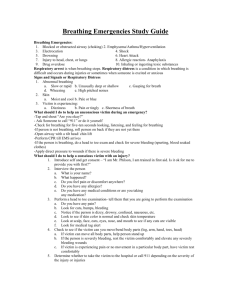
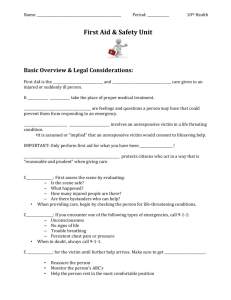
BaSic FirSt aid Lecture Guide
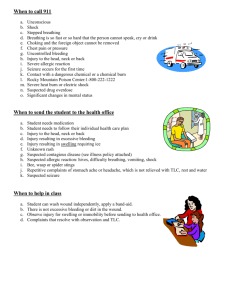
advertisement

Section 2: Basic First Aid Lecture Guide Table of Contents General Information Introduction...............................................2 Responding to Emergencies.....................3 Legal Issues..............................................6 Protection from Infection............................7 Heart Attack...............................................9 Stroke........................................................11 Adult/Child Choking...................................13 Infant Choking...........................................15 First Aid Assessment Assessing a Victim....................................18 Positioning a Victim...................................22 Moving a Victim.........................................23 Medical Emergencies Difficulty Breathing....................................55 Asthma......................................................57 Allergic Reactions.....................................59 Seizures....................................................61 Fainting.....................................................63 Diabetic Emergencies...............................64 Environmental Emergencies Poisoning..................................................70 Heat-related Emergencies.........................74 Cold-related Emergencies.........................77 Bites & Stings............................................80 Prevention and Planning Injuries Bleeding, Shock, Trauma..........................24 Head, Neck & Back Injuries......................34 Chest & Abdominal Injuries.......................42 Muscle, Bone & Joint Injuries....................45 Burns.........................................................50 First Aid Kits..............................................87 Maltreatment of Children...........................87 The Lecture Guide is the primary resource to guide the Instructor through the lecture and move the course along smoothly. The layout follows the layout of the Student Workbook, with similar topic headings. Add statistics or points of interest to the Lecture Guide to customize your presentation. 1. The box under each topic heading indicates: a. DVD Chapter to show at the beginning of the topic. Sometimes you will show multiple DVD chapters, then pause to discuss or practice them. b. DEMONSTRATE: The Instructor demonstrates on a manikin, student volunteer, or him or herself. c. PRACTICE: Skill for students to practice. A skill that is tested will say (Skill ) next to it. Skill Check Option 1: Use Skill Sheets to check off each step of a skill as your student successfully demonstrates it. Option 2: Use a Skill Summary to check off a completed skill. d. SUPPLIES: Equipment or supplies needed to teach each topic. 2. Some topics are optional depending on the needs of the workplace and students. a. e.g. Applying a splint, infant choking care 3. A dotted line separates the topic introduction from the rest of the topic. 4. Gray shaded boxes that say ‘Senior’ are only taught with the workbook, “CPR, AED and First Aid for the Senior Community.” 5. Gray shaded boxes that say ‘Child’ are only taught with the workbook, “CPR and First Aid for Childcare Providers.” 6. Review ‘How Would You REACT?’ pages with your students. The questions have the correct answers in bold. The scenarios will vary according to the details you give the students. Visit www. emssafety.com/Login for suggested scenario responses. You may also substitute your own scenarios which apply more specifically to the needs of the students and workplace. Basic First Aid Lecture Guide 1 Basic First Aid Introduction Instructor Introduction • Introduce yourself; give your qualifications and experience. • Questions are welcome. • Locations of bathrooms, exits, etc. • Provide breaks during the course. Why are you here? • Your workplace or profession requires it • You want to learn for your own knowledge Why should you learn First Aid? • > 123M visits to emergency department each year in U.S. • > 1/3 of visits are for injuries. • Overcome barriers to act: o Fear of doing the wrong thing or hurting someone o Fear of catching a disease o Panic or not knowing what to do • Goal: Respond safely, confidently and effectively in an emergency. What will you learn today? • Quickly recognize an emergency • Assess a victim and recognize life-threatening conditions • Know when to call 9-1-1 • First aid treatment for common illnesses and injury • Things you can do to prevent an emergency How will you learn? • DVD, workbook, lecture, demonstration, hands-on practice, discussion o Emphasize skills and confidence-building over lecture. • Must pass skills and written test to receive a course completion card. o Instructor’s job is to help you learn and pass this course. o Card is valid for up to 2 years. 2 years is too long to remember everything in an emergency. Must review and refresh your learning periodically. o Receive access for 2 years to a digital workbook online. Let Instructor know privately if: • Any medical or physical conditions that may limit your participation • Latex allergy (unless all classroom supplies are latex-free) Follow state, local, and workplace regulations and policies. • Some first aid treatments may be restricted by state, local, or workplace regulations. o e.g. Epinephrine auto-injector; asthma inhaler • Although you may be taught and tested on some treatments that are restricted in certain regions, this does not authorize you to perform them while giving first aid. • Learn your state, local, and workplace regulations. 2 Basic First Aid Introduction © 2011 EMS Safety Services, Inc. Responding To Emergencies DVD Ch: 1, 2 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives: • Be able to recognize an emergency and evaluate a scene for safety. • Know when and how to activate EMS and interact with EMS. Key Concepts • Emergency scenes can be dangerous. • Rescuers can quickly become victims. • Caution and common sense can save your life. REACT to an Emergency Recognize an emergency • Screams, panic; seriously ill or injured person; victim or bystanders agitated or threatening • Suspicious environment; collision or stopped vehicle; environmental hazard • Remain calm; stay aware of your own safety. • Consider resources and options. Environment Size up the scene from a safe distance. Common hazards include: • Blood and body fluids: Use personal protective equipment on every scene. • Traffic: Use your vehicle, hazard lights and bystanders to control traffic around the scene. Watch for jagged metal and broken glass. Don’t turn your back to oncoming traffic. • Fire or smoke: Stay low to avoid smoke inhalation, and focus on escaping. If possible, drag the victim to safety. Never enter a smoke-filled environment. • Wet, icy or unstable surface or structure: Slips, falls and vehicle movement can cause additional injuries to bystanders and rescuers. Avoid walking onto a frozen lake or pond if the stability of the ice is unknown. • Downed electrical wires: Do not enter the scene; maintain a safe distance. If downed lines are near your car, stay inside the vehicle. • Hazardous materials, chemicals and gases: Unusual smells, hissing sounds, liquids, hazardous containers; dead birds, animals, and fish could indicate a biological or chemical hazard. Leave the area and report it immediately. • Open water, strong currents: Do not attempt a water rescue without professional training and equipment. It only takes a foot of swift moving water to move a car downstream. • Confined space: Could be a cave, sewer, drainage culvert, or someone’s garage. Look for clues such as more than 1 victim with no apparent injury. Do not enter without training and proper equipment. • Hostile environment: Do the victim or bystanders appear agitated or threatening? Basic First Aid Lecture Guide Responding To Emergencies 3 Size-up the victim(s). • How many? • What is their general condition? Are they moving? • Try to identify cause of illness or injury. • If more than 1 victim, decide who needs help the most. If unsure, help the person closest to you. Activate EMS now if the scene is dangerous or if there is an obvious life-threatening injury or illness. Tip Before you enter an emergency scene, consider how you will exit. Identify two possible exits. Assess the victim • Go to the victim’s side and assess response and breathing. • Look for serious illness or injury, such as difficulty breathing or severe bleeding. Call for help • If the victim has a life-threatening condition, get help. • Shout for help; call 9-1-1 or your emergency response number. o If not sure it’s an emergency, activate EMS. The dispatcher will ask questions to determine if it’s an emergency. Treat the victim • Treat life-threatening conditions first. o If unresponsive, call 9-1-1 (activate EMS) and assess breathing. o If no breathing or only gasping, begin CPR (compression-only CPR if untrained). o If severe bleeding, control with direct pressure. • Treat the victim in the position found. Only move the victim if danger or need to reposition for essential care or position of comfort. When you call 9-1-1 the dispatcher will ask: • Name, location, call back phone number. • What happened, number of victims, general condition, what aid is being given • Follow instructions, and always hang up last. When EMS responders arrive: • Continue care until you are told to stop. • Tell EMS what time the event occurred, what time you arrived, and what care has been given. Senior • Give EMS a printed list of medications if available. • If the person wears glasses or hearing aids, try to provide these before EMS transports the person. 4 Responding To Emergencies © 2011 EMS Safety Services, Inc. Child • Give EMS responders a copy of the child’s Emergency Information Form from the school or childcare facility. • Follow your school or childcare facility’s Emergency Action Plan for contacting parent or legal guardian and for supervising other children. Sum it up • Remain calm. • Assess the scene from a safe distance. • Check for hazards and resources before focusing on the victim. • If the scene is not safe, do not enter; call 9-1-1. • Do not become a victim. Rescuer Stress Learning Objectives • Understand that there might be physical, mental, and emotional consequences to providing care in an emergency. Key Concepts • It’s normal to feel stress after an incident. • Each rescuer will respond differently to stress depending on: o Experience o Personality o Seriousness of the incident o Outcome • Rescuer stress may cause changes in emotions, ability to concentrate, appetite, sleep, and other physical symptoms. Don’t ignore signs and symptoms of rescuer stress. • Take care of yourself. o Eat properly. o Avoid alcohol, drugs and caffeine. o Exercise. o Get enough rest. • Talk about your feelings. o Find someone who has had a similar experience. o Don’t judge yourself for your actions. o Obtain professional help if needed. DISCUSS: • Has anyone here responded to a serious emergency? • Will you discuss what emotions you felt after the emergency was over? • How did you deal with the emotions? Basic First Aid Lecture Guide Responding To Emergencies 5 Legal Issues DVD Ch: 3 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives: • Know the common elements of the Good Samaritan Law. • Understand the need for consent, right to privacy and right to refuse care. Key Concepts • Some people have a duty to respond to an emergency. • Other people respond voluntarily. Good Samaritan Law • Purpose: encourage people to help in an emergency. • Requirements: o Respond voluntarily (no ‘duty to act’) o Not getting paid to respond o Provide care with good intentions o Stay within the limits of your training o Not reckless or careless when giving care o Not abandoning the victim after beginning care Gain Consent Before Treating • Give your name, level of training, and the problem. Ask if you can help. Types of Consent • Expressed consent: Victim expresses desire for aid • Implied consent: Consent is assumed (unresponsive person) • Minor’s consent: A parent or legal guardian must give consent. If condition is life-threatening, treat under implied consent. Right to Refuse Care • A mentally competent adult can refuse care at any time. • Observe the situation from a distance and call 9-1-1 if needed. Right to Privacy • Do not give out the victim’s information to coworkers or bystanders. • Give information to EMS responders and to the person in charge of workplace safety. 6 Legal Issues © 2011 EMS Safety Services, Inc. Senior Do Not Attempt Resuscitation (DNAR) • Some people may have a DNAR order from their doctor. o Usually specific to out-of-hospital cardiac arrest. o Must be put in place before an emergency. • If DNAR order is in place, do not begin CPR. o Call 9-1-1 and tell the dispatcher that the person is unresponsive and not breathing, and has a DNAR order. • DNAR protocols may be different in each state. • Learn about your state’s Advance Directives from your doctor or attorney. Sum it up • A designated first aid responder has a duty to act when at work. • Once you begin care, do not leave the victim until help arrives. • Request consent before giving care. • Do not provide treatment that you are not trained to give. Protection from Infection DVD Ch: 4 DEMONSTRATE: Glove removal PRACTICE: Glove removal (Skill ) SUPPLIES: Disposable gloves Skill Sheet 3 Instructor Note: Skip this chapter if you will be certifying your students in the annual Bloodborne Pathogens awareness training in Section 3 of this Instructor Manual. Learning Objectives: • Understand how to help prevent BBP exposure and what to do if you are exposed. • Demonstrate the skill of disposable glove removal. Key Concepts • The OSHA Bloodborne Pathogens Standard requires the employer to help protect you from exposure to BBP. • Use precautions with every emergency to protect yourself. • Hand washing is an important part of infection control. Bloodborne Pathogens • Bloodborne pathogens are disease-causing microorganisms in blood. • Most serious: HIV, Hepatitis B, Hepatitis C • May be transmitted during an emergency when giving first aid, handling contaminated sharp objects, cleaning a blood spill. Basic First Aid Lecture Guide Protection from Infection 7 Routes of transmission: • Splash to eye, mouth or nose • Opening in skin (cut, scab, rash, hangnail) Universal Precautions Universal Precautions & Body Substance Isolation provide protection. • Assume all blood and body fluids are infectious, except sweat. • Take precautions with all victims, even children. • Use personal protective equipment. o Disposable gloves, gown, mask, goggles or face mask, CPR barrier o Choose the right equipment for each emergency. o Wash hands thoroughly immediately after glove removal. o Wash with soap and water for at least 20 seconds. o If hands not visibly soiled and running water is not available, use hand sanitizer, then wash ASAP. What to do if you’re exposed: • Immediately remove your gloves. • Wash your hands and the exposed area thoroughly with soap and water. • Follow your workplace Exposure Control Plan. Removing Soiled Gloves DEMONSTRATE: Soiled glove removal PRACTICE: Soiled glove removal Instructor Note: Use Skill Sheet 3 - Glove Removal, Choking Care Cleaning after an Emergency • Wear personal protective equipment. • Clean the spill with paper towels or an absorbent powder. • Pick up sharp objects or broken glass with tongs or brush and dustpan. • Disinfect with 10% bleach and water or another disinfectant. • Dispose of soiled personal protective equipment according to workplace policy. • Wash your hands. Tip 8 If you don’t have a biohazard bag or container, place the contaminated items in a leak-proof plastic bag and seal it. Dispose of it according to your workplace policy. Protection from Infection © 2011 EMS Safety Services, Inc. Airborne Pathogens • Other diseases can be spread when an ill person coughs or sneezes. • Protect yourself by: o Getting a flu vaccine. o Washing your hands often. o Avoiding contact when possible with people who may be contagious. Sum it up • Keep first aid kits stocked with personal protective equipment. • If you don’t have personal protective equipment with you, use whatever is available: o e.g. To control bleeding, have the victim apply the pressure, or use layers of clean cloth or extra gauze. Heart Attack DVD Ch: 5 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives: • Know how to recognize a heart attack and the proper rescuer actions. • Understand the importance of early activation of EMS. Key Concepts • Heart disease is the leading cause of death in the U.S. • Heart attack can lead to cardiac arrest. • More than 1.25 million Americans have a first or recurrent heart attack every year. • About 70% of the deaths from heart attack occur before the victim reaches the hospital. • Call 9-1-1 early for any signs of heart attack. Coronary Artery Disease (CAD) • The build-up of fatty deposits in blood vessels. o Coronary arteries narrow and harden. o Vessels can become blocked. o Process takes years. • Heart disease is preventable. What is a heart attack? • The heart pumps blood throughout the body. • Coronary arteries deliver oxygenated blood to the heart. Basic First Aid Lecture Guide Heart Attack 9 • A blocked coronary artery deprives the heart of oxygen. o Results in death of heart muscle (heart attack). o If enough critical heart tissue is affected, causes cardiac arrest. o Can end a life in seconds. Signs and Symptoms of Heart Attack • Chest discomfort: • Pale, cool, sweaty skin o Pain, pressure, tightness, squeezing, fullness. • Shortness of breath o Discomfort may radiate to the arms, neck, back, jaw, or abdomen. • Nausea, vomiting o Often mistaken for heartburn or indigestion. • Dizziness, fainting or unresponsiveness • Unexplained fatigue Treatment of Heart Attack 1. Call 9-1-1 and get an AED if available. 2. Position of comfort, usually sitting. 3. Calm and reassure the person. 4. Offer 1 adult or 2 baby aspirin for victim to chew. o Make sure no allergy to aspirin, signs of stroke, or recent bleeding problems. o Make sure the victim is alert and can swallow. 5. If victim becomes unresponsive, check breathing. o If no breathing or only gasping, begin CPR (compression-only CPR if you are untrained). o Use the AED when it arrives. Don’t Delay calling 9-1-1 • If any signs and symptoms are present. • If the symptoms fade and return. • To give aspirin. Calling 9-1-1 can mean the difference between heart attack & cardiac arrest. • Paramedics can provide treatment before cardiac arrest occurs. Sum it up • Heart attack victims often deny or ignore symptoms, or say there is another cause. • Be alert to less common symptoms in women, diabetics, and older people. • Fast recognition of heart attack symptoms gives the best chance of survival. • Clot-busting medications can dissolve the clot. • Only effective in the first few hours of a heart attack. 10 Heart Attack © 2011 EMS Safety Services, Inc. Stroke DVD Ch: 6 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives: • Know how to recognize a stroke and the proper rescuer actions. • Understand the importance of early activation of EMS and early treatment at a hospital. Key Concepts • Stroke is the 3rd leading cause of death in the U.S. • 800,000 strokes each year in the U.S. • Call 9-1-1 early for any signs of stroke. What is a stroke? • A stroke is like a heart attack occurring in the brain. • Caused by a clot or bleed in the brain. • Symptoms may be minor or severe. • Many survivors are permanently impaired and struggle with daily activities. Stroke Signs and Symptoms Occur Suddenly • Weakness or numbness of arm or leg, usually on one side of the body • Facial droop or paralysis, usually on one side o Lopsided smile • Difficultly speaking o Unintelligible, confused or garbled speech • Difficulty eating, swallowing, or managing secretions o Coughing, choking, drooling • Loss of balance or coordination, difficulty walking o Falling, difficulty with movement or physical tasks • Decreased mental status o Confusion, anxiety, unresponsiveness • Changes in sensation o Numbness or tingling o Inability to sense body position • Severe headache or dizziness • Change in vision o Blurred, loss of vision in one eye, change in field (area) of vision Basic First Aid Lecture Guide Stroke 11 Treatment of Stroke 1. Call 9-1-1 (activate EMS). 2. Protect the airway. a. May have trouble controlling the tongue or managing secretions. b. If fluids or vomit in the mouth, place in the recovery position to allow fluids to drain. 3. Calm and reassure the victim. 4. Note the time that symptoms began. If the person is unresponsive: 5. Check for breathing. 6. If no breathing or only gasping, begin CPR. Transient Ischemic Attack (TIA) • Often called a baby stroke. • Warning sign of a future stroke. • Due to a temporary lack of oxygen. • Symptoms last from a few seconds to 24 hours. Time is critical. • Treat most strokes with clot-busting medication (fibrinolytic therapy). o Same as with a heart attack. o Only effective in the first few hours of a stroke. • Early recognition of stroke can make the difference between life and death or between complete recovery and lifelong disability. STRoke Assessment Use STR to quickly recognize common signs of a stroke. • Smile: Ask person to smile. o Both sides of face should move equally. • Talk: Ask person to repeat a common phrase. o Listen for slurred or incorrect words. • Reach: Ask person to close eyes and raise arms. o Look for arm drift or weakness on one side. Sum it up • Recognize the signs and symptoms of stroke. • Do not wait to see if the symptoms will disappear (TIA). • Call 9-1-1 and get help early for the best chance of survival and recovery. 12 Stroke © 2011 EMS Safety Services, Inc. Adult/Child Choking DVD Ch: 7 DEMONSTRATE: Adult/child choking care PRACTICE: SUPPLIES: Adult/child choking care CPR or choking manikin (Skill ) Skill Sheet 3 Learning Objectives: • Recognize choking in the adult or child. • Demonstrate choking management of a responsive victim. • Understand rescuer actions if the victim becomes unconscious. Key Concepts • Choking is a preventable emergency. • Most choking incidents occur in children younger than 5 years. • Treatment is the same for an adult or child. • Act quickly, because severe choking will result in death if not treated. Recognize choking • Choking is often confused with other emergencies. o e.g. Heart attack, asthma, seizure, drug overdose • Consider what the person was doing to help recognize choking: o Talking or drinking alcohol while eating o Eating too fast or not chewing food completely o Wearing dentures while eating (difficult to tell if food is chewed) o Walking or running while eating or chewing gum • Universal sign of choking: 1 or both hands at the throat. DEMONSTRATE: Universal sign of choking Mild Obstruction • The airway is partially blocked. • If the person can forcefully cough or speak, do not interfere. • Forceful coughing is the best way to relieve an obstruction. o Ask, “Are you choking?” o If can cough or speak, encourage coughing. o Watch for progression to a severe obstruction. o Send someone to call 9-1-1 if coughing is prolonged. Severe Obstruction- Act quickly! • The airway is completely blocked and the person cannot breathe. • Use abdominal thrusts (Heimlich maneuver) to clear the airway. Basic First Aid Lecture Guide Adult/Child Choking 13 DEMONSTRATE: Abdominal thrusts on a manikin or student volunteer Instructor Note: Do not perform actual abdominal thrusts on a student volunteer. Senior If the victim is in a wheelchair: • Perform abdominal thrusts if you can quickly access the right location. o May depend on wheelchair style, size and sitting position of victim. • Perform chest thrusts if you cannot perform abdominal thrusts. Child To perform abdominal thrusts on a small child, the rescuer may need to kneel down behind the child to get into the right position. Unresponsive Choking Person If the victim becomes unresponsive, perform CPR. 1. Lower the person to the ground. 2. Send a bystander to call 9-1-1. a. If you are alone with an adult victim, go call 9-1-1 yourself. b. If you are alone with a child or infant, go call 9-1-1 after 2 minutes of CPR. 3. Perform CPR with the added step of looking in the mouth after each set of compressions. a. If the object is seen, remove it. Do not ‘blind sweep’ the mouth. 4. Continue CPR. Chest Thrusts If pregnant or too large to reach around the abdomen, use chest thrusts. • Stand behind the person and reach under the arms and around the chest. • Place one fist in the center of the chest. o Same location as chest compressions • Grasp the fist with your other hand. • Perform continuous backward thrusts. Choking Prevention Tips • Eat slowly and chew food completely. • Do not talk or laugh with food in your mouth. • Adults: Don’t drink too much alcohol while eating; make sure dentures fit well. • Children: Cut food into small pieces; cut round food into halves or quarters. • Keep children seated and supervised at mealtime. • Protect young children from objects small enough to fit through the center of a toilet paper roll. 14 Adult/Child Choking © 2011 EMS Safety Services, Inc. Sum it up: • Suspect choking if the person suddenly stops talking or breathing. • Mild obstruction: encourage coughing; do not interfere. • Severe obstruction: Act quickly; call 9-1-1 if you are unable to help. • Everyone who has had abdominal thrusts should be seen by a doctor. PRACTICE & SKILL CHECK: Adult / child choking care Instructor Note: Use Skill Sheet 3 - Glove Removal, Choking Care • Simulate on a partner or practice on a choking manikin. • Tell the students that they will not give actual abdominal thrusts on a person during skills practice. • Closely supervise students to ensure that they do not give actual abdominal thrusts. Infant Choking (optional) DVD Ch: 8 DEMONSTRATE: Infant choking care PRACTICE: Infant choking care (Skill ) SUPPLIES: Infant manikin Skill Sheet 3 Instructor Note: This topic is required for Infant CPR certification. Learning Objectives: • Understand the common causes, prevention, and signs of choking. • Demonstrate choking management of a responsive infant victim. • Understand rescuer actions if the infant becomes unconscious. Key Concepts • An infant cannot communicate to you that he or she is choking. • Forceful coughing is the best way to relieve an obstruction. Recognize choking in an infant: • Unable to cough or cry effectively • No breathing or difficulty breathing (wheezing or high-pitched sound) • Bluish skin color • Bulging, tearing eyes • Panic or distressed facial expression Mild Obstruction • If can forcefully cough or cry, monitor breathing. • Watch for progression to a severe obstruction. • Call 9-1-1 if coughing is prolonged. Basic First Aid Lecture Guide Infant Choking 15 Severe Obstruction- Act quickly! • The airway is completely blocked and the infant cannot breathe. • Use back blows and chest thrusts to dislodge the object. DEMONSTRATE: Back blows and chest thrusts on an infant manikin Unresponsive Infant If the victim becomes unresponsive, perform CPR. 1. Look for the object in the mouth after each set of compressions. o If seen, remove the object. Do not ‘blind sweep’ the mouth. 2. Continue CPR. 3. If you are alone, call 9-1-1 after 2 minutes of CPR. Sum it up • Prevent choking before it becomes an emergency. PRACTICE & SKILL CHECK: Infant choking care* Instructor Note: Use Skill Sheet 3 - Glove Removal, Choking Care *Required for Infant CPR certification 16 Infant Choking © 2011 EMS Safety Services, Inc. How Would You REACT? QUESTIONS 1 Possible hazards at an emergency scene may include: a. b. c. d. e. 2 Fire or smoke Blood or body fluids Traffic Unstable structures All of the above Implied consent allows you to treat an unresponsive person. True SCENARIOS Home You are talking with your wife when she suddenly slumps in her chair. She cannot maintain her position in the chair and does not make sense when she speaks. How would you REACT? Community False You see a car stopped on the other side of a busy road. There is someone sitting slumped over the wheel. How would you REACT? 3 You do not need to wear gloves when giving care to a bleeding child because he or she will not carry bloodborne pathogens. 4 True Women may experience different heart attack signs and symptoms from men. True 5 False School You are supervising the school lunch when you notice a young child stand up and clutch his throat. He looks panicked. You ask what’s wrong, but he cannot speak. How would you REACT? False Work If a victim has difficulty speaking or weakness on one side of the body, he or she should: a. b. c. d. Wait to see if it will pass Call a doctor Drive to the emergency department Call 9-1-1 Basic First Aid Lecture Guide A 50-year-old coworker complains of chest discomfort. He says not to worry because he had spicy food for lunch. He looks sweaty and his breathing is labored. How would you REACT? How Would You REACT? 17 Assessing a Victim DVD Ch: 9, 10 DEMONSTRATE: Assessing a victim PRACTICE: Assessing a victim SUPPLIES: Skill Sheet 4 (Skill ) Learning Objectives: • Understand the scene size-up, initial assessment, and on-going assessment, and how to perform them. • Identify common situations in which EMS should be activated. • Demonstrate the initial assessment of a victim. • Know how to prioritize life-threatening conditions. Key Concepts • Ensure your own safety. • Assess a victim in the position found. • Treat life-threatening conditions first. Scene Size-up • Size-up the scene for safety before you enter. o If not safe, call 9-1-1 and follow dispatcher instructions. • Size-up the victims. o How many, general condition, possible cause of injury or illness. • Suspect serious injury if: o Vehicle, motorcycle, bicycle accident o Fall from greater than standing height o Explosion or gunshot • Identify available resources. o Bystanders, first aid kits, personal protective equipment, cell phones Initial Assessment 1. Assess response: • Approach the victim from the side and gather a general impression. Appears unresponsive: • If appears unresponsive, tap the shoulder and shout, “Are you okay?” • If no response, have someone call 9-1-1 (activate EMS), get the first aid kit and AED. • Go call yourself if you are alone with an adult victim. Responsive: • Gain consent. Give your name and training, and ask if you can help. • Ask questions to determine what happened. What is the chief complaint? 18 Assessing a Victim © 2011 EMS Safety Services, Inc. 2. Assess Breathing Unresponsive: Scan the chest for breathing. • If no breathing or only gasping, begin standard CPR if you are trained. o Give continuous chest compressions if you are not trained. • If breathing, continue assessment and closely monitor breathing. Responsive: Check for the quality, rate and effort of breathing. • Listen for noisy breathing. Is the airway clear? • Is the person working hard to breathe? • Can the person speak? Is the person speaking in broken sentences? • Is breathing fast or slow? 3. Assess Head-to-Toe • Look head-to-toe for obvious signs of injury o e.g. Bleeding, bruising, burns, twisted limbs o Smell for chemicals which might indicate poisoning. • Assess appearance o Color, sweating, temperature, movement, position Assess temperature with the back of your gloved hand on the person’s forehead. Normal skin is warm, dry, and good color. • Treat life-threatening conditions first. o Prioritize problems with response, airway, breathing, circulation. o If you find a life-threatening condition, stop the assessment and give care. (e.g. Control bleeding with direct pressure.) 4. Look for Medical Alert Jewelry • Look for a medical alert necklace, bracelet, or shoe tag. • Might indicate heart condition, diabetes, seizure disorder, asthma, allergy, etc. Tip Check the victim’s cell phone for an ICE contact: In Case of Emergency. It will usually be a family member or close friend. Senior Caregiver Assessment: • Make movements slow and deliberate. • May be difficult to differentiate between new problem and symptoms from a chronic medical condition. o e.g. Is mental confusion from hypoglycemia or from a previous stroke? o Interview family members to find out. • May deny symptoms because does not want to risk losing independence. o May not want to be a bother. o May not want to go to the hospital. Basic First Aid Lecture Guide Assessing a Victim 19 Communication: • Speak slowly and clearly, but do not exaggerate your speech. • May answer questions slowly; be patient. o Medications or fatigue may slow response. • If impaired vision and hard of hearing, do not assume the person cannot understand. o Talk directly to the person, not just to family members. Vision • Stand where the person can see you. • Stay within view as you ask questions. • If the person wears glasses, get them for the person. Hearing • If the person wears hearing aids, get them for the person. • Turn down background noise (TV, radio, loud talking). • Speak in lower frequencies. o Difficulty hearing high-pitched voices. o May understand male voices more easily. • If cannot hear you, consider writing questions down. Child Assessment: • If more than 1 child, go to the quiet one first. May be unresponsive. • Get down to child’s level. • Take your time with the assessment. o Speak slowly and clearly. o Make movements slow and deliberate. o Ask a young child to point to where it hurts. Infants: The most difficult to assess, because they cannot communicate verbally. • Be alert for signs of listlessness or exhaustion, which indicate severe distress. • Support the head of infants younger than 4 months. Age 1-5: Easily scared by strangers. • Do not remove clothing, and avoid any unnecessary touching. • Use observation to help your assessment. Age 6-12: When injured or stressed, may behave younger than their actual age. • Be honest if something is going to hurt. • Work slowly, avoiding any surprises. • Give a simple explanation of what you are going to do. Involve parents or caregivers • Do not separate the child from family or caregiver. 20 Assessing a Victim © 2011 EMS Safety Services, Inc. • Give the parent a task to perform. o Apply pressure on a bleeding wound. o Hold the child. o Call 9-1-1. • Ask for help reassuring a frightened child. • Ask about a child’s medical history. Follow your school or childcare facility’s Emergency Action Plan. • Notify child’s parent or emergency contact. • Supervise other children during the emergency. • Send an adult to accompany the child to the hospital and remain there until a parent or legal guardian arrives. • Talk with other children who witnessed the emergency. On-Going Assessment Reassess the scene and your victim while you wait for professional responders to arrive: 1. Ensure the scene is still safe. 2. Reassess and continually monitor responsiveness and breathing. 3. Observe for changes in mental status (victim becomes confused or unresponsive). 4. Calm and reassure the victim. Call 9-1-1 if: • Unresponsive or altered mental status • Difficulty breathing or no breathing • Severe or uncontrolled bleeding • Signs of heart attack (chest discomfort, radiates to arm, jaw, neck, back, stomach) • Signs of stroke (sudden severe headache, slurred speech, arm or leg weakness, especially on one side of the body) • Pressure or pain in the abdomen that does not go away • Severe, persistent vomiting, vomiting blood or passing blood in the stool • Severe allergic reaction • Pregnancy emergency • Seizure • Critical burn, electric shock • Suspected poisoning • Head, neck or back injury • Possible broken bone • Fall greater than standing height • Any time you are not comfortable with a medical or dangerous situation Basic First Aid Lecture Guide Assessing a Victim 21 Sum it up • Activate EMS early if danger or serious illness or injury. • At every emergency scene you will: o Assess the scene for safety. o Get the first aid kit and AED. o Put on personal protective equipment. o Assess the victim. DEMONSTRATE: Assessing a victim PRACTICE: Assessing a victim Instructor Note: Use Skill Sheet 4: FA Assessment, Bleeding Positioning a Victim DVD Ch: 11 DEMONSTRATE: Tripod position PRACTICE: SUPPLIES: Learning Objectives • Identify when to use the recovery position. • Describe different positions for various conditions. Key Concepts • Move a victim only if immediate danger or needs essential care. • Use different positions for different conditions. Unresponsive Victim Unresponsive Victim • The airway can become blocked by the tongue, vomit, blood or mucus. • The recovery position keeps the airway open and allows fluids to drain. • Use the recovery position when: o A person is unresponsive and has vomit, fluid or blood in the mouth. o A lone rescuer has to leave to get help. • Log roll a victim into the recovery position. o Roll without twisting the spine. o Position should be stable, with the person unlikely to roll further forward or back. • 22 If an unresponsive victim is face down, carefully log roll the victim face up. Positioning a Victim © 2011 EMS Safety Services, Inc. Modified H.A.IN.E.S. recovery position • There are many different types of recovery position. • Use this recovery position especially if you suspect neck or back injury. • End with the victim lying on his side, head supported by his raised arm. Place a pregnant victim on her left side. • Allows blood to flow more freely. • Avoids problems from the weight of the baby pressing down on nerves and blood vessels. Responsive Victim Shock position: lying face up • Use if signs of shock, dizzy or faint Sitting up: semi-reclined, upright, or supported on hands • Use for difficulty breathing DEMONSTRATE: Tripod position • Tripod position is used by people with severe shortness of breath. Position of comfort: The position that is most comfortable • Use for nausea, pain, shortness of breath Sum it up • Use the recovery position for an unresponsive person if you must leave to get help, or to keep the airway open and allow fluids or vomit to drain. • Do not move a trauma victim unless absolutely necessary for essential care. o e.g. CPR, placing a blanket under a victim to insulate from heat or cold, bleeding control, or airway management Moving a Victim DVD Ch: DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Know when a person should and should not be moved. • Identify the “drag and carry” methods for movement of a victim. Key Concepts • Use good lifting techniques to protect yourself. • Only move a victim for essential care such as CPR or airway management, or if there is immediate danger. • Pull or drag the victim in the direction of the long axis of the body. Basic First Aid Lecture Guide Moving a Victim 23 Lifting and Moving Principles • Keep your feet shoulder width apart. • Keep your back straight, abdominal muscles tight. • Bend at the knees, and use thigh and buttocks muscles to lift. • Know your limitations and when to get help. • Lift with the victim held close to your body. • Do not twist your back, but pivot with your feet. Use a log roll to turn the victim. • Hold the victim at the head, shoulder and hip, and roll the person like a log, without twisting the neck or back. • Minimizes motion of the spine, so it is safer if there is suspicion of neck or spinal injury. Emergency Drags • Ankle Drag: Pull by the ankles. • Shoulder Pull: Kneel down behind the head and reach under the armpits. Stand and drag to safety. Use for short distances over rough surfaces. • Blanket Drag: Log roll the victim onto a blanket, wrap the blanket, and drag to safety. • Clothes Drag: Grab the neck and shoulders of the shirt or jacket and support the head with your forearms. Make sure the clothes don’t press on the throat. Emergency Carries • Human Crutch: Support the injured leg and help the person walk on the good leg. • Pack Strap Carry: Pull the person’s arms over your shoulders, cross at your chest and hold the wrists. • Seat Carry: 2 rescuers link both arms to form a seat, and the victim holds your shoulders. o Alternate: Link 1 arm to form a seat, and link the other arm behind the victim’s back. Sum it up • Only drag or carry a person when necessary. • Generally wait for professional responders to arrive and move the victim. Bleeding, Shock and Trauma DVD Ch: 12 DEMONSTRATE: Bleeding control & bandaging Shock treatment PRACTICE: Bleeding control & bandaging (Skill ) SUPPLIES: Gauze pads & rolls Gloves Skill Sheet 4 Learning Objectives 1. Identify the different types of bleeding. 2. Demonstrate how to stop bleeding and apply a bandage. 24 Bleeding, Shock and Trauma © 2011 EMS Safety Services, Inc. 3. Understand assessment and emergency treatment of traumatic injuries. 4. Understand basic wound care, how to recognize and treat shock, and how to help prevent infection. Key Concepts • Minor wounds often stop bleeding without intervention. • Severe, uncontrolled bleeding is life threatening. • Can die of blood loss in just a few minutes. • Control of severe bleeding is a critical treatment that can save a life. • Firm, direct pressure on a wound will control most bleeding. • Apply direct pressure until the bleeding has stopped or trained rescuers arrive. External Bleeding The body contains an average of 10 pints of blood. • Can usually lose 1 pint with no negative effects. o The amount for a blood donation. • Loss of 2 pints may result in shock. • Loss of 5-6 pints usually results in death. ! Children and the elderly have less tolerance for blood loss, and may go into shock sooner than a non-elderly adult. Three types of bleeding: • Arterial: Bright red blood spurting from the wound. • Venous: Dark red blood steadily flowing from the wound. • Capillary: Blood slowly draining or oozing from the wound. Arterial bleeding is most serious due to: • Speed of blood loss • Hardest to control Types of Wounds • Laceration: A cut or torn wound. o e.g. Piece of glass, machinery accident o Often has jagged edges. • Puncture: Usually a deep wound with minimal bleeding. o e.g. Nail, animal bite o Greatest chance of infection. o May cause internal bleeding. • Abrasion: A painful scraping away of skin. • Avulsion: Skin or tissue completely or partially torn from the body. o Usually severe bleeding. Basic First Aid Lecture Guide Bleeding, Shock and Trauma 25 o Fold or replace torn skin if possible. o Wrap the wound as a laceration. o If the skin or tissue is completely torn from the body, salvage it as an amputated part. • Amputation: Loss of body part. Severe Bleeding Treatment of Severe Bleeding The priority is to stop the bleeding. Do not attempt to clean the wound. 1. Scene safety, get the first aid kit and AED, put on personal protective equipment. 2. Lay the victim down. 3. Remove any clothing over the wound so you can see where the bleeding is coming from, and if there is anything embedded in the wound. 4. Apply continuous, firm direct pressure. a. May take more than 10 minutes. b. Add dressings; don’t replace. 5. Treat for shock (lay flat and maintain body temperature). 6. After bleeding has stopped, apply a pressure bandage if needed to secure dressings in place and maintain pressure. a. Especially if you are the only rescuer and you must leave to get help. b. Wrap an elastic or roller bandage around the limb and secure in place. c. Don’t wrap so tightly that it creates a tourniquet effect. Do not peek at the wound to see if it has stopped bleeding. Do not remove any deeply embedded objects, or attempt to clean the wound. Senior If a person takes blood thinning medication, it may take much longer to control bleeding, even with a minor wound. Call 9-1-1 if: • Bleeding is severe or doesn’t stop • Impaled object • Signs of internal bleeding or shock • Suspect head, neck or spine injury Get medical care if: • Wound is large or deep and may need stitches o Stitches should be made within 6-8 hours after the injury. • Dirt or debris remains in the wound • Wound is from a bite, puncture, burn, electrical or chemical injury • Wound is on the head, face or neck • Signs of infection: redness, warmth, increased pain, pus, swelling, fever • May need tetanus shot (none for 5 years) 26 Bleeding, Shock and Trauma © 2011 EMS Safety Services, Inc. Tourniquet Application • Stops blood flow to an arm or leg by compressing the blood vessels. • Can lead to serious complications such as loss of an arm or leg, or even risk your life. • Use only if severe, uncontrolled bleeding from an arm or leg is life-threatening. • A commercial tourniquet is better than a homemade one. Applying a Tourniquet 1. Apply a tourniquet to the limb at least 2” above the injury, but not over a joint. 2. Tighten the rod just to the point that bleeding stops, and secure it. 3. Record the time that you put it on. 4. Notify EMS that a tourniquet was applied, and the time. Shock • Life-threatening condition that occurs when the body’s organs and tissues don’t receive enough oxygenated blood. • Caused by severe injury or sudden illness. • Immediate first aid can prevent shock or stop its progression. • Goals of first aid care: o Treat any obvious cause of shock o Improve blood flow to the brain, heart and lungs o Get emergency medical help • Do not delay calling for emergency help. Suspect Shock if: • Severe bleeding (most common cause of shock): o Large open wounds o Serious injury to chest or abdomen o Severe trauma or fractures • Fluid loss o Severe burns, vomiting, diarrhea, infection • Possible heart attack o Heart cannot maintain blood pressure • Anaphylaxis o Severe allergic reaction o e.g. Allergies to food or drugs, bee stings • Spinal cord injury Signs and symptoms of shock vary according to cause. Basic First Aid Lecture Guide Bleeding, Shock and Trauma 27 Signs and Symptoms of Shock • Rapid, shallow breathing • Thirst • Weak, rapid pulse • Nausea, vomiting • Pale, cool, moist skin • Confusion, agitation • May have red, warm skin with anaphylaxis or septic shock • Fainting, dizziness • Unresponsiveness DEMONSTRATE: shock position and treatment Treatment of Shock 1. Call 9-1-1 (activate EMS). 5. Loosen tight clothing. 2. Lay the victim down. 6. Calm and reassure. 3. Control any external bleeding. 7. Monitor status. 4. Maintain body temperature. a. Cover with a blanket. b. May need to insulate from the ground below. ! Do not give food or drink to a victim of severe bleeding, shock or trauma. Surgery may be required. Signs of shock are not always obvious, especially in children. Suspect shock in cases of severe bleeding. Internal Bleeding • Internal bleeding is concealed within the body and may not be obvious. o Common with car accidents, falls, knife and gunshot wounds o Can be life-threatening • Common causes: Injury to internal organs; fractures; medical condition • Goals of treatment: Prevent shock; get EMS responders on scene ASAP. Signs and Symptoms of Internal Bleeding • Bruised, tender, swollen or hardened skin or tissues, especially in the abdominal area and suspected fracture sites • Chest or abdominal pain • Bleeding from a body opening: Mouth, nose, ear, rectum, vagina, urethra • Blood in vomit: Bright red or coffee ground appearance • Blood in stool: Dark tarry or bright red • Blood in urine: Red, pink or tea-colored • Signs of shock 28 Bleeding, Shock and Trauma © 2011 EMS Safety Services, Inc. Treatment of Internal Bleeding 1. Call 9-1-1 (activate EMS). 3. Calm and reassure. 2. Treat for shock. 4. Monitor status. Traumatic Injuries Trauma is a wound or injury caused by sudden external force or violence. • Major trauma can result in shock, respiratory failure, and death. • Motor vehicle accidents are the most common cause of injury-related death. • Gunshot wounds are the 3rd leading cause. Amputation: Partial or complete loss of body part due to an injury or accident. Treatment of Amputation Stop the bleeding and salvage the amputated part. 1. Apply direct pressure to the site of bleeding. 2. Treat for shock. 3. Wrap amputated part in dry sterile gauze and put in plastic bag. 4. Put plastic bag into second bag filled with ice. Do not let ice come in contact with amputated part or immerse in water. Impaled Object: Remains embedded in the skin. Treatment of Impaled Object Stop the bleeding, and stabilize the object in place. 1. Leave the object in place. Removal may cause severe bleeding. 2. Call 9-1-1. 3. Expose the wound. 4. Apply direct pressure at wound edges to control bleeding. 5. Stabilize the object in place. a. Use bulky dressings or clean cloths and tape. b. Secure at least ¾ of the object in place. c. If impaled in an extremity and EMS is delayed, apply a splint. 6. Calm and reassure the victim. Do not apply pressure directly on the object. Do not remove an impaled object. Do not shorten an impaled object. Basic First Aid Lecture Guide Bleeding, Shock and Trauma 29 Remove a foreign object impaled in the cheek. • Massive bleeding can obstruct the airway. • If there is difficulty removing the object, leave it in place. • Pack the cheek with sterile gauze (between the teeth & cheek). • Position the person so that blood will drain out of the mouth. Gunshot Wound (GSW) There are approximately 200 million privately owned firearms in the U.S. • Causes laceration, crushing and shock wave-type injuries. • Causes damage to bones, vital organs and major blood vessels. • May have exit wounds that are larger than entrance wounds. • Can ricochet off bones and cause additional injuries. Treatment of Gunshot Wound Ensure scene safety before responding. 1. Call 9-1-1 for EMS and law enforcement. 2. Severe Bleeding Treatment protocol a. Check for entrance and exit wound. b. Control bleeding. 3. Spinal immobilization if potential spine injury. 4. Do not disturb potential crime scene evidence. c. Treat for shock. d. Keep the victim still. Crush Injuries: Occur from blunt force applied for an extended period. • Tissues are not being supplied with blood while under compression. • Common injuries: fractures, lacerations, bruising, bleeding • Injury scenes can be dangerous; consider secondary collapse. Treatment of Crush Injuries 1. Scene safety 3. Severe Bleeding Treatment protocol. 2. Call 9-1-1 for serious injury. 4. Spinal immobilization Minor Wound Care 1. Universal Precautions • Wash hands or use hand sanitizer • Put on gloves 2. Stop the bleeding with direct pressure. • May take less than 5 minutes. 3. Rinse thoroughly with clean water. 30 Bleeding, Shock and Trauma © 2011 EMS Safety Services, Inc. 4. Apply triple antibiotic ointment to a superficial wound. • Ensure no history of allergy to the antibiotic. 5. Cover with a dressing. 6. Watch for signs of infection or allergy to tape or ointment. Tip Don’t clean a wound with a cotton ball or anything fluffy that may leave deposits. Senior A skin tear is a tearing away of the skin from the tissue below. • Common in older persons with drier, thinner, and less elastic skin. • Result of a bump, fall, or even vigorous washing and drying of skin. • Common on hands, arms and lower legs. • Treat as an avulsion: replace torn skin if possible. Risk factors for skin tears: impaired vision, limited mobility, malnutrition, use of corticosteroids, dementia, loss of pain perception. Nosebleeds • Very common, but rarely life threatening. • Usually caused by dryness. Treatment of Nosebleeds 1. Sit in a chair and tilt the head slightly forward. 2. Pinch the nostrils for about 10 minutes. 3. Apply ice pack wrapped in a moist cloth to nose. Breathe through the mouth. Get medical help if: • The nose bleeds for more than 20 minutes. • The victim has difficulty breathing. • The bleeding is very fast or heavy. • The victim feels dizzy or weak. • It occurs after an injury to the head. o May indicate a skull fracture or broken nose. • The nosebleed is associated with hypertension. Do not tilt the nose up in the air. Do not put head between the knees. Basic First Aid Lecture Guide Bleeding, Shock and Trauma 31 DEMONSTRATE: Bleeding control and bandaging PRACTICE: Bleeding control and bandaging Instructor Note: Skill Sheet 4 - FA Assessment, Bleeding 1. Separate students into pairs: 1 ‘victim’ and 1 ‘responder.’ 2. Have responder control bleeding, then bandage arm wound. 3. Have students switch roles and repeat. Blisters (optional topic) A blister is an area of raised skin filled with a watery liquid. • Usually the result of friction, 2nd degree burn or a skin rash. • Do not pop the blister. • Keep clean and dry, cover with a bandage, and avoid pressure on it. • If blister pops, follow Minor Wound Treatment protocol. • Consult physician if signs of infection or large blistered area. Splinters (optional topic) Splinter Removal: 1. Wash your hands and clean the area thoroughly with soap and water. 2. If the splinter sticks out from the skin: a. Use clean tweezers to grab the splinter and carefully pull it out at the same angle that it went in. b. If the splinter is small and you can’t grab the splinter with tweezers, apply a piece of sticky tape over the splinter and pull off the tape to remove the splinter. 3. If the splinter is hard to grab or under the skin: a. Sterilize a sharp needle with rubbing alcohol or by placing the tip in a flame. b. Use the needle to carefully remove skin over the splinter and lift the tip of the splinter out. Grab the splinter with tweezers. 4. Follow Minor Wound Treatment protocol. 5. Apply a bandage if the wound may get dirty. Get medical help if: • Close to your eye • Signs of infection • Deeply embedded 32 Bleeding, Shock and Trauma © 2011 EMS Safety Services, Inc. How Would You REACT? QUESTIONS SCENARIOS Home 1 If the victim is responsive, you should ask questions to find out what is wrong. 2 True False You are climbing down a ladder and you catch your foot and fall. You have a two inch laceration to your right forearm, and no other pain. It is bleeding steadily. How would you REACT? Which of the following best describes the shock position? a. b. c. d. Person lying down, face up Person lying on their left side Person lying on their right side Person sitting in the position of comfort Community You have just parked your car at the grocery store when you see a man lying down motionless next to a car. How would you REACT? 3 A rescuer who finds an unresponsive but breathing victim sitting in a car should remove the person quickly, and then call for help. 4 True Treat an avulsion by putting the torn skin back in place, then bandaging the wound as a laceration. True School False You are monitoring the parents as they drop their children off at school in the morning. You see a child exit a bus and get hit by a car. The child is sitting up holding her knee and crying. Her leg appears deformed. How would you REACT? False Work 5 The proper treatment position for a nosebleed is to have the person sit in a chair and: a. b. c. d. Tilt the head slightly forward Put the head between the knees Tilt the head all the way back None of the above Basic First Aid Lecture Guide You walk into the warehouse and see a coworker lying at the bottom of the rolling stairs. How would you REACT? How Would You REACT? 33 Head, Neck & Back Injuries DVD Ch: 13 DEMONSTRATE: Penetrating trauma to the eye (optional) PRACTICE: SUPPLIES: Paper cup, bulky dressing, gauze roll or kerlix Learning Objectives • Describe the signs, symptoms, and treatment of head injury. • Understand that protective gear and seat belts can prevent head injuries. • Identify the causes, signs and symptoms of neck and spine injuries. • Describe treatment of neck and spine injuries. • Identify the common causes, signs and symptoms of eye injuries. • Describe the treatments for penetrating trauma & chemicals in the eye. • Understand the proper treatment when a tooth is knocked out. • Know when an emergency visit to the dentist is necessary. Head Injuries Key Concepts • With any head injury, assume the person also has a neck injury. o Stabilize the head and neck as a unit to prevent further injury. • Treat the victim in the position found. • All head injuries should be evaluated by a physician. Overview Inside the skull, the brain is surrounded by cerebrospinal fluid (CSF). • Cushions the brain from bumps of everyday activities. • The fluid may not be able to absorb a hard blow. • An external object can also damage the brain (penetrating head injury). • 1.7 million traumatic brain injuries each year; 52,000 die. Common Causes: • Car, motorcycle, bicycle accidents • Fall from a height greater than standing • Physical assault • Electrical shock or lightning strike • Sports activities: diving, contact sports 34 Head, Neck & Back Injuries © 2011 EMS Safety Services, Inc. External Head Injuries Most blows to the head result in external injuries. • Scalp lacerations bleed profusely. • A hematoma is a large swelling on the scalp after a blow. o The scalp’s veins leak blood into the tissue just beneath the skin. o Will last for several days or even weeks. • A black eye is the result of bleeding around the eye and under the skin. o Most are not serious. o Avoid any pressure on the eye itself. o If there is bleeding within the eye, seek emergency medical care. • Trauma to the nose is usually caused by blunt injury. • Consider a facial fracture if facial irregularity. Treatment of Minor Scalp Wounds No signs of head or neck injury 1. Control bleeding. 2. Provide wound care as needed. 3. Apply an ice pack wrapped in a moist cloth. 4. Monitor for changes in status or symptoms. 5. If possible fracture or brain injury, activate EMS. Internal Head Injuries (Traumatic Brain Injury, or TBI) Any head injury that causes unresponsiveness indicates at least a concussion. • A concussion is a bruise to the brain. o Caused by a violent jolt or blow. o Usually not life threatening. o May include a loss of consciousness. o The person may repeat a question over and over again. o Possible bleeding in or around the brain. • Watch closely for signs and symptoms of further brain injury. o A physician should evaluate a patient with a significant head injury. o If person displays signs or symptoms of brain injury, activate EMS. Parents and sports coaches should be familiar with the signs of a concussion. • A person who has had a prior concussion has an increased risk of serious brain injury and even death in subsequent brain injuries. • Coaches must know when to remove players from a game or practice. • Parents must be alert to signs of head injury. Basic First Aid Lecture Guide Head, Neck & Back Injuries 35 Signs and Symptoms of Head Injury • Head trauma • Headache, neck pain or stiffness • Confusion, amnesia, repetitive questions • Change in behavior, mood or sleeping pattern • Bleeding or fluid from the nose, ears, eyes, mouth • Seizures • Unresponsiveness, drowsiness, fatigue, dizziness • Abnormal breathing • Slurred speech • Loss of bowel or bladder control • Nausea and repeated vomiting • Difficulty swallowing • Difficulty with movement, sensation or balance • Ringing in the ears • Blurred vision; unequal pupils • Bruising behind the ears • Raccoon’s eyes Treatment of Head Injury 1. Call 9-1-1 (activate EMS). 6. Report to EMS personnel: 2. Stabilize head and neck together in the position found. a. The mechanism of injury 3. Treat the conditions found (e.g. control bleeding, treat for shock). c. Initial and follow-up assessments 4. Calm and reassure. 5. Monitor for changes in response, breathing, appearance, and mental status. b. How long a victim was unresponsive d. Victim’s prior and current mental status e. Any past history of head injuries Do not move the victim unless it is absolutely necessary. Do not remove a penetrating object. Do not leave the victim alone. Senior Falls are the leading cause of traumatic brain injury (TBI). • People > 75 have the highest rate of injury and death from TBI. • Reduce risk for falls. • Recognize TBI after a fall. • Get medical help. Child Shaken Baby Syndrome • When an infant or toddler is shaken, the brain bounces back and forth inside the skull. • Causes brain bruising, swelling, and possible brain damage or death. • Usually younger than 2 years old. • Can occur with as little as 5 seconds of shaking. 36 Head, Neck & Back Injuries © 2011 EMS Safety Services, Inc. DISCUSS: How can you protect yourself and your family from head injury? • Make sure your helmet fits properly. • Know the signs and symptoms of concussion. • Always wear a seatbelt; place infants and small children in child car seats. • Keep firearms unloaded and locked away securely. • Install child safety gates at the top and bottom of stairs. • Use non-slip mats in tubs and showers. • Install window guards to prevent falling out of windows. • Wear a hard hat at work when indicated. Sum it up • Early response to a head injury could save a life. • If a person has signs and symptoms of a brain injury, call 9-1-1. Neck and Spine Injuries Key Concepts • If a victim has a head injury, assume there is also a neck injury. • If there is a chance of spinal injury, assume there is one. • Even with a spinal fracture, the spinal cord may still be intact. • Improper care of the victim can result in permanent paralysis or even death. The spinal cord is a group of nerve tracts extending along the back. • Originates in the brain and ends in spinal nerves that go to the various parts of the body. • Protected by the spine, a series of bones that extends from the base of the skull to the tailbone. • All the information going from the brain to the limbs and back travels through the spinal cord. When the spinal cord is damaged it can result in: • Loss of movement, sensation, breathing and bladder control • Immediate death 12,000-20,000 spinal cord injuries each year in the US; up to 50% will die. • Males sustain 80% of SCI. • >50% of SCI victims are between 15 to 35 years old. High-risk Incidents: • Motor vehicle accidents • Severe blunt trauma • Penetration injuries • Diving and sports injuries • Head injuries, falls • Lightning strikes • The victim is unresponsive for an unknown reason Basic First Aid Lecture Guide Head, Neck & Back Injuries 37 Signs and Symptoms of Neck / Spine Injury • Head, neck or back injury or pain • Weakness or paralysis in extremities • Unresponsive trauma victim • Loss of bowel or bladder control • Numbness or tingling in extremities • Difficulty breathing Treatment of Neck / Spine Injury 1. Call 9-1-1 (activate EMS). 5. Monitor for changes. 2. Use your hands to stabilize the head & neck in the position found. 6. Do not move the victim except for essential care or imminent danger. 3. Treat the medical conditions found. a. Move long axis (drag, pull). 4. Calm and reassure the victim. b. Maintain neck immobilization. Sum it up • The initial care of a spinal injury may affect the rest of the person’s life. • If there is a chance of spinal injury, assume there is one. Eye Emergencies Key Concepts • When treating an eye injury, do not apply pressure to the eye. • Most eye injuries are preventable. Overview • 1 million new eye injuries each year; 43% occur in the home. • The leading causes include: o Household chemicals o Yard and workshop debris o Sports accidents o Fireworks o Battery acid o Over-exposure to UV radiation o Inappropriate games and toys with inadequate supervision • About 40,000 sports-related eye injuries each year; 90% are preventable. • > 700,000 work-related eye injuries each year in the U.S. o 90% are preventable with proper safety eyewear. Debris in the Eye Small, loose foreign bodies in the eye will usually be removed by tears. • Blink several times. 38 Head, Neck & Back Injuries © 2011 EMS Safety Services, Inc. • Gently flush the area with lukewarm water. • If flushing does not help: o Lay a swab across the top of the eyelid. o Fold the lid over the swab and flush with lukewarm water, or use wet sterile gauze. Do not try to remove something directly over the cornea. • If you are unable to remove it, seek medical care. • Do not rub the eye. • Do not apply ointments or creams. Chemical in the Eye Chemicals must be immediately flushed from the eye. • Tilt the head down toward the affected eye. • Apply a gentle stream of water to the bridge of the nose for at least 20 minutes. • Keep the affected eye lower than the unaffected eye. • Remove contact lenses. • Ensure that run-off does not come into contact with rescuers. • Contact your local poison control center for specific instructions. • Seek medical care immediately. • Take the label or chemical container with you. Blow to the Eye • Apply an ice pack wrapped in a moist cloth to reduce pain and swelling. • Do not apply pressure to the eye. • If the victim develops a black eye, pain, or changes in vision, see a physician. • A black eye can be a sign of significant eye or head injury. Corneal Abrasions • A corneal abrasion is a scratch on the surface of your eye. • It can be caused by dust, dirt, a fingernail, or even a contact lens. • Often described as a continual feeling that something is in the eye. • Usually very painful. • You may notice redness, tears, blurred vision, or sensitivity to light. • Must be evaluated by a physician and may require antibiotics. Penetrating Trauma to the Eye DEMONSTRATE: Penetrating Trauma to the Eye (optional) Basic First Aid Lecture Guide Head, Neck & Back Injuries 39 Treatment of Penetrating Trauma to the Eye Stabilize the object; do not remove it. 1. Send a bystander to call 9-1-1 (activate EMS). 5. Use a cup, bulky dressing and gauze roll to stabilize the object in place. 2. Calm and reassure. 6. Keep all pressure off the eye. 3. Control bleeding as necessary. 7. Do not attempt to wash the eye. 4. Cover the uninjured eye. Sum it up • Eye injuries are the most common preventable cause of blindness. • Wear protective eyewear when needed in the home, garden, work, and during sports. DISCUSS: Eye Injury Prevention (optional topic) In the Workplace: • Identify operations and areas that present eye hazards. • Offer vision testing to your employees. • Provide protective eyewear that fits properly and is comfortable. • Establish an eye protection program with mandatory annual training. • Ensure access to eyewash stations. At Home: • Cut infant’s and children’s fingernails short. • Trim low-hanging tree branches. • Pad or cushion sharp edges or corners of furniture and fixtures. • Use seat belts and child car seats when driving. • Avoid toys that fly, fire projectiles or have sharp points or edges. • Keep chemicals and household products locked up. • Use guards on power equipment. • Regular eyeglasses do not provide adequate protection. • Wear safety goggles to protect against flying particles or chemicals. During Sports: • Wear a helmet, goggles or face shield when there is a chance of eye injury. Dental Emergencies Key Concepts • 5 million teeth are knocked out each year. • If a tooth is knocked out or broken, be careful not to inhale or swallow the tooth or blood. Knocked-out Adult Tooth • If a tooth is reinserted quickly, it is usually retained permanently. • See a dentist within 30 minutes for the best chance of saving the tooth. 40 • Primary teeth are never reinserted. Head, Neck & Back Injuries © 2011 EMS Safety Services, Inc. Treatment of Knocked-Out Tooth 1. Handle the tooth by the crown, not the root (base). 2. Rinse the tooth gently if dirty. Cleaning the root could reduce the chance of successful reimplantation. 3. Place the tooth in a container of cool milk. 4. Bite down on a sterile gauze pad or clean cloth to control bleeding. 5. Apply an ice pack wrapped in a moist cloth to the face. 6. See a dentist within 30 minutes to reinsert the tooth. 7. Remain alert for signs of airway compromise. Tip If a tooth is lost, have a chest x-ray to see if the tooth was inhaled or swallowed. Broken or Loose Tooth • Gently bite down on gauze to hold it in place. • Contact your dentist immediately. • Avoid drinking or eating. Bleeding from the Mouth • Causes: bitten lip, tongue, cheek • Control bleeding: o Apply direct pressure. o Apply an ice pack wrapped in a moist cloth. o If unable to stop the bleeding after 15 minutes, call 9-1-1 or go to a hospital emergency department. • Observe for signs of airway obstruction. o In the unresponsive victim, blood from a mouth injury can obstruct the airway. o Position the victim to allow blood to drain out of the mouth. Jaw Injury A jaw fracture is suspected if there is: • Pain • Swelling • Limited opening of the mouth • A new malocclusion (poor bite) • Double vision • Facial numbness To reduce pain: • Close the mouth and splint the jaw with a gauze roll (or a towel, shirt or necktie). • Do not interfere with the airway or over-tighten. Basic First Aid Lecture Guide Head, Neck & Back Injuries 41 • Remain alert for airway complications. • Apply an ice pack wrapped in a moist cloth. • Seek professional medical attention promptly. If there is airway obstruction or uncontrollable bleeding, activate EMS. Sum it up • Most dental trauma is preventable: o Use mouth guards or face shields. o Wear a seat belt. o Don’t chew on ice or hard candy. • See a dentist within 30 minutes if a permanent tooth is knocked out. • If airway obstruction, activate EMS. Chest and Abdominal Emergencies DVD Ch: DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Know how to recognize and treat chest and abdominal wounds. • Understand that any pregnancy-related illness, complication or injury should be evaluated by a physician. Broken Ribs • A rib fracture is painful but rarely life-threatening. • Complications: o Sharp bone ends can cause a punctured lung or lacerated liver. o Observe for internal bleeding or respiratory distress. Flail Chest occurs: • When 2 or more ribs are broken in at least 2 places. • Produces a free-floating segment. • Ribs no longer assist with breathing. • Can damage the lung beneath it by bruising or puncturing it. Signs and Symptoms of Flail Chest • Bruising • Deformity • Pain with a deep breath • Paradoxical movement • Tenderness when palpating the injured area o The flail segment moves in the opposite direction of the rest of the chest. • Swelling 42 Chest and Abdominal Emergencies © 2011 EMS Safety Services, Inc. Treatment of Flail Chest 1. Call 9-1-1 (activate EMS). 3. Treat for shock. 2. Consider neck damage. Sucking Chest Wound • Trauma has punctured the chest wall. • Air rushes into the chest cavity, collapsing the lungs. • Life-threatening condition. Signs and Symptoms of Sucking Chest Wound • A sucking sound is heard with each breath. • Sharp chest pain • Difficulty breathing • Anxiety • Bluish skin color Treatment of Sucking Chest Wound 1. Call 9-1-1 (activate EMS). 2. Calm and reassure; keep the person still. 3. Apply an airtight dressing (foil or plastic wrap) to keep air from entering during inhalation. o Leave one side untaped to let air escape when exhaling. 4. Monitor condition. 5. If breathing worsens, remove 3-sided dressing. Abdominal Wounds Open abdominal wound: • Usually caused by a penetrating injury. • May expose internal organs. • Do not remove objects impaled in the abdomen. • Do not attempt to push abdominal organs back in. Closed abdominal injury: • Usually caused by blunt trauma injury. • Consider spine immobilization. • Watch for signs of internal bleeding. Common Causes: • Automobile accidents • Knife or gunshot wounds • Medical problems related to the stomach and intestines Basic First Aid Lecture Guide Chest and Abdominal Emergencies 43 Signs and Symptoms of Abdominal Wound • Weak, rapid pulse • Vomit that is bright red or looks like coffee grounds • Pale, cool, moist skin • Dark tarry or bright red stool • Abdominal pain, tenderness or rigidity • Back pain (kidney damage) • Nausea or vomiting Treatment of Abdominal Wound 1. Call 9-1-1 (activate EMS). 2. Position on back with knees bent, if does not increase pain. 3. Stabilize foreign object; do not remove. 4. Cover exposed organs loosely with a moist, sterile dressing, and plastic wrap. 5. Do not give food or drink. This may delay necessary surgery. Pregnancy-Related Emergencies • Treatment of pregnancy-related emergencies is extremely complex. • Position pregnant victims on their left side. • Activate EMS at any sign of sudden illness or injury. Appendicitis (optional topic) • The appendix is a small, finger-like pouch attached to the intestines. • When blocked, it becomes infected and requires surgery to remove. • 7% of Americans develop appendicitis. • Most common between the ages of 10-30. • If not detected early, may rupture within 2-3 days and spread infection throughout the abdomen. • Appendicitis can be life threatening and is a medical emergency. Signs and Symptoms of Appendicitis • Pain in the lower right abdomen; pain with palpation of area. • Loss of appetite • Nausea and vomiting • Distended (swollen) abdomen, constipation • Low-grade fever Treatment of Appendicitis 1. If you suspect appendicitis, contact your doctor immediately. 2. If you have symptoms of peritonitis, it’s a medical emergency; activate EMS. Sum it up • A sucking chest wound is a life-threatening situation. • Do not remove objects impaled in the abdomen. 44 Chest and Abdominal Emergencies © 2011 EMS Safety Services, Inc. Muscle, Bone and Joint Injuries DVD Ch: 14 DEMONSTRATE: Splint application Sling / swathe (optional) PRACTICE: Splint, sling, swathe (optional) SUPPLIES: Splint, binding or wrap Triangular bandages Learning Objectives • Define fracture, dislocation, sprain and strain. • Describe assessment and treatment of muscle, bone & joint injuries. • Demonstrate splint and sling application (optional). • State the meaning of the acronym RICE. Key Concepts • The human body is made up of more than 600 muscles and 200 bones. • Types of musculoskeletal injury: fractures, dislocations, sprains, strains and contusions • A First Aid provider treats fractures, dislocations, severe sprains and strains the same. Fractures and Dislocations A fracture is a break in a bone. • An open fracture has bleeding and penetration of the skin by the bone. • A closed fracture leaves the skin intact. A dislocation is a separation or displacement of joint surfaces. • Usually caused by a hard blow. • Treat a dislocation the same as a fracture. Signs and Symptoms of Fracture • Pain and tenderness • Numb, cold to touch • Bruising, swelling at injury site • Crepitus (crackling sound with movement) • Deformity, angulation, bump, shortening • A “snap” or “pop” heard at the time of injury • Bleeding, exposed bone ends (open fracture) • Inability to move the injured part ! Compare the injured side to the uninjured side to determine deformity and swelling. Basic First Aid Lecture Guide Muscle, Bone and Joint Injuries 45 Treatment of Fracture 1. Call 9-1-1 (activate EMS). 2. Keep the person calm and still. 3. Observe for signs of shock. 4. Cover open wounds with a sterile dressing. Control bleeding with gentle pressure. 5. Apply an ice pack wrapped in a moist cloth for 15-20 minutes. 6. Watch for signs of shock or internal bleeding. 7. Monitor temperature and sensation beyond the injury. 8. Only splint the injury if EMS is delayed or if you must transport the victim yourself for a minor injury or from a remote location. Do not try to move a victim unless it is absolutely necessary. Do not try to realign a broken bone. Do not give food or drink. Do not straighten or manipulate the fracture site. Splint in the position found. Child • Children fall frequently, but most falls do not result in a fracture. • A child’s bones are softer than an adult’s bones. • Fractures in children usually heal faster than fractures in adults. • The fracture of a growth plate (area at the end of a long bone where new bone tissue grows) may require physician follow-up to make sure there are no complications when it heals. Applying a Splint Apply splints to suspected fractures, dislocations and severe sprains. • To immobilize the joints above and below the injury. • Should not increase pain. • Allows transport with less pain and risk of further injury. • Made from rigid materials or “buddy taped” to another body part. • Usually wait for EMS personnel to splint the injury. DEMONSTRATE: Applying a splint Splinting Procedure: 1. Explain the procedure to the person. 2. Remove jewelry or other items that may be affected by swelling. 3. Check temperature and sensation below the injury site. 4. Control bleeding: cut away clothing, cover open wounds with sterile dressings. 5. Select a splint that is longer than the bone it will support. 6. Pad the splint if needed. Measure it against the uninjured side. 46 Muscle, Bone and Joint Injuries © 2011 EMS Safety Services, Inc. 7. Carefully apply the splint. Secure the splint above and below the injury, not directly over it. 8. Recheck temperature and sensation below the injury site. DEMONSTRATE: Creating a sling and swathe (optional) Creating a Sling and Swathe: A sling supports and positions the limb. Place the injured arm into a triangular bandage or other large piece of cloth. 1. Wrap one end of the sling behind and the other in front of the injured arm. 2. Tie the ends together behind the neck. 3. Position the arm at a right angle so it does not slip. 4. Create a swathe with an additional triangular bandage or other long cloth. Types of Splint • Flexible splint: SAM splint • Improvised splint: stick, magazine, blanket • Anatomic splint: splint one body part to another R.I.C.E. Technique Sprains, Strains and Contusions • A contusion is bruising resulting from a direct blow. • A sprain is a stretching or tearing of ligaments or other structures in a joint. • A strain is a stretching or tearing of muscle or tendon. • Common injury sites include the shoulder, elbow, finger, hip and ankle. • Mild sprains and strains will usually heal within 2 weeks. • If a sprain remains swollen and painful for several days, consult a physician. Rest: Stop activity. Do not put weight on the injured part. Ice: Apply an ice pack wrapped in a thin moist cloth for 20 minutes, 3-4 times a day for the first 2-3 days. Compress: Wrap an elastic bandage around the injury to control swelling. • Wrap in an upward spiral, overlapping with each turn. • Apply the bandage snugly, but not so tightly that it cuts off circulation and causes the person to lose sensation beyond the injury. • Check for sensation, warmth and color before and after applying the compression bandage. This way you can tell if any numbness or tingling is due to the injury or the bandaging. Elevate: Raise the injured area above the heart, if it does not increase the pain. Basic First Aid Lecture Guide Muscle, Bone and Joint Injuries 47 Do not apply ice directly onto bare skin. Tip ! To treat a severe ankle sprain, place a horseshoe-shaped soft pad with the opening facing up on the outer ankle before applying a compression wrap. This will prevent swelling in the outer ankle. Do not apply heat to a new injury because it will increase swelling and bruising. People with decreased sensation, diabetes or vascular disease should consult their doctor before applying ice. Muscle Cramps • The muscle is locked into an involuntary contraction or spasm. • Cause is unknown but may involve muscle fatigue, overexertion, dehydration, exercising in extreme heat, pregnancy, or inadequate stretching. Treatment of Muscle Cramps 1. Stop the activity, gently stretch and ice the muscle. 2. If cramps persist, consult your physician to determine a medical cause. Sum it up • Immobilize a suspected fracture, and wait for EMS personnel to splint it. • Use RICE to reduce pain and swelling. OPTIONAL PRACTICE: Splint Application OPTIONAL PRACTICE: Sling and Swathe Application Senior Falls and Fractures Key Concepts • Falls are serious for anyone, but can be especially serious for older persons. • More than 1 in 3 people over age 65 fall every year. o Up to 5% of these falls result in fractures. • Over 2 million people are treated in emergency departments each year for fall-related injuries. Common Fractures in Seniors Hip fracture • The most common fracture after age 75. • 80% occur in older women. 48 Muscle, Bone and Joint Injuries © 2011 EMS Safety Services, Inc. Signs and Symptoms of Hip Fracture • The leg may be turned outward in an unnatural position. • Unable to move the leg. • Severe sudden pain. • Usually associated with a fall, but may be spontaneous (no apparent cause) Treatment of Hip Fracture 1. Call 9-1-1 (activate EMS). 2. Keep the person calm and still. Do not move the person. May be confused with a hip dislocation, which can occur after hip replacement surgery. • The leg may be turned inward or outward in an unnatural position. • Treat a suspected dislocation and fracture the same. Pelvic fracture • There may be no visible deformity, but extreme pain when trying to roll, walk, or even move the legs. • Call 9-1-1 (activate EMS). Compression fracture of the spine • The collapse of one 1 or more vertebral bones can occur with no apparent cause. o It can be very painful or may have no symptoms at all. o Get medical care for evaluation, pain management, and osteoporosis treatment. • If unable to move or walk or if pain is severe, call 9-1-1. • If the vertebral fracture is caused by an injury such as a fall: o Call 9-1-1 (activate EMS). o Keep the person calm and still. o Do not move the person. Osteoporosis • A disease that causes a gradual loss of bone density. • Results in extremely fragile bones that break under minimal stress. • Women lose bone density faster than men. • 50% of all women and 25% of all men over age 50 will sustain a fracture due to osteoporosis. Prevent osteoporosis to prevent fractures. • See a healthcare provider to: o Evaluate you for osteoporosis. o Clear you to perform weight bearing activities and exercises to strengthen your bones. Basic First Aid Lecture Guide Muscle, Bone and Joint Injuries 49 o Evaluate your medications to see if they contribute to osteoporosis or falls. o Evaluate your nutritional status. • Take care of yourself. o Stop smoking. o Avoid excessive alcohol consumption. o Eat a healthy and adequate diet. Sum it up • A fall can be serious and affect the rest of your life. o Many people develop a fear of falling and become less active. o Less activity leads to osteoporosis and loss of strength and mobility. o Osteoporosis can lead to increased risk of fracture during a fall. o Decreased strength and mobility leads to higher risk for falls. o A fall can result in a loss of function or independence, and produce a fear of falling. • Follow the fall prevention tips at the end of the workbook to prevent falls. • See a healthcare provider to evaluate you for osteoporosis. • See a physical therapist to improve your strength and mobility. Burns DVD Ch: 15 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Identify the types and severity of burns. • Describe the assessment and emergency treatment of burns. Key Concepts • Cool thermal burns with water. o Helps stop the spread of a burn. • About 4,500 fire and burn deaths per year. • About 20,000 more are injured from fire and burns. • Smoke alarms decrease your risk of dying in a fire by 50%. Thermal Burns • Ensure scene safety. • Stop the heat source. • Death often results from smoke rather than heat or flames. • Hypothermia may occur in large burns due to decreased ability to retain heat. o Prevent further heat loss by covering the victim with a clean white sheet. 50 Burns © 2011 EMS Safety Services, Inc. Treatment of Minor Burns 1st degree or small 2nd degree 1. Rinse with cool water for at least 20 minutes or until pain is relieved. Stop the cooling process if the person shivers. 2. 2nd degree burn: apply antibiotic ointment and cover with dry, sterile, non-stick dressing. Treatment of Severe Burns 1. If clothes are on fire: a. Stop, Drop and Roll. b. If you stand up, the fire will burn your airway. 2. Remove from environment if smoke and heat. 3. Call 9-1-1 (activate EMS). 4. Remove any clothing or jewelry that does not stick to the burned skin. 5. Cover with a dry, sterile bandage or cloth. 6. Elevate the burn to decrease swelling. 7. Monitor response, breathing, and signs of shock. a. Look for singed hairs or soot around the mouth or nose. b. This could indicate a respiratory tract burn, which may lead to swelling that closes the airway. • Do not apply butter, ointment or creams to a severe burn. • Do not try to remove jewelry and clothing that has been burned into the skin. • Do not apply ice directly onto the skin. • Do not break blisters. Senior • Seniors are more at risk for burns due to: o More difficulty differentiating between hot and cold o Decreased pain perception • The young and the elderly have the most difficulty recovering from severe burns. • Unexplained or suspicious burns could be an indication of abuse. Child • The young and the elderly have the most difficulty recovering from severe burns. • Unexplained or suspicious burns could be an indication of abuse. Basic First Aid Lecture Guide Burns 51 Chemical Burns Treatment of Chemical Burns 1. Call 9-1-1 (activate EMS). 2. Brush a dry chemical off the skin with a gloved hand. 3. Remove contaminated clothing and jewelry. 4. Rinse the burn with cool water for at least 20 minutes. Ensure run-off water does not flow over unaffected skin or onto the rescuer. 5. If the chemical burn is in the eye, begin flushing the eye with water immediately and do not stop until EMS takes over. a. Use a gloved hand to help hold the eye open if needed. 6. Contact the poison control center for expert information or if you are not sure if the chemical is toxic. 7. Follow the first aid directions on the label or locate the Material Safety Data Sheet (MSDS). ! A chemical can also be inhaled, potentially damaging the lungs. Electrical Burns 1. Scene safety: turn off the power supply. 2. Call 9-1-1 (activate EMS). 3. Provide CPR or treat for shock if needed. 4. Look for entrance and exit wounds, and treat thermal burns. All victims of electrical burns need to be evaluated by a physician! DISCUSS: Fire Safety Tips (optional topic) • Escape first, then call for help. Close all the doors that you can between yourself and the fire. Use rags to seal the door. • Know two ways to escape from every room. • Practice escape routes. • Establish a meeting place at a safe distance outside the building. • Do not open doors that are hot to the touch. • When escaping, never stand up: crawl low, and keep your mouth covered with a moist cloth. The air is cleanest low to the ground. • Place smoke alarms in each room; change the batteries annually. • Respond to every alarm as if it were a real emergency. • Never use an elevator during a fire. • Never re-enter a burning building to search for missing people or pets. Always wait for firefighters. • Equip security bars or windows with a quick-release. 52 Burns © 2011 EMS Safety Services, Inc. Sum it up • If there is a fire, escape first, then call for help. • Stop the spread of a burn, then check for shock and breathing problems. • Activate EMS for a large or critical burn. DISCUSS: Smoke detectors and fire extinguishers 1. How many students have smoke detectors at home? 2. How many students change the batteries annually? 3. How many students have a fire extinguisher in their kitchen? In their garage? Basic First Aid Lecture Guide Burns 53 How Would You REACT? QUESTIONS SCENARIOS Home 1 When helping a victim who has a possible head injury, the rescuer should also consider a neck injury. 2 There is immediate danger The victim needs CPR The airway is blocked All of the above Community You are walking out of a restaurant when you see an older person trip on a parking space barrier and fall. He is lying on the ground with his leg turned outward in an unnatural position. How would you REACT? A victim with a knocked-out tooth should reinsert it back into the socket himself. 4 False The only time to move a victim with a suspected neck or spinal injury is when: a. b. c. d. 3 True Your brother is painting the house when he falls off a ladder. He complains of severe neck pain and tries to stand up. How would you REACT? True School False Apply heat to a newly-sprained ankle to reduce pain and swelling. True During recess a child is running, trips and falls. When he stands up and walks back across the playground, he says his ankle hurts. How would you REACT? False Work 5 The signs and symptoms of a fracture may include: a. b. c. d. e. 54 Pain Bruising Deformity Swelling All of the above A maintenance worker is repairing a light switch when there is a jolt of electricity and he falls to the floor. How would you REACT? How Would You REACT? © 2011 EMS Safety Services, Inc. Respiratory Emergencies DVD Ch: DEMONSTRATE: 16 PRACTICE: SUPPLIES: Learning Objectives • Recognize the signs and symptoms of a respiratory emergency, and know how to respond. • Describe the appropriate emergency treatment for severe asthma. Key Concepts • Sudden, severe difficulty breathing is a medical emergency. • Recognition of the emergency and prompt activation of EMS is critical. Delay can be fatal. • Approximately 25 million Americans suffer from asthma. • A person with a history of severe asthma attacks may wear medical alert jewelry and carry a quick-relief inhaler. Many causes of breathing difficulty: • Injury • Heart attack • Stroke • Allergic reaction • Choking • Poisoning • Respiratory infection • Asthma • Congestive heart failure • Chronic obstructive pulmonary disease (COPD) Senior COPD is a group of lung diseases, including chronic bronchitis and emphysema, which limit the flow of air into and out of the lungs. • 80% of all cases are caused by heavy, long-term cigarette smoking. • COPD cannot be cured; symptoms can be controlled. o Quit smoking o Exercise o Proper diet o Adequate rest o Stress management Basic First Aid Lecture Guide Respiratory Emergencies 55 Signs and Symptoms of Respiratory Emergency • Breathing rate: Too fast or too slow • Noisy breathing: Wheezing, gurgling, high-pitched sound • Tripod positioning: Upright, rigid posture with arms locked and supporting body weight • Labored breathing: Using shoulder and back muscles to assist breathing • Broken dialogue: Speaking in short sentences, pausing for breath • Color: Ashen, pale, bluish skin, especially lips & fingernail beds • Mental status: Dizzy, confused • Behavior: Anxious, restless, irritable • Chest pain: If SOB is caused by injury, heart attack, collapsed lung, blood clot in lung • Signs of choking: No breathing, 1 or both hands at the throat • Children: Nasal flaring, rib retraction Tip When surveying the scene, quickly look for clues to the cause of the problem: • Partially eaten food • Asthma inhaler present • Poisons present (e.g. opened chemical containers or pill bottles) • Drug paraphernalia • Medications stored in a disorganized way • Oxygen tank • Accident scene When assessing the victim, quickly try to determine the cause of the breathing difficulty: • What happened to cause the problem? • Is there a history of severe allergy or asthma? • Are there other symptoms of heart attack or stroke? Treatment of Respiratory Emergency 1. Activate EMS (call 9-1-1). 3. Keep the person calm and still. 2. Position of comfort, usually sitting up. Senior Pneumonia • A respiratory condition that destroys lung tissue & causes fluid build-up around the lungs • Reduces the lungs’ ability to get oxygen, so a person breathes faster to compensate. • Very serious illness for older adults or people with chronic illness • > 52,000 people die of pneumonia each year in the U.S. • If you suspect pneumonia, see your doctor right away. • Pneumonia is preventable with vaccination. 56 Respiratory Emergencies © 2011 EMS Safety Services, Inc. Child Whooping Cough (pertussis) • A respiratory infection that produces prolonged coughing attacks. o End coughing attack with a high-pitched ‘whoop’ sound o Persistent, hacking cough • Contagious before major signs and symptoms are present. • If you suspect whooping cough, see your doctor right away. • Whooping cough is preventable with vaccination o Vaccination is usually required for school attendance. Asthma • A chronic disease in which the main air passages of the lungs become inflamed. • Many asthmatics carry inhaled medication that can quickly open airways. • By treating attacks early, the severity of the attack is usually reduced. • Asthma attacks are usually brought on by triggers: o e.g. Odors, exercise, stress, smoke, pollution, allergens, respiratory infection. • Avoid the triggers of asthma attack (except exercise). • Suspect asthma in a person with a history of asthma attacks. Senior • Some people develop asthma later in life. • Take action to control asthma triggers. • Tell your doctor if you have symptoms of asthma. o Certain medications can provoke asthma. o There are alternatives to most medications that may not cause an asthma attack. • Ask your doctor for an asthma treatment plan. • Keep an updated list of current medications and dosages. • Tell your friends and relatives how to help you in case of an asthma attack. • Get a flu shot each year. o Respiratory infections are a common trigger for asthma. Signs and Symptoms of Asthma Attack • Labored, rapid breathing • Bluish lips and fingers • Wheezing, coughing • Flared nostrils • Shortness of breath, chest tightness • Sweating • Anxiety • History of asthma attacks • Tripod position Basic First Aid Lecture Guide Respiratory Emergencies 57 Treatment of Asthma Attack 1. Position of comfort, usually sitting up. 2. Ask the person if he or she has an inhaler. If the person cannot self-administer the medication, offer to help them use it. 3. Try to determine the attack trigger in order to remove it. 4. Keep the person calm and still. Using a Quick-Relief Inhaler: 1. Locate and assemble the inhaler. 2. Shake it hard a few times. 3. Remove the cover. Attach the spacer if there is one. Call 9-1-1 if: 4. Instruct the person to fully exhale. 5. Place the inhaler in the person’s mouth and press down on the canister as the person inhales slowly and deeply. • Severe asthma attack • No inhaler nearby • No relief from the inhaler 6. Instruct the person to hold his or her breath for 10 seconds. 7. Repeat with a 2nd dose after a few breaths. Make sure the victim is fully alert before assisting with an inhaler. ! Make sure the person is using his or her own prescription quick-action inhaler, and it has not expired. A person with asthma should follow his or her healthcare provider’s instructions for use of an inhaler if they differ from these instructions. In some regions a first aid provider is not allowed to help administer asthma medication. Follow your state, local and workplace regulations for the use of prescribed asthma medications. Child • If you are a caregiver of an asthmatic child, make sure the parents leave the child’s medications with you, along with specific instructions. • Follow your state guidelines for storage and use of medications. Sum it up • If you suspect a respiratory emergency, call 9-1-1 without delay. • Control asthma with medicine and avoiding triggers. 58 Respiratory Emergencies © 2011 EMS Safety Services, Inc. Allergic Reactions DVD Ch: 17 DEMONSTRATE: Epinephrine auto-injector PRACTICE: Epinephrine auto-injector (Skill ) SUPPLIES: Epinephrine auto-injector trainer Skill Sheet 4 Learning Objectives • Identify the signs and symptoms of an allergic reaction. • List 5 common allergens. • Demonstrate the correct use of an epinephrine auto-injector. Key Concepts • An allergy is an overreaction of your body’s immune system to a substance. • 50 million Americans suffer from allergies. • The quicker the onset of symptoms, the more severe the reaction. • Allergic reactions get worse with each exposure. • A person with a severe allergy may wear medical alert jewelry. Common Allergens • Inhaled: Pollen, mold spores, dust, pet dander, smoke, pollution • Swallowed: Shellfish, dairy products, drugs, eggs, nuts, chocolate • Injected: Bee sting venom • Poisons: Can be inhaled, swallowed or injected Signs and Symptoms of Allergic Reactions • Rashes, oozing blisters, hives (red raised lesions with itching and swelling), and itchy skin • Sneezing, nasal congestion, coughing • Asthma (wheezing, shortness of breath) • Swollen face, eyes, throat, tongue • Anaphylactic shock • Gastrointestinal disturbances (from food allergies) Anaphylactic Shock • The most severe result of an allergic reaction. • Causes swelling in the airways and a sudden drop in blood pressure. • It is life threatening and requires immediate emergency medical care. • Death can occur within minutes. • Suspect anaphylaxis when signs and symptoms involve more than one body system (respiratory, cardiovascular, skin, gastrointestinal) Basic First Aid Lecture Guide Allergic Reactions 59 • Food is the leading cause of anaphylaxis in the community. o 30,000 food-induced anaphylactic reactions treated in the emergency department each year in the U.S. o About 200 people die of anaphylaxis each year. Epinephrine • People with known severe allergies may carry an epinephrine auto-injector. • Epinephrine is the most commonly used drug for emergency treatment of anaphylaxis. • The sooner it is administered, the more effective it is in stopping the reaction. Treatment of Severe Allergic Reactions 1. Send a bystander to call 9-1-1 (activate EMS). 2. Calm and reassure the person. 3. If requested, help the person locate and use the epinephrine auto-injector. a. You must be trained to use it. b. Your state, local, and workplace regulations must allow it. 4. If the allergic reaction is from a bee sting, quickly scrape off the stinger with a straightedged object. 5. Monitor response, breathing, and signs of shock. 6. If a 2nd injection is needed, the person should self-administer it. To use an epinephrine auto-injector 1. Carefully remove the safety cap and press the tip firmly against the outside of the thigh, between the hip and knee. 2. Hold for 10 seconds, then pull straight out. 3. Rub the injection site for about 10 seconds. 4. Record the time of the injection. 5. Dispose of the auto-injector safely, or give to EMS when they arrive. ! The person should follow his or her healthcare provider’s instructions for use of an epinephrine auto-injector if they differ from these instructions. Follow your state, local, and workplace guidelines and regulations for use of an epinephrine auto-injector as a first aid treatment. An auto-injector can be used through clothing. • Inject the large muscle of the thigh. • Make sure there is no obstruction, such as keys or clothing side seams. Sum it up • Peanuts, bee sting venom and penicillin often cause a life-threatening reaction in highly allergic people. • Anaphylaxis occurs quickly after contact with the allergen. Act fast. • Never take someone else’s antibiotics due to possible allergic reaction. 60 Allergic Reactions © 2011 EMS Safety Services, Inc. Seizures and Fainting DVD Ch: 18 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Describe the signs, symptoms and treatment for a seizure. • Know the steps to treat a victim who has fainted or feels faint. Key Concepts • A seizure is an abnormal electrical discharge in the brain. • About 10% of the U.S. population will have a seizure during their lifetime. • Almost 3 million Americans have epilepsy, the most common cause of seizure. o Condition in which the person has repeated seizures. o Usually controlled by medication. • If someone tells you he thinks he is going to have a seizure, believe him. Types of Seizure • May affect only one part of the body, or may affect the whole body. • Symptoms displayed will depend on the cause of the seizure and the part of the brain that is affected. o A petite mal seizure can appear as a staring episode (day-dreaming). o A grand mal seizure has more dramatic symptoms, and commonly requires first responder intervention. Child Febrile seizures • Triggered by a rapidly increasing body temperature usually to over 102°. • Most common before age 2, but seen in children up to age 5. • About 3-5% of children between 9 months and 5 years of age have at least one febrile seizure. • Most febrile seizures do not cause any harm. Signs and Symptoms of Seizure • Involuntary movements and rhythmic muscle contractions • Staring, eye movements, drooling • Abnormal sensations, hallucinations • Nausea, sweating, dilated pupils, flushed skin, incontinence • Unresponsive, unaware of surroundings Basic First Aid Lecture Guide Seizures and Fainting 61 Treatment of Seizure 1. Place the victim face up on the floor; remove nearby objects and furniture. 2. Protect the victim’s head from injury with a small pillow or other soft object such as a blanket or jacket. a. Ensure that you do not close the victim’s airway or restrict movement by raising the head too high. 3. Try to loosen any tight clothing, especially around the neck. 4. Ask spectators to leave. 5. Time the seizure. 6. Do not restrain or put anything in the person’s mouth. 7. Do not move the victim unless he or she is in a dangerous location. After the seizure: 8. Assess response, breathing, circulation and appearance. a. May be injured from a fall, bleeding from a bite to tongue or cheek, have inhaled food, fluid or vomit into the lungs, or not getting enough oxygen. b. If not breathing, perform CPR. c. If fluids or vomit in the mouth, place in the recovery position. d. If potential spinal injury, stabilize the head and neck as a unit. e. Cool a febrile seizure victim. Remove clothing, sponge with lukewarm water. Stop cooling if shivering or goose bumps appear. 9. Call 9-1-1 (activate EMS). Continue to monitor the person. • Do not try to awaken the person. • CPR or rescue breathing are rarely needed after a seizure. • Person will be sleepy for one hour or longer. • May not remember the seizure episode. • Do not give food or drink until completely awake and alert. • For a febrile seizure patient, give the normal dose of ibuprofen or acetaminophen when the child is completely awake. • A physician should evaluate all seizure victims. Record details of the seizure: • Date • Length of seizure • Type of symptoms • Which body parts were affected • Behavior after the seizure • Any other pertinent information 62 Seizures and Fainting © 2011 EMS Safety Services, Inc. Fainting Key Concepts • A brief loss of consciousness usually caused by a momentary lack of blood supply to the brain. • Fainting is a common problem. • Can be caused by dehydration, temporary low blood pressure or low blood sugar, or may be related to environmental, emotional or physical stress. Signs and Symptoms of Fainting • Lightheadedness • Pale, sweaty skin • Blurred vision • Unconsciousness • Nausea Treatment of Fainting 1. Have the person lie down until dizziness passes. a. May also sit with his head between his knees to get the blood flowing to the brain. b. Caution: If a person faints in this position, he may be injured. c. Do not stand up until feeling better. 2. Loosen restrictive clothing. 3. Call 9-1-1 if the victim remains unresponsive for more than 1-2 minutes, has signs of sudden illness, or is injured from a fall. 4. Treat any injuries if the victim fell when fainting. Senior Fainting • Don’t ignore fainting. • May be a sign of a more serious medical condition. • May indicate the need for medication adjustment. • Can cause serious injury if you fall. Postural Hypotension • A drop in blood pressure (hypotension) that occurs with a sudden change in posture. o Change from sitting to standing. o Change from lying down to sitting or standing. • More common in older people. • Can make you feel dizzy, lightheaded, or even faint. • Lasts from a few seconds to a few minutes, depending on the cause. Basic First Aid Lecture Guide Seizures and Fainting 63 Don’t ignore the symptoms! • Take your time when you first change positions. o When you sit up, wait a minute before you stand. Move your legs and pump your ankles to warm up your muscles before you stand. o When you stand up, wait for your body to adjust before you walk. o Take your time when changing positions to allow your body to adjust. • Talk to your doctor about your symptoms. o May be a side effect of some medications. o May be a symptom of a medical problem. e.g. Dehydration, heart condition, untreated diabetes • Be careful in hot environments. o You may sweat and become dehydrated, which lowers your blood pressure. • If you’ve been in bed due to an illness, be careful as you get up. o Muscle weakness contributes to this condition. Vertigo • A sense of movement or rotation of a person or their surroundings. o High risk for falls. o Get medical care to determine the cause. Sum it up • After a seizure or fainting, assess response, breathing, circulation and appearance. • Stay with the person until he or she is responsive, alert, and speaking. • People who lose consciousness may vomit. • Ensure airway remains unobstructed. • Activate EMS. A physician should determine the cause of all first time or repeated seizures. Diabetic Emergencies DVD Ch: 19 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Identify the signs and symptoms of low blood sugar. • Describe the treatment for diabetic emergencies. Key Concepts • Diabetes is a disease that decreases a person’s ability to process sugar. o Most of the food we eat is broken down into glucose for energy. 64 Diabetic Emergencies © 2011 EMS Safety Services, Inc. o Normally the body produces insulin to move glucose from our blood into our cells. o With diabetes, the body either doesn’t produce enough, or the cells do not respond to the insulin that is produced. o Diabetics try to keep their blood glucose levels as normal as possible. • Almost 26 million people in the U.S. have diabetes. • > 25% of adults over age 65 has diabetes. • Diabetes is one of the leading causes of death and disability in the U.S. Three types of diabetes: Type 1 diabetes is an autoimmune disease. • The immune system attacks and destroys the insulin-producing cells in the pancreas. • Accounts for 5-10% of diagnosed diabetes in the U.S. Type 2 diabetes is the most common form of diabetes. • Associated with older age, obesity, family history of diabetes, history of gestational diabetes, physical inactivity, and ethnicity. • 80% are overweight. • Weight loss and increased physical activity can prevent or delay type 2 diabetes. Gestational diabetes develops only during pregnancy. Two types of diabetic emergencies: • High blood sugar o Develops gradually over several days. • Low blood sugar o Sudden onset within minutes o The brain needs glucose in order to function. o A serious, life-threatening medical emergency o If blood glucose falls too low, it can result in a loss of consciousness, brain damage and death. Low blood sugar can quickly develop when a person has: • Taken too much insulin • Exercised too much • Not eaten enough • Had a lot of alcohol to drink o Glucose is released too slowly into the bloodstream. Basic First Aid Lecture Guide Diabetic Emergencies 65 Signs and Symptoms of Low Blood Sugar • Rapid onset: can occur in just a few minutes • Tremors or seizures • Change in behavior: confusion, irritability, aggression, nervousness, uneasiness • Hunger or thirst • Weakness, fatigue • Blurry or double vision • Headache or dizziness • Rapid pulse and breathing • Pale, cool moist skin • Unresponsiveness Treatment of Diabetic Emergency 1. Assess responsiveness, breathing, and appearance. 2. If the person is alert enough to sit up and swallow, give sugar to eat or drink a. e.g. Orange juice, regular soda, a sugar and water solution, honey, glucose tablets b. If the person is drooling or cannot sit up and eat or drink, do not give anything to eat or drink. Call 9-1-1 if: • You cannot quickly find sugar. • The person cannot swallow. • The person does not improve within 5 minutes after taking sugar. • The person becomes unresponsive. Do not give chocolate in a diabetic emergency because it does not contain enough sugar. Tip A person who has had a diabetic emergency should be evaluated by a physician to check medication dosage. Exercise, diet, and medications are the basis of diabetes management. Sum it up • Do not ignore the early symptoms of low blood sugar. o Shaky, nervous, irritable, confused • Provide care before it becomes an emergency. • Give sugar in all diabetic emergencies. o You can quickly improve symptoms of low blood sugar. o There is little risk of worsening the condition of a person with high blood sugar. 66 Diabetic Emergencies © 2011 EMS Safety Services, Inc. Dehydration DVD Ch: DEMONSTRATE: PRACTICE: SUPPLIES: Instructor Note: This topic is only for the CPR and First Aid for Childcare Providers and the Senior Community Student Workbooks. Senior/Child Learning Objectives • Describe the signs, symptoms, and emergency treatment of dehydration. • Understand when a person may be at risk for dehydration. Key Concepts • Children and older people dehydrate more quickly than younger adults. • Severe dehydration can lead to seizures, permanent brain damage, shock and even death. Dehydration occurs when the body does not have as much water and fluids as it should. • Our bodies lose fluid every day from sweat, urine, and feces. • Fluids are replaced through normal eating and drinking. • Dehydration occurs when fluid loss exceeds fluid intake. Causes of Dehydration: • Losing too much fluid from vomiting or diarrhea, excessive urination, excessive sweating, fever o Excessive sweating may occur during extended exercise or on a hot day. o Fever causes more water to evaporate from the body. • Not drinking enough fluids due to: o Loss of appetite or decreased alertness from illness o Nausea o Sore throat or mouth sores • May be a combination of both. Senior • Older people dehydrate more quickly than younger adults. • People with chronic illness are also at higher risk. o Uncontrolled diabetes produces excessive urine output. o Doctor may test your blood sugar to check for undiagnosed diabetes. • Decreased sense of hunger or thirst, so don’t realize you need to drink more. • If the doctor prescribed water pills or fluid restriction, ask the doctor how much to drink when the weather is hot. Basic First Aid Lecture Guide Dehydration 67 Senior Signs and Symptoms of Dehydration Mild/Moderate Dehydration • Dry or sticky mouth • Less active, sleepy • Low urine output • Dark-colored urine (concentrated) Severe Dehydration • Very dry mouth • No tears • No urine output • Skin is loose and wrinkled • Very sleepy, drowsy, lethargic or unresponsive • Sunken eyes • Skin is cool and blotchy (mottled) on arms, hands, legs and feet • Rapid heart rate • Severe weakness, dizziness or lightheadedness • Dizziness when you get up • Signs of shock Treatment of Dehydration Mild Dehydration 1. Drink fluids as tolerated. Frequent, small amounts are better tolerated than a large amount at one time. 2. Treat the cause of dehydration. Follow healthcare provider’s advice for medications and management of diarrhea and vomiting. a. Mild diarrhea: Bland foods, clear liquids as tolerated. b. Mild vomiting: Stop eating solid foods. Wait 2-3 hours, then try to drink clear fluids in small amounts. a. Severe diarrhea and vomiting: Discontinue fluids and solid foods. Call physician or take person to emergency department. May require IV fluids and hospitalization. Moderate/Severe Dehydration 1. Assess response, breathing, and appearance. 2. Call 9-1-1 (activate EMS). 68 Dehydration © 2011 EMS Safety Services, Inc. Child Children and infants dehydrate more quickly than adults due to smaller body weights. Signs and Symptoms of Dehydration Mild/Moderate Dehydration • Dry mouth with few tears when crying • Fussy, less active, not wanting to play • Infants: wet fewer than 6 diapers per day • Children: fewer trips to the bathroom to urinate • Dark-colored urine (concentrated) Severe Dehydration • Very dry mouth • Cry without tears • Skin is loose and wrinkled • Very sleepy, drowsy, or unresponsive • Sunken eyes • Sunken fontanelles in an infant (the soft spot on the top of the head) • Skin is cool and blotchy (mottled) on arms, hands, legs and feet • Rapid heart rate for age • Signs of shock Treatment of Dehydration Mild Dehydration 1. Drink fluids as tolerated. Frequent, small amounts are better tolerated than a large amount at one time. 2. Treat the cause of dehydration. Follow healthcare provider’s advice for medications and management of diarrhea and vomiting. a. Mild diarrhea: Bland foods, clear liquids as tolerated. b. Mild vomiting: Stop eating solid foods. Wait 2-3 hours, then try to drink clear fluids in small amounts. c. Severe diarrhea and vomiting: Discontinue fluids and solid foods. Notify parents or guardians, call physician, or take child to emergency department. May require IV fluids and hospitalization. Moderate/Severe Dehydration 1. Assess response, breathing, and appearance. 2. Call 9-1-1 (activate EMS). Basic First Aid Lecture Guide Dehydration 69 ! If not fully alert, do not give fluids or food. Senior/Child Prevent dehydration before it occurs • Recognize conditions that may cause dehydration and ensure adequate fluid intake. • If a person is sick, treat the symptoms to reduce water loss and encourage fluid intake. o Illness with sore throat may cause pain when drinking fluids o Illness with fever increases water loss through evaporation o Diarrhea and vomiting are common causes of diarrhea. Tip If vomiting or diarrhea seems to be caused by a new medication, talk to your doctor. There are often many choices of medications that are effective but have fewer side effects. Sum it up • Make sure to get enough fluids whether ill or physically active. • When a person is dehydrated due to sweating or hot weather, be alert to heat-related illness. • Get medical care when ill to stop the progression to severe dehydration. • Dehydration that is recognized and treated early usually has a good outcome. Poisoning DVD Ch: 20 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Describe the signs, symptoms, and emergency treatment of poisoning. • Know when to call the poison control center and when to activate EMS. Key Concepts • A poisoning occurs when exposure to a substance results in bodily harm. • Poison control centers receive over 4 million calls each year. • About 91% of poisonings occur at home. • Poisons can be swallowed, inhaled, absorbed through the skin, or injected. 70 Poisoning © 2011 EMS Safety Services, Inc. Swallowed Poisons: eating or drinking • Overdose of medication • Illegal drugs • Child exposures most frequently involve: o Cosmetics or personal care products o Cleaning substances o Analgesics (pain relievers) o Drugs, alcohol o Plants Inhaled Poisons: breathing dust, gases, fumes or mists • Include pesticides, smoke from fires, fumes from glue or paint, vapors and gases. • Carbon monoxide and carbon dioxide are especially hazardous. o They are colorless and odorless. • Confined spaces may contain an accumulation of flammable or toxic gases. o Rescuers can become victims themselves. o Be cautious when there is more than one victim in a confined space. Absorbed Poisons: through skin contact • Poisonous plants: o Poison ivy, poison sumac, poison oak. o Can cause itching, swelling, redness, blisters o Remove exposed clothing carefully and wash skin thoroughly with soap and water ASAP. o Rinse the exposed area with rubbing alcohol to avoid spreading the oil. Contact a physician for treatment. • Chemicals: o Difficulty breathing, fever, headache, generalized weakness o Rashes, blindness Injected Poisons: hypodermic needle, bite or sting • Some insects, snakes and marine animals can inject venom into a victim. • Generally not life-threatening. • They can cause an allergic reaction, which can develop into anaphylactic shock. • Medications and illegal drugs can be injected with a hypodermic needle. Material Safety Data Sheet (MSDS) • Required by OSHA for every chemical and hazardous substance in the workplace. • Provided by the chemical manufacturer. • Must be available to anyone who uses the substance. • Identifies the chemical, how to work with it safely, what to do in case of exposure, etc. DISCUSS: Where are the MSDS kept in your workplace? Basic First Aid Lecture Guide Poisoning 71 Drug Poisoning Drug Poisoning • Includes exposure to illegal, prescription, and over-the-counter drugs. • There are as many emergency department visits for prescription and over-the-counter drug overdoses as there are for illegal drug overdoses. • 93% of poisoning deaths are in adults, usually due to drug poisoning. • In 2007 there were over 27,000 drug overdose deaths in the U.S. Don’t ignore signs of substance abuse! • Be observant for syringes, paraphernalia, needle marks, smell of alcohol, alcohol containers. • Often late or absent at work or school • Irresponsible, anxious, defensive • Agitated, threatening, combative • Mood swings, poor concentration, poor judgment Drugs and alcohol can be dangerous for the user and people around them. • The impaired person may drive or operate machinery at work o In 2009 > 30 million people age 12 or older drove under the influence of alcohol in the U.S. • Drugs and alcohol impair reflexes and coordination • Can lead to seizures or respiratory arrest A rescuer must recognize that a poisoning may have occurred and act fast! • Look for clues to a poisoning. o e.g. Empty bottles, opened containers, disturbed plants • Try to identify the poison, how much and when it was taken. Signs and Symptoms of Poisoning Vary according to the type and method of poisoning. • Throat or abdominal pain • Nausea or vomiting • Drooling, unusual odor on breath • Change in behavior, mood or responsiveness • Sweating • Diarrhea • Difficulty breathing • Seizures • Burns, redness, blisters around the mouth • Chest pain or tightness • Dizziness, headache 72 Poisoning © 2011 EMS Safety Services, Inc. Treatment of Poisoning 1. Check for scene safety and clues to poisoning. 2. Call 9-1-1 (activate EMS) for life-threatening symptoms: o e.g. Unresponsive, difficulty breathing, severe pain 3. Call 1-800-222-1222 (Poison Help) if the person is alert and in no distress. 4. For an inhaled poison, move the victim into fresh air if it is safe for you. 5. For an absorbed chemical poison: o Remove exposed clothing. o Brush off the chemical with a gloved hand. o Rinse the skin with water for at least 20 minutes. 6. For drug or alcohol poisoning: o Calm an agitated or threatening person. o Ensure an escape route if the person becomes violent 7. Place in a position of comfort. o If the person might vomit, place in the recovery position to protect the airway. 8. Monitor closely. Do not give food or drink unless instructed to do so. Do not induce vomiting unless instructed to do so. Do not enter any confined space without proper equipment and training. Poison Control Centers • The poison control center number is (800) 222-1222. • They will connect you with your local poison control center. • An expert is ready to help at any time of day or night. • The call is free and confidential. • They have interpreters. • Many hospital emergency departments call poison control centers for expert information. DISCUSS: Prevent Inhaled Poisoning (optional topic) • Open windows and turn on a fan when using chemical products. • Make sure fuel burning appliances are professionally installed and inspected each year. • Do not mix chemicals or household products. o e.g. Mixing bleach and ammonia creates a poisonous gas • Do not burn charcoal or use gasoline-powered engines in confined spaces such as tents, garages, or poorly ventilated rooms. • Place carbon monoxide and smoke detectors near your bedrooms. Basic First Aid Lecture Guide Poisoning 73 Sum it up • Place in the recovery position if you must leave to get help. o Vomiting is common, especially with drug or alcohol poisoning. • The poison control center number is (800) 222-1222. o Try to give the victim’s age, weight, allergies, and medical conditions. • The best way to handle poisonings is to prevent them. Heat Emergencies DVD Ch: 21 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Describe the signs, symptoms, and emergency treatment for heat exhaustion and heat stroke. Key Concepts • Heat-related emergencies are a true medical emergency. • They usually result from heavy exercise, work, or play in hot weather. • They also occur when people spend a prolonged amount of time in the heat, such as during a heat wave. • > 1,500 people die from excessive heat each year in the U.S. People most susceptible to heat illness: • People who work or exercise outdoors: athletes, laborers, soldiers, workers who wear personal protective equipment such as firefighters • People with poor tolerance to heat: over age 65, the very young, alcoholics, obese, have medical problems Sweating is your body’s natural cooling mechanism. • Evaporation rate decreases as the humidity level rises. • In extreme heat or high humidity, the body’s cooling system may fail. • When you exercise, wear comfortable clothes that allow evaporation. Hydration is critical when working or exercising. • A person who is dehydrated is more susceptible to heat-related illness. • Drink fluids before and during exercise. • Drink enough fluids to replace at least 80% of that lost. • Don’t wait until you are thirsty. • Avoid drinks that make you lose water, such as alcohol or drinks with caffeine. 74 Heat Emergencies © 2011 EMS Safety Services, Inc. Heat Cramps Signs and Symptoms of Heat Cramps • Painful muscle cramps in arms, legs, and abdomen. • Occur during strenuous activity. • Heavy sweating Treatment of Heat Cramps 1. Stop activity and move to a cool location. 3. Gently stretch and massage muscles. 2. Drink sports drink or juice. Heat Exhaustion Signs and Symptoms of Heat Exaustion Similar to signs and symptoms of shock • Sweating • Nausea, vomiting • Intense thirst • Muscle cramps • Pale, cool skin • Elevated temperature, generally less than 104° F • Fatigue, weakness, faintness • Anxiety, headache • Increased heart rate • Dizziness Treatment of Heat Exaustion 1. Stop activity and lie down in a cool location. 2. Remove clothing. 3. Cool the person (cool water bath, spray, fan) 4. Drink sports drink or juice if tolerated. a. No nausea, vomiting, seizure, or confusion. b. Responsive, coherent, able to hold a glass without help. Heat Stroke • The body is unable to regulate its temperature. • Body temperature rises rapidly. • Can lead to brain damage or death if not treated quickly. Basic First Aid Lecture Guide Heat Emergencies 75 Signs and Symptoms of Heat Stroke • High body temperature, usually above 104° F • Slurred speech • Hot, dry, flushed skin (no sweating) • Seizures o Skin may be moist if heat stroke was caused by exertion. • Confusion, dizziness • Severe headache • Rapid breathing and heart rate • Unresponsiveness Treatment of Heat Stroke 1. Call 9-1-1 (activate EMS). 2. Quickly cool the victim. a. Immerse in water up to the neck. b. Spray, sponge, or shower with cool water. c. Place ice packs against the groin, armpits, and sides of the neck. Senior • Older people are more prone to heat illness due to physical changes in the body: o Fewer sweat and oil glands in the skin result in less effective heat loss through evaporation. o Decreased blood circulation to the skin results in less heat radiation through the skin. o A temperature that does not seem too hot to others could cause heat illness in an older person. • Scene size-up should include the temperature of the home. • An environment that is too warm or a person dressed too warmly could also indicate a heat-related emergency. Child • Do not leave a child alone in a car on a hot day. • When the outside temperature is 93° F, the temperature inside a car can reach 123° F in just 20 minutes. Sum it up • Heat exhaustion can quickly progress to heat stroke. • Heat stroke can lead to brain damage or death if not treated promptly. • Recognize and care for heat-related illness before it becomes life-threatening. 76 Heat Emergencies © 2011 EMS Safety Services, Inc. Cold Emergencies DVD Ch: 22 DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • List actions that can help prevent a cold-related emergency. • Describe the signs, symptoms and treatment of hypothermia and frostbite. Key Concepts • Your body loses heat in water up to 25 times faster than in air. • Cases have been recorded in temperatures as high as 65° F. Hypothermia • Hypothermia is abnormally low body temperature. • Immersion in cold water is the most common cause of hypothermia. • Hypothermia is a serious, life-threatening condition. Signs and Symptoms of Hypothermia • Shivering • Slow breathing and pulse • Cold, pale skin • Unresponsiveness • Drowsiness, exhaustion Treatment of Hypothermia 1. Move to a warm environment. 2. Call 9-1-1 (activate EMS). 3. Gently remove damp clothing, dry the skin, and replace with dry clothing. a. Cover the head and neck and wrap in blankets. 4. If alert, give warm liquids. 5. Monitor response and breathing. 6. Use your own body heat to warm the person. 7. If far from medical care, warm with heat pads or containers of warm water. a. Keep a barrier between the heat source and the skin to avoid burning the person, since sensation may be impaired. Basic First Aid Lecture Guide Cold Emergencies 77 Do not manipulate the extremities. Moving the arms and legs could force cold blood back to the heart, which may result in cardiac arrest. Do not give alcohol (may cause heat loss) or coffee (may cause dehydration). Do not apply direct heat if you are near medical care. Do not immerse in warm water because it will warm the person too quickly. Frostbite • Frostbite is the actual freezing of body tissues. • Caused by prolonged exposure to cold. • Children are more at risk, because they lose heat more rapidly than adults. Signs and Symptoms of Frostbite • Pale, cold, waxy skin • Blisters, hardened tissues • Painful burning sensation, or numbness Treatment of Frostbite 1. Move to a warm location. 6. Place frostbitten part next to your body. 2. Call 9-1-1 (activate EMS). 7. If help is delayed, immerse the frostbitten part in warm water for 20-30 minutes. 3. Remove wet clothing, dry the skin, and replace with dry clothing. 4. Remove rings, bracelets and watches. 5. Cover with dry sterile dressings. o 100° - 104° F 8. Slowly warm the frozen areas over 25-40 minutes. Do not pop blisters. Do not rewarm with direct heat (over a stove, open flame or heating pad) Do not rub frostbitten skin. Do not rewarm the part if it may refreeze. Senior Seniors are more susceptible to cold emergencies. • Decreased ability to sense a change in temperature. o The body is supposed to sense a change in temperature, then respond by generating heat (shivering) or dissipating heat (sweating). o Temperature may need to change by 10° F before can sense the change. o Loss of muscle mass results in less shivering in cold temperatures to keep the body warm. o Weight loss and less fat under the skin results in less insulation against the cold. • People with medical conditions that impair sensation, blood flow or movement are at increased risk for hypothermia. 78 Cold Emergencies © 2011 EMS Safety Services, Inc. Child Children are more prone to heat loss due to: • Body temperature regulation mechanism is not fully developed. • Lose more heat through their head, which is disproportionately larger than an adult’s head. • May not dress appropriately in the cold. • May not go indoors when feeling cold. Sum it up • Immersion in cold water is the most common cause of hypothermia. • Take precautions to prevent a cold-related emergency. Drowning DVD Ch: DEMONSTRATE: PRACTICE: SUPPLIES: Instructor Note: This topic is only for the CPR and First Aid for Childcare Providers Student Workbook. Learning Objectives • Know how to respond safely to a drowning emergency. • Understand that a small child should never be left alone when there is a chance of drowning. Key Concepts • About 4,000 people die each year from unintentional drowning. • Drowning is the leading cause of injury death in children age 1-4, and the 2nd leading cause of death in children under age 14. • Nonfatal drowning can result in severe brain damage with impaired memory, learning, and basic functioning. • Drowning is preventable. Water Safety Water safety is especially important in a home with small children. • Drowning can occur quickly and in very little water. o e.g. Bucket, toilet, bathtub with just 1” of water. • Always closely supervise a child who is near any water. Respond Safely and Quickly 1. Consider scene safety first. One victim can quickly become two victims. a. Use caution if you are not a good swimmer or are not trained in the water rescue of a panicked victim. 2. Remove the victim from the water as quickly as possible, if it is safe to do so. Basic First Aid Lecture Guide Drowning 79 a. If the victim is still in the water, send a bystander to activate EMS and get an AED. b. Use rescue equipment if available (e.g. Rope, boat, life preserver). c. Specially trained rescuers may give rescue breaths while still in the water. 3. Assess responsiveness. a. If responsive, treat for hypothermia. i. If no traumatic injury, remove wet clothing, dry the person, and replace with dry clothing or cover with blankets. ii. Move to a warm location. iii. If potential spinal injury, do not move the person. Stabilize head and neck together in the position found. Wait for EMS responders. 4. If unresponsive, assess breathing. a. If no breathing or only gasping, begin CPR if you are trained. i. If alone with a child victim, perform CPR for 2 minutes before leaving to activate EMS. ii. If alone with an adult victim, activate EMS and get an AED before beginning CPR. 5. Continue CPR until the victim begins to move or professional rescuers arrive and take over. ! Drowning victims commonly vomit during CPR. Carefully log roll the victim to the side, sweep the mouth clear, roll back, and continue CPR. Diving or surfing accident • Consider the possibility of a spinal injury. • The priority is airway, breathing, and circulation, because without them the victim will die. • Try to stabilize the neck and avoid moving the victim during care. Sum it up • The speed of response is critical for a drowning victim. o Giving immediate chest compressions and rescue breaths may possibly revive a drowning victim without the use of an AED. • All drowning victims should be seen by a physician. Even if they seem fully recovered, complications may develop later. Bites and Stings DVD Ch: DEMONSTRATE: PRACTICE: SUPPLIES: Learning Objectives • Know which insects and snakes are poisonous. • Know the proper treatment for bites and stings. 80 Bites and Stings © 2011 EMS Safety Services, Inc. Animal or Human Bites Key Concepts • Almost 40% of U.S. households have a pet dog. o Dogs bite more than 4.7 million people each year. o 2.8 million of the dog bite victims are children. • Rabies and tetanus are the biggest concerns because there is no cure. o A bite from a skunk, raccoon, bat, fox, or another mammal that is unprovoked or behaving strangely is treated as a rabies exposure. o Tetanus, also known as lockjaw, is contracted when a cut or wound is contaminated with the tetanus bacteria. Treatment of Animal Bites 1. Ensure scene safety. Do not try to capture a potentially rabid animal. 2. Wash a minor wound immediately with soap and lots of water. a. Wound irrigation under pressure can reduce the risk of rabies or bacterial infection. 3. Control bleeding with direct pressure. 4. Apply antibiotic ointment (if no allergy) and cover with a sterile dressing. 5. Report bites to a police or animal control officer. • Call 9-1-1 if there is severe bleeding, the animal remains a danger, or the animal may have rabies. • Get medical care for further wound cleaning, stitches, rabies vaccination, signs of infection, or care of bites to the face, neck or hands, deep puncture wounds, or large lacerations. DISCUSS: Tips to Avoid Dog Bites • If approached by a dog, stand still while it determines you are not a threat. • If threatened by a dog, remain still, avoid eye contact, do not run, slowly back away. • Teach children not to annoy or tease animals. • Be cautious around moms with pups. • Do not approach an unknown animal. • Do not disturb an eating or sleeping dog. • Do not leave young children or strangers alone with a dog. • Do not attempt to break up a dog fight. • Ask permission from a dog’s owner before petting a dog. • If knocked down by a dog, curl into a ball, protect your face and lie still. Human Bites • Can be as dangerous as animal bites due to possibility of infection. • May occur when very young children are playing, during a fight, in a mental institution, or in a prison. • A physician should always evaluate human bites. Basic First Aid Lecture Guide Bites and Stings 81 Snakebites Key Concepts • 7,000 - 8,000 venomous snakebites each year in the U.S. • Most snakes are not poisonous. Four types of poisonous snakes found in the U.S.: o Rattlesnakes create a rattling sound by shaking the rings at the end of their tail. They are responsible for most poisonous snakebites in the U.S. o Coral snakes have yellow, red and black rings along their bodies. o Water moccasins (cottonmouths) have a white, cottony lining in their mouth. o Copperheads have a copper-colored head and a reddish-brown hourglass pattern on the body. Signs and Symptoms of Snakebites • Fang marks (2 small puncture wounds) • Weakness, sweating • Burning pain • Rapid heart rate, low blood pressure • Rapid swelling within minutes • Seizures, fainting, dizziness • Nausea and vomiting • Numbness and tingling Treatment of Snakebites 1. Scene safety. Call 9-1-1 if you suspect the bite is from a venomous snake. 2. Keep the victim calm and still, with the bite area lower than the heart. Decrease activity. 3. Wash the wound gently with soap and running water. 4. Remove jewelry and constrictive clothing; swelling can progress rapidly. 5. Wrap an elastic bandage around the entire bitten arm or leg, starting furthest from the heart. a. Use overlapping turns. b. Wrap snugly but still allow a finger to slip under the bandage. c. Check temperature and sensation below the wrap to make sure it is not too tight. 6. Get medical help immediately. Antivenom must be given within a few hours. 7. Mark the border of the swelling/redness every 15 minutes with a pen. Do not apply a tourniquet or ice. Do not cut the wound or apply mouth suction. Do not try to capture the snake. Do not approach a dead or dying snake. Do not pick up a snake or play with it unless you are properly trainedl Treat all unknown snakes as poisonous. Consider the need for a tetanus shot. 82 Bites and Stings © 2011 EMS Safety Services, Inc. Insect Stings Key Concepts • Insect stings are rarely serious. • A sting will normally cause localized redness, swelling, burning and itching. • 2% of the U.S. is severely allergic and will develop anaphylaxis; 40 - 50 die each year. Treatment of Mild Reaction 1. If stung by a bee, quickly scrape off the stinger with your fingernail or a straight-edged object. 2. Speed is important; 90% of the venom is delivered within 20 seconds. 3. Wash with soap and water. 4. Apply an ice pack wrapped in a moist cloth for 10 minutes on, then 10 minutes off. 5. Consider over-the-counter medications for itching, pain & inflammation. 6. See your physician if the swollen area is large, if the sting site is in the mouth or nose, or if you develop mild nausea, intestinal cramps or diarrhea. Signs and Symptoms of Severe Reaction Anaphylaxis • Difficulty breathing or wheezing • Hives and rash • Dizziness, faintness • Facial, throat or tongue swelling; difficulty swallowing • Stomach cramps, nausea or diarrhea • Shock Treatment of Severe Reaction 1. Send a bystander to call 9-1-1 (activate EMS). 2. If victim is carrying an epinephrine auto-injector, help administer it if requested and you are trained. 3. Observe for signs of shock; treat as indicated. Spider Bites and Scorpion Stings Key Concepts • Spiders bite and scorpions sting to defend themselves. • > 50,000 species of spiders; 2 are dangerous to humans. • 1 type of scorpion is dangerous to humans. Black widow spider • Shiny black with a red or orange hourglass-shaped mark on its abdomen. • Found in dark and damp places. Basic First Aid Lecture Guide Bites and Stings 83 • Death is rare; exceptions may be young children, the elderly, and people with cardiovascular disease. Brown recluse (violin spider) • Light brown color and dark brown fiddle-shaped mark on its upper back. • Hide in boxes, closets, basements, and garages. Bark scorpion • Scorpions in the U.S. are found mostly in the southwest. • Only the bark scorpion (found primarily in Arizona, New Mexico and on the California side of the Colorado River) is dangerous to humans. • Scorpions only sting when provoked. General Signs and Symptoms of Spider Bites & Scorpion Stings • Severe pain, burning • Headache, dizziness, weakness • Chest pain • Sweating, fever, cramps • Rigid muscles, painful joints • Nausea, vomiting, salivation • Redness, swelling, rash, itching • Rapid heart rate & blood pressure • Small puncture wounds • Respiratory distress, anxiety • Blister or ulcer that may turn black • Unresponsiveness Treatment of Spider Bites & Scorpion Stings 1. Call 9-1-1 (activate EMS) if: a. A suspected bite from a black widow, brown recluse, or scorpion. b. Any life-threatening signs are present. 2. Wash the wound with soap and water. 3. Apply an antibiotic ointment if no allergy. 4. Apply an ice pack wrapped in a moist cloth. 5. If you killed the spider or scorpion, bring it with you for identification. ! Children under 10 and older people are more at risk to develop serious symptoms. Antivenom is available for scorpion stings or black widow bites. Tick Bites Key Concepts • Found in the woods, shrubbery, high grasses, gardens, marshes & beaches. • Most tick bites are harmless; some transmit life-threatening diseases. • Check for ticks on parts of the body that bend, on top of the head, behind the ears, on the neck and hairline, where clothing presses on the skin. 84 Bites and Stings © 2011 EMS Safety Services, Inc. Tick Removal and Treatment 1. Remove as soon as possible. Risk of disease transmission increases after 24 hours. 2. Use fine-tipped tweezers to grasp the tick close to the skin. 3. Lift the tick straight out without crushing or squeezing it. 4. Save the tick for testing in a sealable bag or container if you are in an area of high risk. 5. Wash wound with soap and water. 6. Swab with an antiseptic solution, then apply an antibiotic ointment if no allergy. 7. Seek medical care if: a. You cannot remove the tick completely. b. You develop a rash or flu-like symptoms. 8. High-risk persons should consult with their physician. a. e.g. Pregnant, living in areas with tick-borne disease. Do not use petroleum jelly, alcohol, or a hot match to kill the tick. Do not handle the tick with your bare hands. Sum it up • Most bites and stings are preventable. o Teach children to treat dogs with caution. o Keep your hands and feet out of areas you can’t see. o Use insect repellant. • If a bite victim develops serious symptoms, seek medical help immediately. Basic First Aid Lecture Guide Bites and Stings 85 How Would You REACT? QUESTIONS SCENARIOS Home 1 Someone having difficulty breathing will probably choose to: A small child has eaten part of an unknown type of plant in the back yard. He does not appear to be in distress. How would you REACT? a. Lie down b. Sit up c. Walk 2 After a seizure, a rescuer should check a victim to make sure he or she is breathing and is not injured. True Community False You are at the park when you see a teenager trying to break up a fight between two dogs. You see one of the dogs bite him on the leg, and then run away. His pant leg is torn, and you can see a small open wound. How would you REACT? 3 A person who is experiencing a diabetic emergency should be given sugar. True False School 4 Most poisonings involve children and occur: a. b. c. d. In the home At school In the childcare setting At work You are at school when you see a small child sitting on a bench supporting herself with her arms. When you get closer you can hear her wheezing, and her lips appear blue. How would you REACT? Work 5 Following a snakebite, it is important to capture the snake to identify it. 86 True False How Would You REACT? It is a hot day. You are pouring cement when your coworker tells you he feels dizzy and weak. His skin appears pale, and he is sweating profusely. How would you REACT? © 2011 EMS Safety Services, Inc. First Aid Kit Contents First Aid Kit Contents • The contents of a first aid kit and even the container holding the supplies should be determined by the kit’s purpose and location. • A first aid kit may be used for the treatment of minor cuts and headaches, or may be an “emergency kit,” containing an AED and supplies to treat specific workplace hazards. • Follow federal and state OSHA guidelines for first aid kits at your workplace. • Check the expiration dates and contents regularly. • Store your first aid kit safely out of the reach of young children, but easily accessible for adults. Instructor Note: End of Basic First Aid Lecture Guide Maltreatment of Children DVD Ch: DEMONSTRATE: PRACTICE: SUPPLIES: Instructor Note: This topic is only for the CPR and First Aid for Childcare Providers Student Workbook. Learning Objectives • Recognize the signs of child maltreatment. • Know how to report it if needed. Key Concepts • Child maltreatment is when a child or young person is being harmed physically, emotionally, sexually, or through neglect of basic needs. • There are > 3 million reports of child abuse or neglect each year in the U.S. o Almost 800,000 children are actual victims of maltreatment. • Teachers, caregivers, and healthcare professionals are usually required by law to report their suspicions to child protective services, social services, or local police. Types of Maltreatment Physical abuse: The willful infliction of physical injury to a child. • Shaken baby syndrome is a leading cause of brain injury in infants. Emotional or psychological abuse: A deliberate attempt to make a child feel worthless and incompetent. • e.g. Rejecting, isolating, terrorizing, ignoring, or corrupting Sexual abuse: The rape, molestation, prostitution, or sexual exploitation of a child. • May also be the employment or coercion of a child to engage in, assist in, or simulate sexually explicit conduct. • The incidence of sexual abuse increases with child age. Neglect: Depriving a child of basic physical needs. • e.g. Shelter, warmth, supervision, safety, medical care • The most common form of child maltreatment. Basic First Aid Lecture Guide First Aid Kit Contents / Maltreatment of Children 87 Warning Signs of Abuse Child: • Unexplained or suspicious injuries • Multiple healing injuries • Untended medical conditions • Delayed physical or emotional development • Frequent absence from school • Extremes in behavior (e.g. Overly compliant, angry, aggressive) • Sudden change in school performance • Sudden refusal to participate in sports or change for gym • Does not want to go home • Frightened of certain adults • Lack of adult supervision • Steals or begs for food or money • Poor hygiene or inadequate clothing for the weather • Drug or alcohol abuse • Self-destructive or depressed • History of running away or suicide attempt • Sophisticated sexual behavior or knowledge • Reports abuse or neglect Parent or Caregiver: • Gives implausible explanation for injury • Unconcerned or indifferent about the child • Considers the child bad, worthless, or a burden • Constantly criticizes or blames the child • Uses or recommends harsh punishment • Expects perfection that the child cannot achieve • Extremely protective or secretive about the child • Drug or alcohol abuse • History of being abused as a child Sum it up • Accusation of child abuse is very serious. • Try to rule out causes other than abuse, but do not delay reporting your suspicions. • Do not count on someone else to report signs of abuse or neglect. • Know your local and state guidelines, and post telephone numbers for reporting. 88 Maltreatment of Children © 2011 EMS Safety Services, Inc.