge that you have changed it. It is good practice to cite the requirements of The Code: Standards of Conduct, Performance and Ethics for Nurses and Midwives (NMC, 2008). For example, ‘I greeted Mrs Green (name changed to ensure confidentiality) on admission and showed her around the ward.’ You should also check that you have the permission of the 3 How to complete your Portfolio 25 person(s) concerned to use any material. Make sure you read through your supporting evidence and remove every mention of the clinical setting and patient or client details. If you want to use your employer’s or your trust’s headed paper for any items of supporting evidence, you must ensure that their policy on the use of headed paper is observed. You must get permission from the trust or employer before using headed paper in your evidence. Using such paper in your evidence does not in itself compromise client confidentiality, provided that the anonymity of the patient and clinical area is preserved. It is important that you ensure your Portfolio is kept secure at all times, whether at home, at work, in tutorials, or in any other place. You must observe the standard of confidentiality set out in The Code. Therefore, your Portfolio should not be shared with anyone who is not connected with the Pre-Registration Nursing Programme. Your assignments are normally confidential documents and will be treated as such by University staff. Only members of staff who need to see them will have access to them, for example your course tutor. However, because of the nature of the subjects covered by courses from the Faculty of Health and Social Care, there may be exceptional cases where the confidentiality rule may need to be reconsidered. Note that if your written evidence in your Portfolio refers to dangerous practice or the abuse of patients or clients, the course team cannot maintain confidentiality, and follow-up action will be necessary. Here is the explanation of the steps a tutor will follow in such a situation. l The tutor will contact the local Staff Tutor to discuss the matter. l The tutor is free to discuss the matter with the student if they feel competent to do so. l Any proposed action should be discussed by the Staff Tutor and the Course Team Chair and Director of the Pre-Registration Nursing Programme, who will refer it to an Associate Dean of the Faculty if required. l No action will be taken without the formal approval of the Dean. l No action will be taken without full consultation with the student concerned and without serious consideration of the likely consequences. 3.4 The three discussion meetings During the course you will participate in a minimum of three practice-based discussion meetings with your mentor and your programme tutor. These three discussion meetings support your achievement and progression and are obligatory. At each meeting the supporting evidence you are collecting is reviewed and used as a basis to identify which Bondy level you have achieved for each outcome. 26 Guidelines for Completing the Common Foundation Programme Portfolio It is your responsibility to negotiate the timing of these meetings and to liaise with your mentor and your programme tutor to agree the date of the first discussion meeting. This should be as early as possible in the course, as indicated on the Study Calendar, and before you do any practice learning. The first meeting should identify your level of practice at the beginning of the course. It is important that your discussion is open and honest, and identifies your strengths and any learning needs for each outcome. Discussion 1 As discussed above, within the first few weeks of the course you, your programme tutor and your mentor should meet to discuss each NMC outcome in relation to your level of practice. The Discussion Self-Assessment Record forms the basis of the discussion and you should complete page 1 of it before your meeting. At the meeting you, your programme tutor and your mentor should plan how any learning needs you have identified will be addressed. These should be recorded on the Self-Assessment Record and summarised on page 2 of it. An important function of Discussion 1 is checking your Ongoing Achievement Record. You will probably find it simplest to go through the Portfolio together with your mentor and your programme tutor. For every outcome you should discuss which level you are performing at, based on the supporting evidence you provide. Look back at Table 1 for an explanation of Bondy Levels 1 and 2. Your mentor will assess your performance against each NMC outcome and then record the Bondy level you are currently practising at on the Record of Progress form. You might have already achieved some NMC outcomes at Level 2, but you must provide evidence to support this. You will need to record the type of evidence you provide using the key in Section 3.1. After working through the NMC outcomes, you need to reflect on your overall progress. Remember that you, your mentor and your programme tutor must complete and sign the Record of Progress, the Ongoing Achievement Record and the Discussion 1 Self-Assessment Record (page 2), stating when learning needs must be addressed and the date for Discussion 2. Checklist for the discussion meeting At the discussion meeting you should all agree: l where you are in relation to achieving the required level in each NMC outcome l where you are in relation to achieving the required level in the essential skills l Ongoing Achievement Record. l which NMC experience requirements need to be accessed outside your normal place of work (refer to the Summary of Practice Hours and Experience form) 3 How to complete your Portfolio 27 l who will arrange access to opportunities or experiences outside your normal place of work, when will they occur and the arrangements for induction to those opportunities or experiences l the date, time and place of the second and third discussion meetings. You should refer to the Study Calendar to establish the recommended timing of these meetings. Practice work During the first few months of your practice work, you will be developing the areas identified in Discussion 1. Remember to collect and save your supporting evidence as you go along and to file each piece of evidence behind the Evidence divider in your Portfolio. Also record each piece of evidence on the Evidence Index. Remember also to use course activities as much as possible to help you collect and structure your evidence. Do all the learning activities suggested and, where possible, ask your mentor or another professional to witness and sign what you do. Discussion 2 The second discussion meeting is a formative activity. It should take place about half way through your practice experience, as indicated on the Study Calendar. It provides an important opportunity to explore: l what you have learned l what you still need to learn l the quality of the supporting evidence you have collected to support achievement of the NMC outcomes l which practice level you have achieved in each NMC outcome and what you still need to do to achieve the required level for the course l which learning activities or evidence gathering you still need to do to demonstrate achievement of the NMC outcomes at the required practice level l which practice level you have achieved for each essential skill and what you still need to do to achieve the required level for the pcourse. This meeting is, therefore, a ‘looking back’ and ‘looking forward’ activity and is very important if you are to reach the required Bondy Level 2 in practice by the end of the course. You, your mentor and your programme tutor should review your progress, focusing particularly on your learning needs identified in the Discussion 1 Self-Assessment Record. The level of achievement gained is noted on the Record of Progress. Again, you should complete page 1 of the Discussion 2 Self-Assessment Record before the meeting. In the meeting, page 2 of the Discussion 2 Self-Assessment Record should be completed, which summarises the discussion between you and your mentor and your programme tutor. It should highlight your strengths and learning needs and show your action plan, detailing how you plan to achieve these learning needs. You should also complete the ‘Agreed summary of discussion’ comments box. Once all of these 28 Guidelines for Completing the Common Foundation Programme Portfolio statements have been agreed by you, your mentor and your programme tutor, the form should be signed by all three of you. The Ongoing Achievement Record also needs to be reviewed and amended as necessary. Your programme tutor should keep copies of these forms. Check how many outcomes you still need to work on. If you, your mentor and your programme tutor decide that you are having problems with any of the outcomes, you will need to arrange another review before Discussion 3. Document this on the Discussion 2 SelfAssessment Record for the appropriate NMC domain. Practice work You now continue with your practice work, again finding every opportunity to build up your supporting evidence. By now, you will probably be clear about the outcomes you still need to work on. This may partly be a matter of not having had enough opportunity to achieve a particular outcome, but you should also be alert to outcomes that you find more difficult and seek opportunities to focus on these. Discussion 3 The third, and normally final, discussion meeting should take place a few weeks before the end of the course, as indicated on the Study Calendar. This is the summative assessment activity, which involves your mentor judging whether you have achieved the NMC outcomes and essential skills at Bondy Level 2 for KYN107. This is a requirement for completing the CFP. Your mentor’s judgement will be informed by: l direct observation of your practice l review of the supporting evidence provided by you l feedback provided by colleagues such as practice supervisors. Your programme tutor supports this decision making. This meeting is, therefore, primarily a ‘looking back’ activity. The level of achievement gained is noted on the Record of Progress. Again, you should complete page 1 of the Discussion 3 Self-Assessment Record before the meeting, and page 2, which summarises the discussion between you, your mentor and your programme tutor, at the meeting. This should highlight your level of achievement, and particularly detail your plan to achieve any outstanding NMC outcomes or essential skills. You should also complete the ‘Agreed summary of discussion’ comments box. Once all of these statements have been agreed by you, your mentor and your programme tutor, the form should be signed by all three of you. The Ongoing Achievement Record should again be reviewed and amended as necessary. Your programme tutor should keep copies of these forms. If you have achieved all of the NMC outcomes to Bondy level 2 by this stage, you should have all your Record of Progress forms signed and dated by both you and your mentor, with the ‘Final Bondy level’ section of the form completed and verified by your programme tutor. If there are any outcomes you have not yet achieved at Bondy Level 2, 3 How to complete your Portfolio 29 it is very important that you, your mentor and your programme tutor are clear about which ones they are and plan how to achieve them before the end of the course. If you have achieved the required CFP essential skills to Bondy Level 2, you should have the Essential Skills Clusters Record signed by both you and your mentor and verified by your programme tutor. If there are any essential skills you have not yet achieved at Bondy Level 2, it is very important that you, your mentor and your programme tutor are clear about which ones they are and plan how to achieve them before the end of the course. In the last few weeks, you need to work on any outcomes not achieved at Level 2, collecting supporting evidence as you go. Ask your mentor to review your evidence and sign that you have achieved Level 2 in the ‘Final Bondy level’ section on the Record of Progress form. You need all your forms signed, ready to submit to the University, by the end of this period. Remember, at the end of CFP, you must transfer a copy of the completed Ongoing Achievement Record into your Branch Portfolio. Non-achievement of NMC outcomes and essential skills at Level 2 If you do not achieve all the outcomes or the required essential skills at Level 2 by the end of the course, discuss the issue with your programme tutor, who will advise you about any further practice you are required to do. Ensure that you identify what action you will take to achieve these outstanding outcomes or essential skills as part of your action plan on the Discussion Self-Assessment Record forms. You should also ensure this is recorded on the Ongoing Achievement Record. 3.5 Portfolio compilation and submission Your Portfolio must show that you have completed the required study and practice elements of the course: for example, practice hours, practice experience and achievement of NMC outcomes and essential skills. If any of this information is missing, your course result will be delayed until you have supplied it. At the end of the course you must submit two copies of the Essential Information section only of your Portfolio. This includes the forms: l Student Personal Details l Mentor/Practice Supervisor Details l Record of Progress l Essential Skills Clusters Record l Record of Practice Hours and Experience l Summary of Practice Hours and Experience l Ongoing Achievement Record l Student Self-Declaration of Good Health and Character. 30 Guidelines for Completing the Common Foundation Programme Portfolio Please make sure that you photocopy the first section of your Portfolio and send it, plus the original section, to the University by the date specified in the Assessment Guide. You must submit two copies of all the forms labelled ‘Essential Information’. This will ensure that your progression to the branch programme is not delayed by an incomplete record. It will also avoid the unnecessary anxiety caused by you having to supply additional information. You are not required to submit the supporting evidence, but you should keep this evidence in the original ring binder, as you may want to develop some of this evidence when you move into branch, to demonstrate your progression through the Programme. The Portfolio forms must be attached together so they do not become separated. We recommend that you purchase two Report Files from a stationer and insert a set of forms into each one. These are very inexpensive and lightweight; postage costs will therefore be lower than if you submit your Portfolio ring binder. Your original Essential Information section will be returned to you. The University will keep the copy so that it can update your student record. At the end of the programme the University will use this information to confirm to the NMC that you are eligible to enter the register of nurses. In the past, there have been instances where the two copies submitted from the Portfolio were not identical. In such cases, further information has to be sought from the student before their record can be completed and they become eligible for progression. Portfolio submission checklist The following checklist will help you ensure that the Essential Information section of your Portfolio is complete before submission. It is important that each form is carefully reviewed to make certain that all details are correct. You must note that if your Portfolio is incomplete by the submission date given in the Assessment Guide, you must still submit it. Non-submission of your Portfolio will result in a fail being awarded for the course and could affect your progression through the programme. l Submit only the Essential Information section of your Portfolio. l Have you completed the Student Personal Details form? l Have you asked your mentor and all of your supervising practitioners to fill out and sign a Mentor/Practice Supervisor Details form? l Record of Progress Have you achieved Level 2 in all 20 NMC outcomes? If you had some outcomes outstanding in Discussion 3, check that your mentor and your programme tutor have signed off the remaining ones. Have you checked that you, your mentor and your programme tutor have signed and dated the Record of Progress? 3 How to complete your Portfolio l 31 Essential Skills Clusters Record Have you achieved Level 2 in all essential skills? If you had some skills outstanding in Discussion 3, check that your mentor and your programme tutor have signed off the remaining ones. Have you checked that you, your mentor and your programme tutor have signed and dated the Essential Skills Clusters Record? l Record of Practice Hours and Experience Have you completed a Record of Practice Hours and Experience form for all of your practice periods? Have you ticked all types of experience covered during this period? Have you ensured that the forms have been signed by you, your mentor or practice supervisor and your programme tutor? Has your mentor or practice supervisor completed the Summary of Performance comment box on page 2 of the form? Have you checked that the practice hours you have recorded add up to the total number of 750 practice hours required by the course? l Summary of Practice Hours and Experience Have you ensured that you have recorded all types of experience you have gained? Does the information recorded match what you have recorded on the Records of Practice Hours and Experience? Has your mentor and your programme tutor completed their comment boxes on page 2? Have you ensured that you, your mentor and your programme tutor have signed the form? Have you taken a photocopy to transfer to your Branch Portfolio? l Ongoing Achievement Record Have you completed the Ongoing Achievement Record for all practice learning periods? Have you checked that you, your mentor and your programme tutor have signed and dated the Ongoing Achievement Record Have you taken a copy of the Ongoing Achievement Record to transfer to your branch Portfolio? l Student Self-Declaration of Good Health and Character Have you completed and signed the Student Self-Declaration of Good Health and Character form and included it with your ‘Essential Information’ forms? l Submission of Portfolio Have you purchased ‘Report Files’ in order to submit your two copies of the Essential Information forms securely? If you fail to follow these points, your Portfolio will be returned to you for completion, which could delay your progression through the programme. 32 Guidelines for Completing the Common Foundation Programme Portfolio References Bondy, K.N. (1983) ‘Criterion-referenced definitions for rating scales in clinical evaluation’, Journal of Nursing Education, vol. 22, no. 9, pp. 376–82. EU (1977) Clinical Instruction, 77/453/EEC, 27 June 1977, Brussels, Office of the Official Publications of the European Community. NMC (2004) Standards of Proficiency for Pre-Registration Nursing Education, London, Nursing and Midwifery Council. NMC (2007) Circular 07/2007 Introduction of Essential Skills Clusters for Pre-Registration Nursing Programmes, London, Nursing and Midwifery Council. NMC (2008) The Code Standards of Conduct, Performance and Ethics for Nurses and Midwives, London, Nursing and Midwifery Council. Appendix 1 NMC outcomes 33 Appendix 1 NMC outcomes The Nursing and Midwifery Council (NMC) is the statutory body which regulates nursing, midwifery and health visiting in the four countries of the UK. It has identified four areas of practice referred to as domains. Within each domain, outcomes and standards of proficiency have been identified, together with exemplars. The outcomes must be achieved for completion of the Common Foundation Programme and entry to the branch programme of your choice. The standards of proficiency must be achieved by the end of the branch programme for entry to the professional register. Domain Outcomes for entry to chosen branch Standards of proficiency for entry to the register 1 Professional and ethical O1.1 Discuss in an informed manner P1.1 Manage oneself, one’s practice, practice the implications of professional and that of others, in accordance regulation for nursing practice with The Code Standards of conduct, performance and ethics for nurses and O1.1.1 demonstrate a basic midwives, recognising one’s own knowledge of professional regulation abilities and limitations and self-regulation P1.1.1 practise in accordance with The O1.1.2 recognise and acknowledge Code Standards of conduct, performance the limitations of one’s own abilities and ethics for nurses and midwives O1.1.3 recognise situations that require referral to a registered practitioner O1.2 Demonstrate an awareness of The Code Standards of conduct, performance and ethics for nurses and midwives O1.2.1 commit to the principle that the primary purpose of the registered nurse is to protect and serve society O1.2.2 accept responsibility for one’s own actions and decisions O1.3 Demonstrate an awareness of, and apply ethical principles to, nursing practice P1.1.2 use professional standards of practice to self-assess performance P1.1.3 consult with a registered nurse when nursing care requires expertise beyond one’s own current scope of competence P1.1.4 consult other health care professionals when individual or group needs fall outside the scope of nursing practice P1.1.5 identify unsafe practice and respond appropriately to ensure a safe outcome P1.1.6 manage the delivery of care services within the sphere of one’s own accountability O1.3.1 demonstrate respect for patient and client confidentiality (continued) 34 Guidelines for Completing the Common Foundation Programme Portfolio Domain Outcomes for entry to chosen branch Standards of proficiency for entry to the register 1 (continued) O1.3.2 identify ethical issues in day-to-day practice P1.2 Practise in accordance with an ethical and legal framework which ensures the primacy of patient and client interest and wellbeing and respects confidentiality O1.4 Demonstrate an awareness of legislation relevant to nursing practice O1.4.1 identify key issues in relevant legislation relating to mental health, children, data protection, manual handling, and health and safety, etc. O1.5 Demonstrate the importance of promoting equity in patient and client care by contributing to nursing care in a fair and antidiscriminatory way O1.5.1 demonstrate fairness and sensitivity when responding to patients, clients and groups from diverse circumstances P1.2.1 demonstrate knowledge of legislation and health and social policy relevant to nursing practice P1.2.2 ensure the confidentiality and security of written and verbal information acquired in a professional capacity P1.2.3 demonstrate knowledge of contemporary ethical issues and their impact on nursing and health care P1.2.4 manage the complexities arising from ethical and legal dilemmas P1.2.5 act appropriately when seeking access to caring for patients and clients in their own homes O1.5.2 recognise the needs of patients and clients whose lives are affected by disability, however manifest P1.3 Practise in a fair and antidiscriminatory way, acknowledging the differences in beliefs and cultural practices of individuals or groups P1.3.1 maintain, support and acknowledge the rights of individuals or groups in the health care setting P1.3.2 act to ensure that the rights of individuals and groups are not compromised P1.3.3 respect the values, customs and beliefs of individuals and groups P1.3.4 provide care which demonstrates sensitivity to the diversity of patients and clients Appendix 1 NMC outcomes 35 Domain Outcomes for entry to chosen branch Standards of proficiency for entry to the register 2 Care delivery O2.1 Discuss methods of, barriers to and the boundaries of effective communication and interpersonal relationships P2.1 Engage in, develop and disengage from therapeutic relationships through the use of appropriate communication and interpersonal skills O2.1.1 recognise the effect of one’s own values on interactions with patients and clients and their carers, families and friends P2.1.1 utilise a range of effective and appropriate communication and engagement skills O2.1.3 acknowledge the boundaries of a professional caring relationship P2.1.2 maintain and, where appropriate, disengage from professional caring relationships which focus on meeting the patient’s or client’s needs within professional therapeutic boundaries O2.2 Demonstrate sensitivity when interacting with and providing information to patients and clients P2.2 Create and utilise opportunities to promote the health and wellbeing of patients, clients and groups O2.3 Contribute to enhancing the health and social wellbeing of patients and clients by understanding how, under the supervision of a registered practitioner, to: P2.2.1 consult with patients, clients and groups to identify their need and desire for health promotion advice O2.1.2 utilise appropriate communication skills with patients and clients O2.3.1 contribute to the assessment of health needs O2.3.2 identify opportunities for health promotion O2.3.3 identify networks of health and social care services O2.4 Contribute to the development and documentation of nursing assessments by participating in comprehensive and systematic nursing assessment of the physical, psychological, social and spiritual needs of patients and clients O2.4.1 be aware of assessment strategies to guide the collection of data for assessing patients and clients and use assessment tools under guidance P2.2.2 provide relevant and current health information to patients, clients and groups in a form which facilitates their understanding and acknowledges choice or individual preference P2.2.3 provide support and education in the development and/or maintenance of independent living skills P2.2.4 seek specialist or expert advice as appropriate P2.3 Undertake and document a comprehensive, systematic and accurate nursing assessment of the physical, psychological, social and spiritual needs of patients, clients and communities P2.3.1 select valid and reliable assessment tools for the required purpose O2.4.2 discuss the prioritisation of care needs (continued) 36 Guidelines for Completing the Common Foundation Programme Portfolio Domain Outcomes for entry to chosen branch Standards of proficiency for entry to the register 2 (continued) O2.4.3 be aware of the need to reassess patients and clients as to their needs for nursing care P2.3.2 systematically collect data regarding the health and functional status of individuals, clients and communities through appropriate interaction, observation and measurement O2.5 Contribute to the planning of nursing care, involving patients and clients and, where possible, their carers, demonstrating an understanding of helping patients and clients to make informed decisions O2.5.1 identify care needs based on the assessment of a patient or client O2.5.2 participate in the negotiation and agreement of the care plan with the patient or client and with their carer O2.5.3 inform patients and clients about intended nursing actions, respecting their right to participate in decisions about their care O2.6 Contribute to the implementation of a programme of nursing care, designed and supervised by registered practitioners O2.6.1 undertake activities which are consistent with the care plan and within the limits of one’s own abilities O2.7 Demonstrate evidence of a developing knowledge base which underpins safe and effective nursing practice O2.7.1 access and discuss research and other evidence in nursing and related disciplines O2.7.2 identify examples of the use of evidence in planned nursing interventions P2.3.3 analyse and interpret data accurately to inform nursing care and take appropriate action P2.4 Formulate and document a plan of nursing care, where possible in partnership with patients, clients, their carers and family and friends, within a framework of informed consent P2.4.1 establish priorities for care based on individual or group needs P2.4.2 develop and document a care plan to achieve optimal health P2.4.3 identify expected outcomes, including a time frame for achievement and/or review in consultation with patients, clients, their carers and family and friends and with members of the health and social care team P2.5 Based on the best available evidence, apply knowledge and an appropriate repertoire of skills indicative of safe nursing practice P2.5.1 ensure that current research findings and other evidence are incorporated in practice P2.5.2 identify relevant changes in practice or new information and disseminate it to colleagues P2.5.3 contribute to the interventions which support and optimise the health and wellbeing of patients and clients Appendix 1 NMC outcomes 37 Domain Outcomes for entry to chosen branch Standards of proficiency for entry to the register 2 (continued) O2.8 Demonstrate a range of essential nursing skills, under the supervision of a registered nurse, to meet individuals’ needs, which include: P2.5.4 demonstrate the safe application of the skills required to meet the needs of patients and clients within the current sphere of practice maintaining dignity, privacy and confidentiality; effective communication and observational skills, including listening and taking physiological measurements; safety and health, including moving and handling and infection control; essential first aid and emergency procedures; administration of medicines; emotional, physical and personal care, including meeting the need for comfort, nutrition and personal hygiene P2.5.5 identify and respond to patients’ and clients’ continuing learning and care needs P2.5.6 engage with, and evaluate, the evidence base that underpins safe nursing practice P2.6 Provide a rationale for the nursing care delivered which takes account of social, cultural, spiritual, legal, political and economic influences P2.6.1 identify, collect and evaluate information to justify the effective O2.9 Contribute to the evaluation of utilisation of resources to achieve the appropriateness of nursing care planned outcomes of nursing care delivered P2.7 Evaluate and document the O2.9.1 demonstrate an awareness of outcomes of nursing and other the need to assess regularly a patient’s interventions or client’s response to nursing P2.7.1 collaborate with patients and interventions clients and, when appropriate, additional carers to review and O2.9.2 provide for a supervising monitor the progress of individuals registered practitioner, or groups towards planned evaluative commentary and outcomes information on nursing care based on personal observations and P2.7.2 analyse and revise expected actions outcomes, nursing interventions and priorities in accordance with O2.9.3 Contribute to the changes in the individual’s condition, documentation of the outcomes of needs or circumstances nursing interventions O2.10 Recognise situations in which agreed plans of nursing care no longer appear appropriate and refer these to an appropriate accountable practitioner P2.8 Demonstrate sound clinical judgement across a range of differing professional and care delivery contexts O2.10.1 demonstrate the ability to discuss and accept care decisions P2.8.1 use evidence-based knowledge from nursing and related disciplines to select and individualise nursing interventions O2.10.2 accurately record observations made and communicate these to the relevant members of the health and social care team P2.8.2 demonstrate the ability to transfer skills and knowledge to a variety of circumstances and settings (continued) 38 Domain Guidelines for Completing the Common Foundation Programme Portfolio Outcomes for entry to chosen branch 2 (continued) Standards of proficiency for entry to the register P2.8.3 recognise the need for adaptation and adapt nursing practice to meet varying and unpredictable circumstances P2.8.4 ensure that practice does not compromise the nurse’s duty of care to individuals or the safety of the public 3 Care management O3.1 Contribute to the identification of actual and potential risks to patients, clients and their carers, to oneself and to others and participate in measures to promote and ensure health and safety O3.1.1 understand and implement health and safety principles and policies P3.1 Contribute to public protection by creating and maintaining a safe environment of care through the use of quality assurance and risk management strategies P3.1.1 apply relevant principles to ensure the safe administration of therapeutic substances P3.1.2 use appropriate risk assessment O3.1.2 recognise and report situations tools to identify actual and potential risks which are potentially unsafe for patients, clients, oneself and others P3.1.3 identify environmental hazards and eliminate and/or prevent where O3.2 Demonstrate an understanding possible of the role of others by participating in interprofessional working practice P3.1.4 communicate safety concerns O3.2.1 identify the roles of the members of the health and social care team O3.2.2 work within the health and social care team to maintain and enhance integrated care O3.3 Demonstrate literacy, numeracy and computer skills needed to record, enter, store, retrieve and organise data essential for care delivery to a relevant authority P3.1.5 manage risk to provide care which best meets the needs and interests of patients, clients and the public P3.2 Demonstrate knowledge of effective interprofessional working practices which respect and utilise the contributions of members of the health and social care team P3.2.1 establish and maintain collaborative working relationships with members of the health and social care team and others P3.2.2 participate with members of the health and social care team in decision making concerning patients and clients P3.2.3 review and evaluate care with members of the health and social care team and others Appendix 1 NMC outcomes Domain 39 Outcomes for entry to chosen branch 3 (continued) Standards of proficiency for entry to the register P3.3 Delegate duties to others, as appropriate, ensuring that they are supervised and monitored P3.3.1 take into account the role and competence of staff when delegating work P3.3.2 maintain one’s own accountability and responsibility when delegating aspects of care to others P3.3.3 demonstrate the ability to coordinate the delivery of nursing and health care P3.4 Demonstrate key skills P3.4.1 literacy – interpret and present information in a comprehensible manner P3.4.2 numeracy – accurately interpret numerical data and their significance for the safe delivery of care P3.4.3 information technology and management – interpret and utilise data and technology, taking account of legal, ethical and safety considerations, in the delivery and enhancement of care P3.4.4 problem solving – demonstrate sound clinical decision making which can be justified even when made on the basis of limited information 4 Personal and professional development O4.1 Demonstrate responsibility for one’s own learning through the development of a portfolio of practice and recognise when further learning is required O4.1.1 identify specific learning needs and objectives O4.1.2 begin to engage with, and interpret, the evidence base which underpins nursing practice O4.2 Acknowledge the importance of seeking supervision to develop safe nursing practice P4.1 Demonstrate a commitment to the need for continuing professional development and personal supervision activities in order to enhance knowledge, skills, values and attitudes needed for safe and effective nursing practice P4.1.1 identify one’s own professional development needs by engaging in activities such as reflection in, and on, practice and lifelong learning P4.1.2 develop a personal development plan which takes into account personal, professional and organisational needs (continued) 40 Domain 4 (continued) Guidelines for Completing the Common Foundation Programme Portfolio Outcomes for entry to chosen branch Standards of proficiency for entry to the register P4.1.3 share experiences with colleagues and patients and clients in order to identify the additional knowledge and skills needed to manage unfamiliar or professionally challenging situations P4.1.4 take action to meet any identified knowledge and skills deficit likely to affect the delivery of care within the current sphere of practice P4.2 Enhance the professional development and safe practice of others through peer support, leadership, supervision and teaching P4.2.1 contribute to creating a climate conducive to learning P4.2.2 contribute to the learning experiences and development of others by facilitating the mutual sharing of knowledge and experience P4.2.3 demonstrate effective leadership in the establishment and maintenance of safe nursing practice (NMC, 2004, pp. 26–34) Appendix 2 Example of evidence written by a student based on a unit activity (UA) 41 Appendix 2 Example of evidence written by a student based on a unit activity (UA) The unit activity asked students to find out about their local manual handling policy and how it is put into practice in their workplace. Here is an example of the completed activity that a student submitted in her Portfolio as evidence for NMC O.2.4, O.2.5, O.2.7 and O3.1, followed by some comments. To find out about the local policy I contacted the back care adviser in the Trust, who confirmed that the Trust has a minimal handling policy. However, she stressed the importance of wards having the correct equipment and knowing when and how to use it properly. She said that carrying out assessments using the Trust’s moving and handling documentation is really essential, and this is an area a lot of wards need to improve on as a good assessment should lead on to the correct techniques and equipment being used for patients, and good communication between the team members. Thinking about the ward I am working on, I have noticed that moving and handling assessment documentation is not filled in for all patients. We have a moving and handling link nurse on my ward and I talked to her about this. She said that she has been talking to other members of the team about how we can improve our moving and handling assessment documentation. She is going to bring it up at the next ward meeting. She said that the assessment documentation forms have been in place for about a year now. We looked at one of the forms together and completed it for a patient who was admitted last night and had not yet had a moving and handling assessment carried out. I feel the form is quite straightforward to follow and it did not take too long to complete, especially as I had been looking after her this morning so I knew her capabilities. We documented that a slide should be used to help her move up the bed. She is able to transfer from bed to chair or chair to bed with one person assisting. In the ward, as well as slides, we have an electronic hoist and all staff seem confident with using it. I have met a few patients who are scared of the hoist but we always start off by finding out if they’ve been in the hoist before and talking to them about it, and reassuring them about its safety. If their families are around we always explain about using the hoist to them too. 42 Guidelines for Completing the Common Foundation Programme Portfolio Comments The above account would be strengthened by attaching an anonymous copy of the completed moving and handling assessment form and by asking the moving and handling link nurse to verify the assessment form and this account by signing and dating it. The account would be strengthened further by making links to the relevant evidence base on moving and handling practice. Appendix 3 Example of testimony written by a practice supervisor (T) 43 Appendix 3 Example of testimony written by a practice supervisor (T) Observation record On Friday 9th September 2005 I observed student nurse O’Brien provide one-to-one care (special) for a client who was at risk of self harm. Nurse O’Brien was under my direct supervision for the duration of the shift. During this time Nurse O’Brien communicated appropriately with the client. She addressed the client by her preferred name at all times. She demonstrated skills of listening when the client was telling her of her frustration at ‘being followed’ (one-to-one care). Nurse O’Brien explained clearly the reason for this care, and when the client started shouting she remained calm, and in an assertive but non-threatening tone asked the client to stop. She allowed the client to vent her frustration, recognising the importance of silence and the limitations of trying to engage the client in a conversation at this time. She refused to be drawn into the client’s tirade of abuse against ‘all the staff’. Once the client had finished expressing her frustration she encouraged her to sit down and watch television, explaining that she, as her ‘special’, could then sit with the client less obtrusively, concurring with the preference the client had stated. Once the client was settled she engaged her in a conversation about the television programme. Nurse O’Brien discussed the incident with me at the end of the shift, showing insight into the client’s perception of one-to-one care, but also recognising that her paramount duty of care was to maintain her client’s safety, even though this might be in opposition to the client’s wishes. She used evidence from the KYN107 course materials on communication strategies to underpin her practice, and undertook a web search using the phrases ‘communication skills’, ‘de-escalation’ and ‘anger management’. NAME: JANE BROWN POSITION: STAFF NURSE SIGNATURE: J. Brown DATE: 9/9/05 Comments This evidence would be strengthened by providing evidence of the web search results in the Portfolio. This evidence could be used to support NMC O1.2, O2.1, O2.2 and O3.1. 44 Guidelines for Completing the Common Foundation Programme Portfolio Appendix 4 Peer testimony of student practice learning The Pre-Registration Nursing Programme is a work-based learning programme offered in partnership with health care providers. Students are employees of our partners and have differing degrees of experience within these settings. This diversity of workplace settings and experience enriches the programme and enhances the opportunities for shared learning. Students can and do take advantage of these opportunities in order to broaden their experience. In order to ensure that students who are experienced practitioners in their own practice area do not have this expertise devalued, and to maintain probity for the programme, the following guidance is provided. It is acceptable for experienced practitioners, who may also be students on the Pre-Registration Nursing Programme, when working within their own practice area to provide witness statements for students who may be participating in complementary or contrasting practice experience within this practice setting. Such statements from peers are acceptable as forms of testimony and can contribute to the student’s evidence base of practice-based learning. Experienced practitioners who are fellow students on the programme cannot act as assessors. The verification of practice hours/experience/achievement of outcomes/standards of proficiency should be undertaken only by qualified practitioners who have been assigned as mentor or associate mentor for the student. Fellow students, however experienced within their own practice setting, cannot be assigned as mentor or associate mentor to other students on the programme. At no time during practice learning is it appropriate for members of a student’s own family or someone who is known personally to them to act as their mentor or associate mentor. If such circumstances should arise, the advice and guidance of the programme tutor should be sought. Appendix 5 Example of a summary account written by a student (SA) 45 Appendix 5 Example of a summary account written by a student (SA) Assisting a patient to eat During my spell of duty on 23/8/05 I was caring for a patient who had senile dementia and who was no longer eating enough. Staff nurse asked me to supervise and assist Mrs X to eat her dinner, ensuring she maintained an adequate food and fluid intake. Mrs X was often agitated and frequently left her meals only half eaten when left to eat alone. I sat with her, encouraging her to eat her meal by reminding her that her meal was on the table in front of her. I asked her about things from her past, where she liked to eat and what her favourite foods were. When she seemed confused about how to eat I helped and encouraged her. It was clear that when able to talk of what seemed familiar in terms of events and foods she ate more readily and seemed to be less agitated. Her conversations mentioned food she had enjoyed in her youth such as fresh fruit. I was able to record these foods in her care plan so that when her future menus were completed she could have food she liked for her meals. I was able to encourage her to drink fluids with her meal and found out that she disliked milk of any sort. This may account for her reluctance to drink fluids. This information was also added to her care plan. This experience highlighted that just asking Mrs X what foods she liked or disliked on admission was not sufficient to give us the information. The context of eating and drinking made her talk about these things, and she was able to give more personal and relevant information. Asking her the questions out of context had not elicited the same responses. This also highlighted to me the importance of talking to people and listening to what they say. I was able to make appropriate changes to her care plan. Staff nurse suggested that the dietician should be contacted to visit Mrs X so that a diet relevant to Mrs X’s needs and likes could be incorporated into her care package. I undertook responsibility for this. Comments This item of evidence would be further strengthened by asking the practice supervisor to read, verify and date the account or even write a short testimony or add comments to it. The outcome of the dietician’s involvement could be included as a later piece of evidence, and evidence identifying the importance of healthy diet in people with long-term conditions would further enhance this example. This evidence could be used to support NMC O2.3, O2.4, O2.5, O2.6, O2.10 and O4.1. Printed in the United Kingdom