Contents - Exercise Sciences!
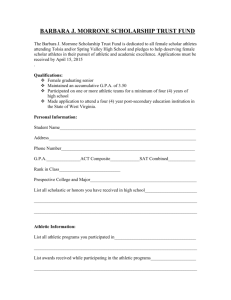
advertisement

BYU Athletic Training Procedures and Appendix Contents Communicable Disease Policy ..............................................................................................................................4 MISCELLANEOUS INFORMATION .......................................................................................................................6 TABLE 1. Work restrictions for health care personnel exposed to or infected with infectious diseases in health care settings.....................................................................................................................................................8 ATHLETIC TRAINING ROOM INFORMATION ................................................................................................... 10 RULES FOR THE BYU ATHLETIC TRAINING ROOM .................................................................................. 10 ATHLETIC TRAINING ROOM CLOSING DUTIES .......................................................................................... 11 FILING MEDICAL RECORDS............................................................................................................................. 14 Local Hospital Information ................................................................................................................................... 18 OSHA Regulations for Exposure ............................................................................................................................. 19 EXPOSURE CONTROL POLICY FOR ................................................................................................................. 20 CONTROL OF INFECTIOUS DISEASES ............................................................................................................ 20 National Athletic Trainers’ Association Code of Ethics ............................................................................... 28 Job Descriptions ......................................................................................................................................................... 31 Springville High School .......................................................................................................................................... 32 Pleasant Grove High School .................................................................................................................................... 33 BYU Men‘s Volleyball ............................................................................................................................................ 33 BYU Men‘s Lacrosse .............................................................................................................................................. 35 American Fork High School .................................................................................................................................... 36 Timpanogos High School ........................................................................................................................................ 38 Cougarettes .............................................................................................................................................................. 39 Utah Valley University ............................................................................................................................................ 40 BYU Women‘s Volleyball ...................................................................................................................................... 41 BYU Gymnastics ..................................................................................................................................................... 41 BYU Women‘s Tennis ............................................................................................................................................ 41 BYU Baseball .......................................................................................................................................................... 42 UVU Track and Cross Country ............................................................................................................................... 43 BYU Football .......................................................................................................................................................... 43 Orem High School ACI-Dujuan Shakespaere ......................................................................................................... 44 Utah Valley Sports Medicine ................................................................................................................................... 46 On-Campus BYU Emergency Action Plans ............................................................................................................ 47 Emergency Procedure for MILLER PARK BASEBALL FIELD ....................................................................... 48 Emergency Procedure for SOFTBALL .............................................................................................................. 49 Emergency Procedure for FOOTBALL .............................................................................................................. 51 Emergency Procedure for GYMNASTICS ........................................................................................................ 54 Emergency Procedure for TENNIS .................................................................................................................... 56 Emergency Procedure for SOCCER .................................................................................................................. 57 1 BYU Athletic Training Procedures and Appendix Emergency equipment located on site: ................................................................................................................. 57 Emergency Procedure for SWIMMING & DIVING ........................................................................................... 58 Emergency Procedure for MEN‘S & WOMEN‘S BASKETBALL .................................................................... 60 Emergency Procedure for VOLLEYBALL.......................................................................................................... 61 Emergency Procedure for DANCE ..................................................................................................................... 65 Emergency Procedure for EXTRAMURAL SPORTS ...................................................................................... 67 Emergency Procedure for CHEER ..................................................................................................................... 70 Practice procedures ............................................................................................................................................... 70 Off-Campus Emergency Action Plans ..................................................................................................................... 73 Springville High School Emergency Action Plan .............................................................................................. 74 Timpview Football Emergency Action Plan ....................................................................................................... 76 Timpview Baseball Emergency Action Plan ...................................................................................................... 78 Timpview Boys‘ & Girls‘ Soccer Emergency Action Plan ................................................................................ 80 Timpview Softball Emergency Action Plan ........................................................................................................ 82 Timpview Boys‘ & Girls‘ Basketball and Volleyball Emergency Action Plan ................................................ 84 Timpview Boys‘ & Girls‘ Track Emergency Action Plan .................................................................................. 86 Pleasant Grove High School Athletics Emergency Action Plan ..................................................................... 88 Orem High School Emergency Action Plan ...................................................................................................... 90 American Fork High School Football Emergency Action Plan ....................................................................... 93 American Fork High School Soccer Emergency Action Plan ......................................................................... 95 American Fork High School Volleyball/Basketball/Wrestling Emergency Action Plan ............................... 97 Mountain View High School Emergency Action Plan ...................................................................................... 99 Lehi High School Emergency Action Plan ....................................................................................................... 101 Emergency Plan for Timpanogos High School ............................................................................................... 103 Physical & Sports Therapy Services — Springville Emergency Action Plan ............................................. 105 Athletic Training Course Descriptions and ........................................................................................................... 107 Learning Outcomes ................................................................................................................................................. 107 EXSC 302 ............................................................................................................................................................ 108 EXSC 320 ............................................................................................................................................................ 108 EXSC 321 ............................................................................................................................................................ 108 EXSC 362 ............................................................................................................................................................ 109 EXSC 394 ............................................................................................................................................................ 109 EXSC 395 ............................................................................................................................................................ 109 EXSC 400 ............................................................................................................................................................ 109 EXSC 414 ............................................................................................................................................................ 110 EXSC 415 ............................................................................................................................................................ 110 EXSC 416 ............................................................................................................................................................ 111 EXSC 417 ............................................................................................................................................................ 111 EXSC 418 ............................................................................................................................................................ 112 2 BYU Athletic Training Procedures and Appendix EXSC 419 ............................................................................................................................................................ 112 EXSC 423 ............................................................................................................................................................ 112 EXSC 460 ............................................................................................................................................................ 113 EXSC 463 ............................................................................................................................................................ 113 EXSC 464 ............................................................................................................................................................ 114 EXSC 468 ............................................................................................................................................................ 114 EXSC 494 ............................................................................................................................................................ 114 EXSC 495 ............................................................................................................................................................ 114 EXSC 498 ............................................................................................................................................................ 115 EXSC 501 ............................................................................................................................................................ 115 HLTH 320 ............................................................................................................................................................. 116 MMBIO 221 .......................................................................................................................................................... 116 NDFS 310 ............................................................................................................................................................ 116 PDBIO 220 ........................................................................................................................................................... 116 PDBIO 305 ........................................................................................................................................................... 116 PSYCH 111 .......................................................................................................................................................... 116 STAT 221 ............................................................................................................................................................. 117 STDEV 170 .......................................................................................................................................................... 117 Competencies and Clinical Proficiencies ............................................................................................................... 118 3 BYU Athletic Training Procedures and Appendix Communicable Disease Policy Brigham Young University College of Health and Human Performances Department of Exercise Sciences Prevention of Infection and Disease Transmission Policy (Modified with permission from Duquesne University) The purpose of this policy is to protect the health and safety of the students enrolled in the Athletic Training Education Program as they participate in the didactic and clinical education experiences required by the program. It is designed to provide students, clinical instructors, and faculty with a plan to assist in the management of students with infectious diseases as defined by the Centers for Disease Control and Prevention (CDC). This policy was developed using the recommendations established by the CDC for health care workers; the recommendations were established on the basis of ―existing scientific data, theoretic rationale, applicability and potential economic impact.‖ Guidelines for Prevention of Exposure and Infection 1. All students must attend required OSHA and Blood-borne pathogen lecture annually to learn, practice, and be evaluated as successfully performing all skills and tasks that will assist them in limiting their exposure in health care settings. 2. To limit exposure, students are required to use proper hand washing techniques and practice good hygiene at all times. 3. Students are required to use Universal Precautions AT ALL TIMES when functioning as health care professional students in health care settings and/or working with potential sources of infectious disease. Guidelines for Managing Potential Infection 1. A student who has been exposed to a potential infection before, during, or after a clinical experience should report that exposure to his/her clinical instructor. 2. A student, who demonstrates signs of infection or disease that may place him/her and/or his/her patients at risk, should report that potential infection or disease immediately to the Student Health Center. If a student is in doubt of his/her health risk, that student should immediately report to the Student Health Center for evaluation by a qualified health professional. A student may utilize his/her family physician; however, the same requirements and notifications yielded from the Health Center will be required of the personal physician. 3. If a student feels ill enough (e.g. fever, diarrhea, other acute symptoms) to miss more than one day of class or clinical experience, that student should be evaluated by the Student Health Center or his/her family physician. 4. Upon review by the Student Health Center or the personal physician, the student must make it known that he/she is an Athletic Training student and that he/she is required to furnish the ATEP Director with notification of his/her health status and ability to participate in the required academic and clinical activities of the educational program. 4 BYU Athletic Training Procedures and Appendix 5. 6. 7. Upon receipt of the health status notification from the Student Health Center or the family physician, the student must present that notification to the ATEP Director or the Clinical Education Coordinator who will inform the other appropriate Athletic Training faculty who (in compliance with HIPAA) are required to know the student‘s health status. The health notification will be placed in a sealed envelope in the student‘s program file. The student is required to notify his/her clinical instructor(s) of missed clinical experiences; this need to miss clinical time will be confirmed by the Clinical Education Coordinator with the designated clinical instructor. The ATEP Director will assume responsibility for the notification of the student‘s professors if the student is required to miss further class time. The student is responsible to keep the ATEP Director and the Clinical Education Coordinator informed of conditions that require extended care and/or missed class/clinical time. Additional health status notifications will be required until such time as the student is cleared to return to full participation in all academic and clinical requirements of the academic program. 5 BYU Athletic Training Procedures and Appendix MISCELLANEOUS INFORMATION Bulletin boards: The bulletin boards in the training room and just outside the training room are used for information for the students:, job placement, announcements, order forms for sweatshirts and kits, etc. You should check these periodically. The dry erase boards are used for important announcements; students must check these daily. Eating with Teams: Legends Grille privileges are available for a limited number of students during two-a-day football practices. Students assigned to Men's basketball and Doctor‘s office may also have dinner with the teams. Occasionally, other teams will eat at the Legends Grille; students will be notified if they are invited to partake. Mailboxes: Each ATS will have a mailbox. With the large program ATEP at BYU, these mailboxes are provided as a method of improving communication between staff and students. This method of communication is useless if you do not check your box periodically. Please check them daily, especially if you are assigned to a sport at BYU. Also, dDo not use them for storage. Lockers: Lockers are provided to a few senior athletic training students with assignments at BYU. Usually, priority is given those students who arrive in early August for assignments. Athletic issue, which is required for working out in the athletic weight room, is given only with a locker. Only a limited number of lockers are allotted to us; please, do not feel slighted if you do not receive one. While working in the training room, all personal belongings should be kept in your locker. If you do not have a locker, these should be kept in the designated area in the storage room. Backpacks, coats, books, etc. should not be brought into the training room. Anything valuable should be left at home; due to the high traffic in this area, you are taking a great risk leaving anything like that valuable around. Telephones: Telephones should be answered by saying ―Athletic training room, ____ speaking.‖ If the call is for someone who is not there, please take a message. The telephones in the athletic training room are not for conversations with friends or outside business, but may be used by students when necessary. Athletes may not use the phones without staff authorization. Trucks and carts: The truck may bey used for any athletic training room business. A staff trainer must approve the use of the truck by a student. However, if you are given an assignment that would be made easier by using the truck, by all means, go ahead and ask! If you are taking the truck, please sign out on the log located in the secretaries' office. Also, let others know where you are going and how long you will be. If you take the truck, you must also take a radio with you. The carts (the limousine, the gator, or the small cart) should be used as needed. Several sports use the carts regularly. If you need one for something out of the ordinary, check with a staff athletic trainer. The carts run on gasoline. When the tank is about 1/4 empty, it should be filled with the gas cans in the garage. Once you start using the gas in the last can, the others should be taken to the station across the street from the car pool (900 North just west of 900 East) and filled. The secretary has a gas card you will use to fill the cans. If the truck or carts break down, arrange to have them repaired ASAP. Obviously, the the truck and the carts should be driven carefully: please, do not hit a pedestrian or another car. 6 BYU Athletic Training Procedures and Appendix Telephones: Telephones should be answered by saying ―Athletic training room, ____ speaking.‖ If the call is for someone who is not there, please take a message. The telephones in the athletic training room are not for conversations with friends or outside business, but may be used by students when necessary. Athletes may not use the phones without staff authorization. 7 BYU Athletic Training Procedures and Appendix TABLE 1. Work restrictions for health care personnel exposed to or infected with infectious diseases in health care settings Disease Conjunctivitis (pink eye) Diarrheal Diseases Acute stage Convalescent stage Salmonella spp. Work Restriction Restrict from pt contact and contact w/pt environment Duration Until discharge ceases Restrict from pt contact, contact w/patient's environment or food handling Restrict from care of high-risk pts Until symptoms resolve Diphtheria Exclude from duty Enteroviral infections Restrict from care of infants neonates, and immuno-compromised patients and their environments Restrict from pt contact, contact w/patient's environment, and food handling Do not perform exposure-prone procedures until counsel from an expert review panel has been sought; panel should make recommendations; refer to state regulations Hepatitis A Hepatitis B (Personnel with acute or chronic Hep B e antigenemia who perform exposure-prone procedures Herpes simplex Hands (herpetic whitlow) Orofacial Human Immunodeficiency virus (HIV) Until symptoms resolve; consult w/local and state officials regarding need for negative stool cultures Until antimicrobial therapy completed and 2 cultures obtained >24 hrs apart are negative Until symptoms resolve Until 7 days after onset of jaundice Until Hep B e antigen is negative Restrict from patient contact and contact with patient's environment Evaluate for need to restrict from care of high-risk patient Do not perform exposure-prone invasive procedures until counsel from an expert review panel has been sought; panel should make recommendations; refer to state regulations Until lesions heal Exclude from duty Exclude from duty Until 7 days after rash appears From 5th day after 1st exposure through 21st day after last exposure and/or 4 days after rash appears Until 24 hours after start of effective therapy Measles Active Post exposure Meningococcal infections Exclude from duty Reference: Bolyard EA, Tablan OC, Williams WW, Pearson ML, Shapiro CN, Deitchman SD, and The Hospital Infection Control Practices Advisory Committee. Special Article: Guideline for Infection Control in Health Care Personnel, 1998. Centers for Disease Control and Prevention. Public Health Service. US Department of Health and Human Service. 8 BYU Athletic Training Procedures and Appendix Mumps Active Post exposure Exclude from duty Exclude from duty Pediculosis (lice) Restrict from patient contact Pertussis (whooping cough) Active Exclude from duty Post exposure Rubella Active Post exposure Scabies Staphylococcus aureus Infection Active (draining skin lesions) Until 9 days after onset of parotitis From 12th day after 1st exposure through 26th day after last exposure or until 9 days after onset of parotitis Until treated and observed to be free of adult and immature lice From beginning of catarrhal stage through 3rd week after onset of paroxysms or until 5 days after start of effective antimicrobial therapy Until 5 days after start of effective antimicrobial therapy Exclude from duty Exclude from duty Until 5 days after rash appears Exclude from duty From 7th day after 1st exposure through 21st day after last exposure Until cleared by medical evaluation Restrict from patient contact Restrict from contact with patients Carrier state Streptococcal infection, group A Restrict from patient care, contact with Until lesions have resolved and patient's environment or food handling No restriction, unless personnel are epidermiologically linked to transmission of the organism Until 24 hours after adequate treatment patient's environment or food handling started Tuberculosis Active disease Exclude from duty Until proved noninfectious Varicella (chicken pox) Active disease Postexposure Exclude from duty Exclude from duty Until all lesions dry and crust From 10th day after 1st exposure through 21st day (18th day if VZIG given) after last exposure Cover lesions; restrict from care of high-risk patients Restrict from patient contact Until all lesions dry and crust Restrict from patient contact from 10th day after 1st exposure through 21st day (28th day if VZIG given) after last exposure or, if varicella occurs until all lesions dry and crust Until acute symptoms resolve of high risk patients or contact with their environment during community outbreak of RSV and influenza Zoster Localized, in healthy person Generalized or localized in Immunosuppressed person Post exposure Viral respiratory infections, acute febrile Consider excluding from the care 9 Until all lesions dry and crust BYU Athletic Training Procedures and Appendix ATHLETIC TRAINING ROOM INFORMATION RULES FOR THE BYU ATHLETIC TRAINING ROOM 1. You will not receive treatment or be taped if you are not in compliance with BYU dress and grooming standards. 2. No food or drinks are allowed in the athletic training room. 3. No athletic equipment or athletic bags are allowed in the athletic training room. 4. All athletes must shower before receiving treatment. 5. All rehab must be approved by the team athletic trainer. 6. No shoes on treatment table or taping bench. 7. Cardio equipment is for rehab only. 8. All rehab equipment must remain in the athletic training room. 9. Everyone must shower and wash all dirt, grass, and rubber pellets off before using the hydro area. 10. All tape must be removed before entering the hydro area. 11. Appropriate/modest attire must be worn in the hydro area. 12. No running, jumping, diving or horseplay in the hydro area. 13. Do not turn on/off turbines while in the whirlpool. If you encounter a student athlete who is being non-compliant, remind them of the Athletic Training Room rules. If they persist in being non-compliant, notify a Staff member immediately. Do not attempt to enforce the Athletic Training Room rules yourself. 10 BYU Athletic Training Procedures and Appendix ATHLETIC TRAINING ROOM CLOSING DUTIES All ATSs will be scheduled to assist in closing the Athletic Training Room. Closing duties will begin at 6:00 p.m. and can take 1–2 hours depending on the number of teams practicing. Closing duties are part of your clinical assignment, practicum, and the profession. Part of your practicum grade depends on your compliance with this assignment; thus, showing up late, not showing up, or complaining about your duties will result in a 10-point reduction per occurrence. These duties are extremely important for keeping a clean health care facility. Please help us take pride in our facility by keeping it clean. CLOSING DUTIES Daily Tasks Clean conference room. o Place chairs neatly around the table. o Clean the table surface with ‗Whizzer.‘ o Put books back in the shelves. o Hang up back packs, coats, etc., on the coat rack or place them out of the way (many meetings are scheduled for mornings here). Place items left in the training room by the athletes in the lost and found box by the front door (give more valuable items to Lynette to keep in her office). Clean the doctor‘s office waiting room. o Organize magazines o Throw away magazines three months or older, and those in poor condition Lock and close front and back doors, pharmacy door (top and bottom), doctor‘s office doors, xray room doors, secretary office doors, garage door, shop door, and storage door. Turn off the lights. TREATMENT AREA Daily Tasks Wipe down all treatment tables and pillows. o Spray on HDQ first. Let it sit on the surfaces for 10 minutes. o After 10 minutes, spray on Whizzer and wipe it off immediately. Organize pillows; distribute them evenly under the treatment tables. Organize hot packs in the appropriate places inside the hydrocollators. Fill hydrocollators with water to a level just to the top of the hot packs (do not overfill). Hang wet hydrocollator covers to dry. Put dry ones away. Follow the laundry schedule for the different sizes of covers. Empty the ice coolers. Dump the ice in the cold whirlpool or in the garage sink. Dry the coolers and open the lids to air dry. Organize the modality shelves. o Turn off all the modalities. o Place all electrode leads in the drawers. o Place all straps, compression sleeves, gel and lotion containers, etc. in the cabinet. o Seal all electrodes inside the plastic containers and place in the drawers. o Wipe down surfaces. Fill gel and lotion containers. Empty ‗Game Ready‘ ice compartments. 11 BYU Athletic Training Procedures and Appendix Weekly Tasks Clean modality cupboards with Whizzer. Clean one hydrocollator weekly on a rotating basis. o Drain and rinse out debris in the garage or the WP area. o Scrub inside surfaces and racks. o Inspect hot packs; discard them if they are damaged. o Clean outside with mineral oil. Annual Tasks Use wood cleaner or polish on wood surfaces. TAPING AREA Daily Tasks Clean all surfaces. o Spray on HDQ first. Let it sit on the surfaces for 10 minutes. o After 10 minutes, spray on Whizzer and wipe it off immediately. Restock the tape drawers and staff tape benches (see the posted chart for specifics). Organize and restock supply shelf (band-aids, etc.). Clean the area around the desk, table storing ice-wrap, file-cabinets, and mailboxes. Make lube pads. Place open boxes of tape in designated cupboards under the tape drawers; do not overstock – one open box each is enough. WHIRLPOOL AREA Daily Tasks Drain all whirlpools. Use HDQ to scrub out the inside of the whirlpool, rinse, and dry. Wipe down the seating areas. Cover the cold pool. Place the wet toe caps on the racks to dry. Empty any containers and set them against the wall to drain/ dry. Place any aquatic rehab items neatly on the shelves. Keep the top of the ice machine organized and clean. Weekly Tasks Use mineral oil to polish and clean the outside of the whirlpool. Annual Tasks Empty ice machine and clean thoroughly. Clean drying racks and white shelves. REHAB AREA Daily Tasks Turn off all machines. Wipe down appropriate surfaces (rehab machines, benches, etc.). o Spray on HDQ first. Let it sit on the surfaces for 10 minutes. o After 10 minutes, spray on Whizzer and wipe it off immediately.. o Do not use anything but water to clean the tracks on the elliptical machines; wipe these down with a moist towel. Put equipment away neatly. Take all tape off the floor. Organize shelves. 12 BYU Athletic Training Procedures and Appendix GARAGE AREA Daily Tasks Clean all coolers. o See cooler cleaning sheet for proper cleaning instructions. o Coolers with leftover PowerAde in them can be marked to save for the next day. They can be left out— but please keep them out of the way. o Each team is responsible to clean the coolers they used. However, if someone forgets, closers should go ahead and clean them. Clean the preparation cart (see the sheet for specifics). Clean the ice shovel and ice scoops with soap and water. Clean all appropriate surfaces (preparation surfaces, ice machine where we store ice scoops, etc.). o Spray on HDQ first. Let it sit on the surfaces for 10 minutes. o After 10 minutes, spray on Whizzer and wipe it off immediately. Park golf carts inside (appropriately space them so there is room to move around inside the garage) Park the Gem cart just outside the garage door and recharge it nightly. Clean golf and cooler carts (remove garbage, put things away, wipe down major spills, etc.). Sweep or squeegee water into drains. Sweep out leaves and debris blown in by the outside door. Weekly Tasks Clean ice machine filters. Clean out the cupboard above the sink. Leave the indoor storage door blocked open Monday evenings; call custodial and request they clean the floor the next morning. Annual Tasks Hose down and clean entire garage floor (including under the ice machine) Empty and thoroughly clean the inside of the ice machine. Clean racks. Wash cooler carts thoroughly. COOLER CLEANING Daily Tasks 1. Rinse the cooler and lid with hot water. Be especially thorough if the cooler had Gatorade in it. 2. Clean inside and outside of the coolers. 3. Squirt the cooler and lid with alcohol and scrub it. If it has stains, scrub it with 100% bleach. Rinse VERY WELL with water. 4. Wipe the cooler and lid dry with a clean towel. Dry both inside and outside. 5. Place the cooler upside down on the drying racks with the lid near it. Leave all coolers and ice chests open to air dry. 13 BYU Athletic Training Procedures and Appendix FILING MEDICAL RECORDS You must write down and record everything you do in the Athletic Training Clinic including evaluations, treatments, providing medication, or rehabilitation program changes. Keeping proper documentation serves many purposes. 1. 2. 3. 4. 5. 6. Medical records are legal documents that protect the athlete‘s and your rights. Medical records are a means of communication with other health care providers. Medical records are organized and provide a rationale for treatment (SOAP notes). Medical records provide quality assurance. Medical records can be utilized in research. Medical records help provide a basis for decisions such as discharge, progression, surgery, etc. BYU utilizes many different methods for documenting services including: 1. Blue Athletic Injury Record: Every athlete with an injury who receives treatment should have a blue Athletic Injury Record form filled out and utilized. The top portion should be filled out completely with a short history and evaluation. The left column is for recording treatment given, as specifically as possible. For example, writing ―US x 10 min‖ is not specific enough. Instead, ―US 1.5 w/cm 2 3 MHz over distal ITBand x 8 min‖ is better. The right column is for comments, including how the athlete feels that day, significant improvements or worsening, plans to change treatment the next visit, etc. If treatment notes in the blue sheet are reported as ‗unchanged‘ for over 1 week, a re-evaluation is in order. See Appendix G for the blue Athletic Injury Record form. 2. Report of Athletic Injury/Illness Form: This form is used to document a specific injury with a specific mechanism that happens during practice or an event. The white copy of the injury report form goes to the secretary, the yellow copy goes in the treatment file. The back of the yellow copy is used exactly the same as a blue treatment sheet (Appendix G). 3. Rehabilitation Record: An athlete injured significantly enough to miss practice for several days, or an athlete who is post-surgery will have a rehabilitation record. Utilize SOAP format with this form. 4. Daily Treatment Journal: Every treatment should be recorded on the log. It is an important back-up to the other sheets, and we use it to keep track of which modalities we utilize to justify purchasing new ones later. 14 BYU Athletic Training Procedures and Appendix General Recording Guidelines 1. Use ONLY black pen. 2. Be honest, even when you make a mistake. If you make a mistake DO NOT just scribble it out. Instead, put a single line through the mistake, write ‗error‘ above it, and initial the mistake. 3. Write legibly 4. Be as objective as possible. Listen to the athlete. DO NOT write down what you think the athlete is saying. Write down what they said. Do not interject your personal opinions. 5. Do not leave blank lines. If you use only part of a line, draw a horizontal line to the end of the line, sign your name and then get your ACI or staff ATC to approve and sign. 7. Preventative treatments consisting of singular ice bags, whirlpool, heat packs, stretching, or massage do not need a treatment sheet, but should be recorded on the log. However, if any of these are part of treatment for an injury, they should be recorded on a treatment sheet. Objectives for Team Physician Athletic Training Room Visits 1. Establish a professional relationship with the team physician. 2. Develop an awareness of the importance of communication with the team physician in the prevention, recognition, treatment, and rehabilitation of athletic injuries. 3. Develop communication skills with the team physician through professional dialogue. 4. Have an opportunity to confer with the physician regarding particular assessments in which pathology is uncertain. 5. Have an opportunity to view the team physician utilizing assessment and evaluation techniques. 6. Be introduced to any new physical assessment techniques by the physician. 7. Have the opportunity to ask questions regarding the anatomy and the body‘s physiologic response to the injury. 8. Have the opportunity to inquire about medication and/or electrical modality prescriptions. 9. Be able to ask questions relative to established and current surgical techniques used in the field of orthopedic medicine. 10. Utilize the team physician as a resource following surgical procedure(s) relative to development of rehabilitation protocols for the athlete. 11. The physician will see, by the ATC referral, athletes with injuries beyond the scope and limitations of athletic trainers. 15 BYU Athletic Training Procedures and Appendix Treatment Policy Home Events 1. Injuries incurred by BYU athletes during a BYU venue must be cared for by, and further assistance coordinated through, the athletic training staff. 2. In the absence of an athletic training staff member, the ATS may provide necessary first aid and initiate a primary injury evaluation. The injury occurrence will be communicated to a member of the athletic training staff and all further care will be coordinated through them. 3. If deemed appropriate or necessary, the injured athlete may be referred to the team physician(s) for further assessment. Referral to a team physician(s) must be approved by and coordinated through a staff ATC, and should NEVER be initiated by an ATS. Coaches should not refer an injured athlete for outside medical care prior to discussing the situation with a staff ATC. Except in the case of medical emergencies, coaches at BYU do not have the authority to make referrals to any physician(s) without consulting and receiving approval from a staff ATC. 4. If necessary, the team physician(s) will examine the injured student athlete and, as warranted, refer them to a medical specialist, order further diagnostic tests, and/or prescribe treatment for the injury. 5. If further diagnostic tests are required, the team physician(s) will make any necessary referral arrangements once the student-athlete has verified insurance stipulations and/or restrictions. It is the student-athletes‘ responsibility to understand the specific guidelines of their insurance policy. 6. All team physician(s) prescribed injury treatment and rehabilitation will, when possible, be carried out within the confines of the Athletic Training Clinic for in-season athletes. Out-of-season athletes will be referred to the University Health Center for treatment. 7. The athletic training staff may provide daily injury updates to individual coaches on all injured team members. The update will provide injury status, as well as any practice/game restrictions or modifications. 8. If the student athlete is not satisfied with his/her injury assessment, treatment or recovery, they should notify the staff ATC of their concerns. 9. If, during the course of the season, an athlete is injured and restricted from participation, he/she must be re-examined by the team physician(s) and/or staff ATC and given clearance to resume activity prior to doing so. Away Events 1. When practicing/competing away from BYU, most first aid services for the intercollegiate athletic teams may be provided by a BYU ATS (dependent upon personnel and facilities made available by the host institution.) 2. In the event an injury should occur and only a BYU ATS is present, the ATS must consult with the host medical and athletic training personnel for treatment and participation recommendations. 16 3. BYU Athletic Training Procedures and Appendix At no time should a coach ask an ATS for a decision regarding ‗return to play‘ of an injured athlete on the road. BYU ATS may share their findings from their preliminary first aid evaluation and, if warranted, recommend referral of the injured athlete to the emergency room. If an ATS is traveling unsupervised, it is the responsibility of the COACH for deciding whether an athlete can play or not. Coverage Policy of Non-BYU Student Athletes 1. If a visiting student-athlete is injured on the BYU‘s campus while participating in an intercollegiate sport activity, they will be afforded the same medical care as a BYU student-athlete. 2. If the visiting team has an ATC and/or team physician traveling with them, they will be allowed to handle the injury according to their procedures and policies. All BYU facilities will be placed at their disposal and they will be treated with the courtesy and respect due their position. 3. If a visiting team is traveling without an ATC or team physician, a member of the BYU athletic training staff and/or team physician will provide medical care and make appropriate recommendations to the student-athlete, coach, and ATS. 4. Visiting student-athletes, who are treated in the BYU Athletic Training Clinic, will be required to sign in and provide data for the treatment log. Transportation Policy of Injured BYU Student Athletes Life Threatening Injuries/Conditions If an athlete is injured during a practice or competition and requires immediate emergency medical attention, the Athletic Training Staff will activate the Emergency Medical System and provide any necessary preventative or maintenance care prior to EMS arrival. Dependent upon the personnel available and the extent of the injury, a member of the BYU Athletic Training staff may accompany the injured athlete to the hospital by ambulance. Non-Life Threatening (Emergency) Injuries/Conditions If an athlete in injured during a practice or competition and requires medical attention, the Athletic Training Staff will arrange transportation, whether by ambulance or protective services, for the injured athlete. Dependent upon the personnel available, and the extent of the injury, a member of the BYU Athletic Training staff or an athletic training student may accompany the injured athlete to the hospital or other medical facility. 17 BYU Athletic Training Procedures and Appendix Local Hospital Information Utah Valley Regional Medical Center 1034 N 500 W Provo, UT 801-357-7850 1 Mile from BYU HealthSouth Provo Surgical 585 N 500 W Provo, UT 801-375-0983 1 Mile from BYU Orem Community Hospital 331 N 400 W Orem, UT 801-224-4080 6 Miles from BYU Timpanogos Regional Hospital 750 W 800 N Orem, UT 801-714-6000 6 Miles from BYU 18 BYU Athletic Training Procedures and Appendix APPENDIX A OSHA Regulations for Exposure to Infectious Materials 19 BYU Athletic Training Procedures and Appendix EXPOSURE CONTROL POLICY FOR CONTROL OF INFECTIOUS DISEASES I. Job Classifications with Occupational Exposure at Brigham Young University. A. Physicians — general practitioner and orthopedic surgeons. Category I — direct contact with blood or other body fluids to which universal precautions apply. B. Athletic Trainers — staff & students. Category II — activity performed without blood exposure but exposure may occur in emergency. C. Laundry personnel Category III — task does not entail predictable or unpredictable exposure to blood. D. II. III. Exposure areas — training room facilities in the SFH, MC & Cougar Stadium, physician's offices in the SFH. Tasks Which May Result in Exposure in the Athletic Training Setting. A. Physicians 1. Aspiration of joint fluids — disposal of contaminated objects. 2. Injections — disposal of contaminated needles. 3. Suturing & care of open wounds, abrasions, weeping lesions, blisters. 4. Care of open fractures. 5. Care of infected areas where drainage is present. 6. Performance of CPR 7. Care of head injuries when drainage is present. 8. Performance of pelvic & genital exams. 9. Care of nose bleeds, dental & oral injuries. B. Athletic Trainers 1. Care of open wounds, weeping lesions, abrasions, blisters. 2. Care of open fractures. 3. Care of infected areas where drainage is present. 4. Performance of CPR. 5. Care of head injuries where drainage is present. 6. Care of nose bleeds, dental & oral injuries. 7. Cleaning & disposing of contaminated objects & surfaces. C. Laundry Personnel 1. Contact with contaminated laundry during cleaning. Prevention Policies A. Observe the concept of 'Universal Precautions' — all patients should be assumed to be infectious for HIV, HBV and other blood-borne pathogens in order to minimize exposure to infectious diseases. 1. Documented transmission of HIV & HBV occurs from: blood, amniotic fluid, pericardial fluid, peritoneal fluid, pleural fluid, synovial fluid, cerebrospinal fluid, semen, vaginal secretions, breast milk, or any body fluid visibly contaminated with blood. 20 BYU Athletic Training Procedures and Appendix 2. 3. No documented transmission of HIV & HBV from: sweat, tears, urine, feces, nasal secretions, sputum, saliva, and vomitus. When encountering body fluids under uncontrolled, emergency circumstances in which differentiation between fluid types is difficult, treat all body fluids as potentially hazardous. B. Hepatitis B Vaccination. 1. All employees whose jobs involve exposure to blood or other potentially infectious fluids should be vaccinated with Hepatitis B vaccine at the expense of the employer. 2. Any employee or student who declines to accept Hepatitis B vaccine must sign the statement in Appendix B. 3. If an employee or student initially declines the Hepatitis B vaccination, he/she may receive the vaccination at a later date. 4. Athletic training students are not defined as employees of the university; as a result, the university does not assume financial responsibility for student Hepatitis B vaccines. Students are given the option to receive the vaccine at minimal cost to them. If the student declines, he/she must sign the statement in Appendix B. C. Personal Protective Equipment. 1. The employer shall provide at no cost to the employee appropriate personal protective equipment: a. Gloves — should be worn when it is anticipated that there may be contact with blood, other potentially infectious materials, mucous membranes and non-intact skin; and when handling or touching contaminated items or surfaces. i. disposable gloves should be used and should not be washed or decontaminated for re-use. ii. gloves should be replaced as soon as possible when contaminated or if they are torn, punctured, or no longer serve as a protective barrier. iii. remove gloves as instructed. Always wash hands after removal of gloves. iv. utility gloves used for cleaning may be decontaminated for re-use if the integrity of the glove is not compromised. b. Masks, Eye Protection and Face Shields — should be worn whenever splashes, spray, splatter or droplets of blood or other potentially infectious materials may be generated and eye, nose or mouth contamination can be reasonably anticipated. c. Gowns, aprons, and other protective body clothing - appropriate is defined as but not limited to gowns, aprons, lab coats, clinic jackets. d. Resuscitation equipment - disposable airways, resuscitation bags, or pocket mouth-to-mouth resuscitation masks should be provided. e. All personal protective equipment should be removed prior to leaving the work area. f. When personal protective equipment is removed, it should be placed in appropriate biohazardous containers for disposal or cleaning. D. Hand washing. 1. Hands and other skin surfaces should be washed immediately and thoroughly, using liquid (not bar) soap, and warm water following: a. contamination with blood or other potentially infectious fluids b. cleaning of contaminated objects and surfaces c. removal of gloves. 21 BYU Athletic Training Procedures and Appendix 2. 3. Dry hands thoroughly with disposable paper towels. Apply lotion to keep hands from chapping if needed. Waterless antiseptic hand cleanser should be used if hand-washing facilities are not available. E. Cleaning & Disinfecting. 1. All spills of blood and blood-contaminated fluids & should be immediately cleaned up using a 1:10 solution of household bleach (see Appendix D) while wearing gloves. Visible material should be removed first using disposable towels; then the area should be decontaminated with the bleach solution. Hands should be washed following removal of gloves. Contaminated cleaning equipment should be cleaned and decontaminated or disposed of in biohazardous waste bags. a. contaminated carpet should be cleaned with the above bleach solution, followed by scrubbing the stained area with metaquat cleaner in the recommended dilution. 2. Biohazardous waste bags are located in each of the training room facilities and the physicians' offices. All soiled or contaminated disposable items (except sharps) should be placed in these red containers. a. the trainers will empty these containers when filled, wearing appropriate protective equipment. Biohazardous bags should be taken to room 917 WIDB for disposal. b. a red biohazardous plastic bag should be placed in kits where contamination of disposable items (gauze, bandages, etc.) is likely to occur (i.e., football field, gymnastics gym, wrestling, etc.) 3. All equipment, environmental and working surfaces shall be cleaned and decontaminated immediately following contact with blood or other potentially infectious wastes. Surfaces should also be decontaminated at the end of the work shift if surfaces may have been contaminated. 4. Broken glassware or sharp objects which may be contaminated should not be picked up directly with the hands. It should be cleaned up with a broom & dust pan, tongs or forceps. 5. All bins, cans, pails or receptacles intended for reuse which may become contaminated should be decontaminated on a regular basis, and immediately upon visible contamination. F. Contaminated Sharps, Needles, Scalpels. 1. Needles & scalpels should not be recapped, purposely bent or broken, removed from disposable syringes, or otherwise manipulated by hand. After use, sharp instruments should be placed in puncture-resistant, labeled sharps containers for disposal. These must be closeable and maintained in an upright position. 2. Sharps containers should be located as close as practical to the use area. 3. When filled, sharps containers will be transported to the BYU Health Center for disposal as per their established policy. 4. Reusable sharps (scissors, forceps, etc.) shall be disinfected by autoclaving before being used again. 5. When using sharps on road trips, a disposable sharps container should be part of the trainer‘s equipment. G. Laundry. 1. Soiled linen should be handled as little as possible and while wearing gloves. It should be bagged at the location where it was used. 22 BYU Athletic Training Procedures and Appendix 2. 3. H. IV. A special bag will be used for contaminated laundry that dissolves when in water. The container for contaminated laundry is labeled and will be located next to the laundry bag on the northeast side of the training room. Protective work clothing contaminated with blood or other body fluids should be placed and transported in bags or containers that prevent leakage. Persons handling such laundry should wear gloves. Protective clothing should be laundered according to the manufacturer's instructions. General Infection Control. 1. Eating, drinking, applying cosmetics or lip balm, and handling contact lenses are prohibited in work areas where there is a reasonable likelihood of occupational exposure. 2. Food & drink shall not be kept in refrigerators, freezers, shelves, cabinets, or on counter tops or bench tops where blood or other potentially infectious materials are present. 3. Mucous membranes that have come in contact with blood or other potentially infectious materials should be flushed with water immediately or as soon as feasible following such contact. An eye wash facility should be available. Exposure Procedures A. When any exposure is suspected as defined under the term 'exposure' in appendix A; the employee exposed shall immediately report the exposure to a full-time staff member. B. There will be immediate compliance with the following: 1. Immediate washing of contaminated skin with warm water and liquid soap for two (2) minutes. 2. Flushing or irrigation with water of contaminated mucous membranes. 3. Encourage spontaneous bleeding of lacerations or needle sticks for 20 seconds. 4. Completion of the Infectious Disease Exposure Form (See Appendix E). C. Post-exposure hepatitis prophylaxis can be made available if recommended by the U.S. Public Health Service. D. A post-exposure confidential medical examination will be available to the exposed employee or student. A completed copy of the Infectious Disease Exposure Form shall be given to the examining physician in addition to a copy of the Federal Register 'Occupational Exposure to Blood borne Pathogens, Final Rule', December 6, 1991. 1. The source individual's blood should be tested as soon as feasible and after consent is obtained to determine HIV and HBV status. If consent is not obtained, the employer should establish that legally required consent cannot be obtained. If the source is already known to be infected with HIV and HBV, testing need not be repeated. 2. Results of the source individual's testing shall be made available to the exposed employee or student. 3. The exposed employee's blood should be collected and tested as soon as possible with the employee's and/or student consent. a. If consent is not obtained, a sample should be drawn and retained for at least 90 days to be available for subsequent testing. 4. The report of the examining physician shall be provided to the employee or student by the employer within 15 days of the completion of the evaluation. a. The physician's written opinion for post-exposure evaluation and follow-up should be limited to: 23 BYU Athletic Training Procedures and Appendix i. ii. iii. iv. E. V. whether Hepatitis B vaccine is indicated for an employee or student that the employee or student has been told of medical conditions resulting from exposure to blood or other potentially infectious materials which require further evaluation and treatment That the employee or student has been informed of the results of the evaluation all other findings or diagnosis shall remain confidential and shall not be included in the written report. Medical Records 1. All records of an exposure incident should be maintained for the duration of employment plus 30 years after termination. These records should include: a. name and social security number of employee or student b. employee's or student's hepatitis B vaccine status including dates of vaccination or refusals to be vaccinated c. copy of all examinations, medical testing and follow-up procedures d. employer's copy of the physician's written opinion e. copy of the information provided to the health care professional f. a determination shall be made as to how future occurrences can be prevented. Information and Training A. All employees or students shall participate in an annual training program at no cost to the either. Annual training should be provided within one year of previous training. B. Employers shall provide additional training when changes in procedures or modification of tasks occurs. C. The training program shall contain the following elements: 1. Access to a copy of the Federal Register, Dec. 6, 1991, Vol. 56, No. 235, pg. 64175-64182 if requested. Copies will be permanently kept with the sports medicine secretary. 2. General explanation of the epidemiology and symptoms of blood borne diseases. 3. Explanation of the modes of transmission of Blood borne pathogens. 4. Explanation of the employer's exposure control plan. Copies of this plan can be obtained from the Sports medicine secretary. 5. Instruction on how to recognize tasks at risk for exposure to blood-borne diseases. 6. An explanation of the uses and limitations of methods that will prevent or reduce exposure including work practices, appropriate engineering controls, and personal protective equipment. 7. Information on the types, proper use, location, removal, handling, decontamination and disposal of personal protective equipment; and an explanation of the basis for selecting such equipment. 8. Information on Hepatitis B vaccine, including information on its efficiency, safety, method of administration, the benefits of being vaccinated, that it is free of charge to employees and available at cost to students. 9. Instructions on who to contact in the event of exposure and emergency procedures to follow after exposure occurs. 10. Explanation of the method of reporting the incident, medical follow-up available, and post-exposure evaluation provided by the employer. 11. Explanation of the signs, color codings and labels of containers of potentially infectious materials. 24 BYU Athletic Training Procedures and Appendix 12. An opportunity for questions and answers. D. Training Records — shall be maintained for 3 years from the date on which training occurred, and shall include the following information: 1. Dates of the training sessions. 2. Contents or a summary of the training sessions. 3. Names and qualifications of persons conducting the training. 4. Names and job titles of all persons attending the training sessions. E. The person conducting the training shall be knowledgeable in the subject matter as it relates to the work place that the training will address. 25 BYU Athletic Training Procedures and Appendix 26 BYU Athletic Training Procedures and Appendix APPENDIX B NATA Code of Ethics 27 BYU Athletic Training Procedures and Appendix National Athletic Trainers’ Association Code of Ethics Preamble The Code of Ethics of the National Athletic Trainers' Association has been written to make the membership aware of the principles of ethical behavior that should be followed in the practice of athletic training. The primary goal of the Code is the assurance of high quality health care. The Code presents aspirational standards of behavior that all members should strive to achieve. The principles cannot be expected to cover all specific situations that may be encountered by the practicing athletic trainer, but should be considered representative of the spirit with which athletic trainers should make decisions. The principles are written generally and the circumstances of a situation will determine the interpretation and application of a given principle and of the Code as a whole. Whenever there is a conflict between the Code and legality, the laws prevail. The guidelines set forth in this Code are subject to continual review and revision as the athletic training profession develops and changes. Principle 1: Members shall respect the rights, welfare and dignity of all individuals. 1.1 Members shall not discriminate against any legally protected class. 1.2 Members shall be committed to providing competent care consistent with both the requirements and the limitations of their profession. 1.3 Members shall preserve the confidentiality of privileged information and shall not release such information to a third party not involved in the patient's care unless the person consents to such release or release is permitted or required by law. Principle 2: Members shall comply with the laws and regulations governing the practice of athletic training. 2.1 Members shall comply with applicable local, state, and federal laws and institutional guidelines. 2.2 Members shall be familiar with and adhere to all National Athletic Trainers' Association guidelines and ethical standards. 2.3 Members are encouraged to report illegal or unethical practice pertaining to athletic training to the appropriate person or authority. 2.4 Members shall avoid substance abuse and, when necessary, seek rehabilitation for chemical dependency. Principle 3: Members shall accept responsibility for the exercise of sound judgment. 28 BYU Athletic Training Procedures and Appendix 3.1 Members shall not misrepresent in any manner, either directly or indirectly, their skills, training, professional credentials, identity or services. 3.2 Members shall provide only those services for which they are qualified via education and/or experience and by pertinent legal regulatory process. 3.3 Members shall provide services, make referrals, and seek compensation only for those services that are necessary. Principle 4: Members shall maintain and promote high standards in the provision of services. 4.1 Members shall recognize the need for continuing education and participate in various types of educational activities that enhance their skills and knowledge. 4.2 Members who have the responsibility for employing and evaluating the performance of other staff members shall fulfill such responsibility in a fair, considerate, and equitable manner, on the basis of clearly enunciated criteria. 4.3 Members who have the responsibility for evaluating the performance of employees, supervisees, or students, are encouraged to share evaluations with them and allow them the opportunity to respond to those evaluations. 4.4 Members shall educate those whom they supervise in the practice of athletic training with regard to the Code of Ethics and encourage their adherence to it. 4.5 Whenever possible, members are encouraged to participate and support others in the conduct and communication of research and educational activities that may contribute knowledge for improved patient care, patient or student education, and the growth of athletic training as a profession. 4.6 When members are researchers or educators, they are responsible for maintaining and promoting ethical conduct in research and educational activities. Principle 5: Members shall not engage in any form of conduct that constitutes a conflict of interest or that adversely reflects on the profession. 5.1 The private conduct of the member is a personal matter to the same degree as is any other person's except when such conduct compromises the fulfillment of professional responsibilities. 5.2 Members of the National Athletic Trainers' Association and others serving on the Association's committees or acting as consultants shall not use, directly or by implication, the Association's name or logo or their affiliation with the Association in the endorsement of products or services. 29 BYU Athletic Training Procedures and Appendix 5.3 Members shall not place financial gain above the welfare of the patient being treated and shall not participate in any arrangement that exploits the patient. 5.4 Members may seek remuneration for their services that is commensurate with their services and in compliance with applicable law. REPORTING OF ETHICS VIOLATIONS Anyone having information regarding allegations of ethical violations, and wishing to supply such information to NATA, shall supply this information, with as much specificity and documentation as possible, to NATA's Executive Director or Chair of the Ethics Committee. Information need not be supplied in writing, and the reporting individual need not identify him or herself. Information, however, that is too vague, cannot be substantiated without the assistance of the reporting person, or information where, in the opinion of the NATA Executive Director or Ethics Chair, there is no need for anonymity for the reporting individual will not be forwarded for action by the committee. An individual may report information on the condition that the individual's name or certain other facts be kept confidential. NATA may proceed with an investigation subject to such a condition; however, NATA must inform the reporting individual that at some point in the investigation NATA may determine that it cannot proceed further without disclosing some of the confidential information, either to the applicant or member under investigation or to some other party. A reporting individual, upon receiving this information from NATA, may decide whether or not to allow the information to be revealed. If the reporting individual decides that the necessary information must remain confidential, NATA may be required to close the unfinished investigation for lack of necessary information. Individuals are strongly encouraged to provide relevant information, with as much detail as possible, in writing to: NATA Ethics Investigations 2952 Stemmons Frwy Dallas, TX 75247-6196 Information available at www.nata.org 30 BYU Athletic Training Procedures and Appendix Job Descriptions Descriptions of all on- and off-campus Athletic Training clinical opportunities 31 BYU Athletic Training Procedures and Appendix Springville High School ACI – Lisa Walker Job Description: Students will be responsible for paperwork … enter information on athletes, fill out soap notes, treatment logs, etc. … (completed on SportsWare program). Open athletic training room (get it ready for athletes to come in) Close athletic training room (clean up from the days activities) Attend practice and games (home and away) Perform athletic training room treatments before and or after practice or games Expectations: Be back for two-a-days (fall) Stay to the end (spring, if they did not do two-a-days) Be available for home and away contests Be available by 2PM each day End of day time will vary from day to day (no definite stop time) Dress appropriately Call or text me with scheduling issues (occasional problems that may arise) When here, pay attention to what is going on here...avoid social texting and cell phone use Bring your favorite textbook to refer to when injuries arise. I will expect you to treat all athletes and sports equally. Perks of interning at SHS: Possible SHS apparel (depends on the coach) Little or NO weekend work In the high school we are not subject to the coaches demands We do NOT do water.... we just make sure someone else does. Great way to learn how to think critically and how to be independent. You will be great with legal issues and liability knowledge. During wrestling season you can make a little bit of money with wrestling tests. SHS is very positive toward the Sports Medicine staff. Great coaches to work with. Experiences/exposure unique to SHS I have been here for 17 years so the continuity of care and how things are done is tried and tested. I am open for new ideas and want BYU students to bring ideas. There is always room for improvement! You will learn about the NATA, RMATA and UATA organizations as you spend time here due to my leadership positions. 32 BYU Athletic Training Procedures and Appendix Pleasant Grove High School ACI – Kristin Pond Job Description: Assist in preparing athletes for practices and games, including taping, treatments, injury evaluations, and rehab. Prepare supplies for the day – stock med kits, ensure that water and bottles have been filled. Attend practices/games. Treatment and rehab following as needed. Assist with basic maintenance of the training room – cleaning tables, floors, stocking drawers, etc. Homework allowed as long as it doesn‘t require your entire attention (you should still be able to keep an eye on the athletes…) Expectations: I‘ve allotted Mondays for BYU AT students day off. I am pretty easy to schedule with (regarding evening classes and work schedules) but please know that I expect you to try and be here every day from 1-5:30, with the possibility of extended hours on game days. Coverage for practices and home games (with priority given to Varsity and high risk sports). The only team I consistently travel with is Varsity Football. Fall Semester: At the beginning of the year, we cover football, girl‘s soccer, girl‘s volleyball, girl‘s tennis and cross-country. I expect BYU ATS to be here for football 2-a-days, which usually start the first full week in August. Game schedule: Tuesday/Thursday – volleyball and soccer games, Thursday – JV/soph football games, Friday – Varsity football games. * Sports transition in November to boys and girls basketball and wrestling. Practice times are the basically the same, but games alternate Tu/Th and W/F for basketball with most wrestling matches on Wed. I also encourage students to become Assessors and help out with weight assessments for wrestlers (it‘s a great way to earn a few bucks!!) Winter (Spring) Semester: Students come to PGHS in the middle of basketball and wrestling season. (See * above). The state wrestling tournament happens in Feb. and I encourage my students to help out there as much as they can – it‘s a great opportunity to get a lot of hands on action! Sports transition in March to boy‘s soccer, boy‘s baseball, girl‘s softball, boy‘s tennis and track and field. Games are spread out throughout the week. Perks of interning at PGHS: We have an AWESOME, brand new Athletic Training Room – one of the largest in the state for a high school. Great athletes and coaches! Always something new – you get to see multiple sports, different levels, and a ton of hands on application of what you learn in the classroom! BYU Men’s Volleyball ACI – Blain Empey Job Description: Hours/Days: o Fall Semester—11:00 to 4:00 M-F starting the second week of school and finishing the last day of class. Thanksgiving week is off. o Winter Semester 2:00 to 7:00 PM, M-Th (practice) starting the first day of school finishing the last day of class. AT students are invited to remain through the end of the season (first weekend in May); however, this is not required nor expected. 4:00 to 10:00 PM, Friday/Saturday (games). o AT students cover pre-practice everyday; the senior student schedules a rotation of who leaves after practice begins. o AT students do not travel with this team. 33 BYU Athletic Training Procedures and Appendix o AT students cover needs of athletes who do not travel by arranging a few hours of availability on days while the rest of the team is gone. They stay in the AT room under the supervision of another ACI. Competition schedule: o Fall semester: The team will begin official off-season practices late October. This lasts four weeks through the first weekend of December (Thanksgiving week off). They host games/tournaments or travel each weekend during this time. o Winter semester: The team will compete at home or away every Friday and Saturday night. Occasionally, they will have a Thursday/Friday competition or compete mid-week. Responsibilities: o Senior students: Mentor first semester students in taping and modality ‗pass-off‘ (before they pass off to ACI). Train and supervise first semester students in mundane responsibilities such as drink preparation and clean up. Stock and maintain the ‗practice kit‘. Tape and provide treatment for athletes before and after practice, supervise athletes while doing established rehabilitation, accompany athletes to doc‘s office visits and report. Attend practice with ACI as first responders. Observe and perform evaluations and formulate treatment programs under ACI supervision. Manage coverage schedules. (Students rotate days off to limit hours to 20 per week). Manage records. o First semester students ‗Pass off‘ taping and modality use within 2 weeks. Manage mundane tasks (treatment logs, drink preparation, clean up). Observe evaluations and treatments. Provide treatments under direct supervision. Assist the senior student and ACI generally in all tasks. Expectations: AT students must learn athlete‘s names by the first week. AT students should have things prepared for practice early so they can assist/observe by the time the athletes arrive. They should keep watch for opportunities to learn and leave mundane tasks for later if those opportunities become available. AT students should plan on being in the AT room before practices every day. They will go out to practice to set up, and stick around until the coach makes announcements at the white board. They can then leave if it is their turn to have that day off. AT students can make themselves available to help with practices. This includes keeping score, shagging balls, and other non-athletic training responsibilities. I don‘t require this, but find that AT students who help out with these things find the athletes know them and trust them to a greater degree. Of course, medical needs take priority. Eating lunch, doing homework, using a cell phone, and those types of things are allowed when athletes don‘t need help. However, they should be done while sitting to the side and not in the front row. I want the athletes to see that you are interested in them and in their practice. AT students should never argue with coaches or players. This includes questionable officiating calls. AT students dress more formally for competition. For men, this means shirt and tie. For women, nice slacks and blouse (check with any female staff AT at BYU for details). Perks: Unfortunately, men‘s volleyball does not have the same budget as football. There are usually no tangible perks such as clothing, training table, etc. Experiences/exposure unique to men’s volleyball: Great competition with a low-profile team (compared to football and basketball) allows great student involvement without coaches having a ‗staff only‘ mentality about students working with athletes. The ACI is a physical therapist and has experience and perhaps a different perspective with rehab. Students have predicable hours with at least half of all weekends off. Although lower profile, games are usually well attended and exciting. 34 BYU Athletic Training Procedures and Appendix BYU Men’s Lacrosse ACI – Pete Webb Job Description: No commitment required before the first day of school Lacrosse practice runs from 7 – 9 am MWF. The athletic training room is open one half hour before and after Daily tape athletes and prepare to take water, injury ice, the AED Do treatments before and after practice Rehab and treatments are Tuesday and Thursday afternoon; typically 1-3:00 pm During the fall the team participates in a weekend tournament in Las Vegas to which a student is commonly ask to attend with the team Competition season is during Winter semester Home games are typically on Saturdays but the time of day varies Expectations: Students are invited and expected to travel with the team as much as possible The players are committed through mid May and so will a student working with lacrosse during the winter semester Perks: Early morning practice freeing up the remainder of the day for school and work; time on afternoons on Tuesday and Thursday is limited Traveling experience High risk and equipment intensive sport with unique challenges Opportunity to be creative in rehabilitation and other aspects of athletic training Experiences/exposure unique to Lacrosse: A wide range of athletic injuries Opportunity to stretch your evaluation, rehab and problem solving skills Fall and winter semesters are essentially the same with the addition of more competitions during winter semester 35 BYU Athletic Training Procedures and Appendix American Fork High School ACI – Becky Bailey Job Description: ATS assigned to AFHS will be involved in taping and rehabilitation of injured athletes. They will have daily opportunities to evaluate injured athletes and suggest treatment for their injuries as well as contribute to necessary referrals to other medical professionals. Students will also be involved in the daily operations of the training room such as record keeping (paper and computer), cleaning and maintenance of equipment. Athletic Training Students assigned to AFHS are expected to ―jump in‖ and be willing to learn and have initiative. Practice schedule: Training Room Hours: 1:00-5:30 every day that there aren‘t games. At AFHS we have athletics periods 4th period each day so practices start at 1:00. A good portion of treatments and taping occurs between 1:00 and 2:00. Other teams will show up to get taped/treated when school gets out at 2:15. On Monday afternoons we have district wide collaboration time that runs from 1:30-2:30. As a result student will not need to be to AFHS until 2:30 on Mondays. Games/matches: Games/matches may run late (9:00 pm or later for football, volleyball, basketball and wrestling) and I can‘t always predict what time we will leave the athletic training room. The time spent after a game is valuable in assessing injuries, establishing whether or not a referral is needed, and providing treatment after the heat of a game. If there are serious injuries, sometimes a trip to the hospital after a game to check on an athlete is required. Students are encouraged to participate in this if such an injury has occurred. We have an excellent hospital here in American Fork with a staff that generally is willing to answer many questions. These experiences can be an invaluable teaching/learning opportunity. o Students will be given a packet of the game schedules of each sport as each season starts. o During the fall sports (August-November), medical care is provided for all levels of football and the varsity games of all other sports. In the winter (November-March) and spring (February-May), medical care for games will only be provided for the varsity teams. Daily practice coverage is provided for all teams. Time off: ATS are generally given one day off a week to keep them under their 20-hour limit and to give them personal and study time. If there are 2 students assigned to AFHS, they generally alternate another day off, every other week, to meet the hour guidelines and allow for one-on-one time with me. I value peer-to-peer learning opportunities but also need one-on-one time to work on individual goals and levels of the student. Travel: AFHS is in a new region this year with schools from the Salt Lake Area. In general, travel will only be to varsity football games. I drive to all football games and students will ride with me in my car. I also travel to all state tournament games. Expectations: Initiative: One of the great things about the high school setting is the variety of injuries that you will get to evaluate and treat each day. I expect students to have initiative and to look for opportunities to learn and to help out. If I am evaluating an injury, doing a tape job or a treatment that you are not familiar with, I expect you to be by my side watching what I‘m doing and asking questions. You CANNOT be timid. The high school students will not trust you and they will wait in line for me to look at them if you don‘t have confidence in yourself. I do not expect you to know everything, but I do expect you to apply what you know and use it. I do not have the time to hold your hand and pamper you along. There is too much to do in this setting with too many athletes. Two-a-days: At AFHS our football, soccer and volleyball teams all run two-a-days. Soccer usually starts the last week of July and football and volleyball start the 1st or 2nd week of August. The start date differs from year to year so you will need to check with me to find out what the schedule will be that upcoming year. o You are expected to be at each session and be there the entire week. It is critical that you are there for 2-a-days, as it is a great time to start to get to know the athletes‘ names and personalities, which will aid you later in evaluations etc. At the end of the two-a-day week our football team always has a football scrimmage/dinner on Saturday night from 4:30-9:ish. You will be expected to be there too. Goals: I want all of the students that are assigned to AFHS to have goals for themselves. I want you to come to AFHS with specific things that you want to accomplish from that assignment. Studying while on assignment: I prefer that you not study while at your assignment. Each week you will be given one, if not two days off specifically for that purpose. I will try very hard not to waste your time and ask 36 BYU Athletic Training Procedures and Appendix that when you are on assignment at AFHS, that you not use that time for studying. There is rarely down time at the high school and if there is, I feel that we can better use it by working on the goals that you have set for yourself and practicing taping or evaluative skills, etc. If you feel that your time is being wasted, then you need to talk to me about it and you need to evaluate whether you are using your initiative to find opportunities. Time off: If a student needs time off from their assignment, they must talk to me in advance and ask for that time off, not just ―tell‖ me what they‘re doing and what days they‘ll be gone. The athletic training rotations should be treated just like an internship, paid or unpaid, and taking time off without prior discussion or notice could negatively affect your grade (evaluations) and any recommendations I might make on your behalf. It is simply not professional. Clothing and Appearance: At AFHS, we abide by the standards of the Athletic Training Program. While on assignment you should wear either your athletic training shirts or any school provided apparel. I do allow jeans to be worn at AFHS as long has they are nice (no holes), modest (no low-riders) and functional (too tight etc.) I also want shirts to be tucked in so that when you need to bend over an athlete, there aren‘t any issues from the backside viewing. Cell phones: Don‘t let cell phones interfere with your assignment. An occasional phone call or text is fine but incessant texting should not occur. FUN!!! If we‘re not having fun then we need to change something. There isn‘t a day that goes by, as stressful as they can get, that there isn‘t something fun we can laugh about and enjoy. Get to know the athletes personally. Talk to them while they‘re icing or having a treatment. These are the moments you can‘t get back. Perks: Variety: There is not a day that goes by that there isn‘t something new to see or something new to do at the high school. In any given season there are at least 3 different sports (6 in the spring) that are going on. At AFHS you‘ll get the opportunity to work with many different sports. View: As odd as it may sound, we have a great view of the Mt. Timpanogos temple from our campus and it has a calming effect on almost everyone. Also, if you have a goal to get to the temple weekly/monthly it is nearby and you can go to a session right after your assignment. Experiences/exposure unique to AFHS: Team Physician: We are very lucky during football season to have Mike Callahan, a local orthopedist as our team physician. His partner, Dr. Paul Ritchie also frequents our games and we are able to learn from their expertise. Dr. Callahan is trained in acupuncture and occasionally will treat our athletes with it for pain control and other ailments. We also have Dr. Dale Greenwood, a dentist, at those games as well. Large, fully equipped training room with various modalities and rehabilitation equipment. Modalities include: Solaris e-stim unit, ultrasound, light therapy, 3 whirlpools, hydrocollators, & cryotherapy State Championship Teams Established program (13 years) with a full-time teacher/athletic trainer; also former employment in a physical therapy clinic and a general medicine/sports medicine clinic. Working relationships with local orthopedic brace companies and sports medicine supply representatives 37 BYU Athletic Training Procedures and Appendix Timpanogos High School ACI – Jordan Hadlock Job Description: Athletic Training Students at Timpanogos will be treating athletes, taping, and observing practice or games every day, Monday through Friday. Most days consist of the hours of 2-6 PM for a normal practice day and games up to about 9 or 10 PM. Fall - In fall we have Football games on Friday‘s and other sports normally on Tuesday and Thursday. Student‘s do not need to report for fall camp, but are certainly welcome. They are expected when school begins. Winter – We have boys and girls basketball along with wrestling during the winter. This requires late games 3 to 4 nights a week. Practice schedules are the same as fall. Spring – Spring sports do not really have late nights because they do not have lights for most high school spring sports, practice schedules are the same. Time off – Students are free to take days off whenever they need them. Often games are the best learning chances for students to get real time action, so attendance on those days are encouraged. Expectations: Students are expected to perform evaluations and help with taping and getting athletes ready for practice and games whenever athletes need the help. Students can always study when there is down time. If students are there, I expect them to be willing to perform in game evaluations, so come ready to run. We rarely travel to away contests, so home games are the best opportunities to get live game time experience. Students are expected to look professional, but can wear whatever they want at THS. Perks: Because of the low profile of high school sports the environment is the biggest perk of Timpanogos High School. We are very relaxed and want you to learn without the stress of set hours and high profile settings. I cannot promise any clothes, but at least we have some great colors (blue and white) if that were to happen! Experiences/exposure unique to THS: One of the most unique and best things about this assignment is the fact that you will be able to perform in game evaluations. If the student is available they will probably be performing the evaluation, even in the games! I understand the limitations of other assignments, but at the High School we have an environment where some autonomy can start to develop. Like I said, come ready to run! 38 BYU Athletic Training Procedures and Appendix Cougarettes ACI – Krista Prusak Job Description: Hours/Days: o Fall Semester 2:00-7:00 pm M/W 3:00-7:00 pm T/TH 1:00-5:00 pm F starting the first week of school and finishing the last day of class. 7:00 am- 5:00 pm M-F Two-A-Day practices every day the two weeks before fall semester starts (the assigned student is invited to come but not required). May attend performances at Men‘s Basketball games, but there are most likely no sideline passes for the Football games. o Winter Semester 2:00-7:00 pm M/W 3:00-7:00 pm T/TH 1:00-5:00 pm F starting the first week of school and finishing the last day of class. AT students are invited to remain through the end of the season (Finals week and last week of April); however, this is not required nor expected. May attend performances at Men‘s Basketball Games Performances at the Covey Center for Arts in February o AT student cover pre-practice everyday. o AT students do not travel with this team. Competition schedule: o Fall semester: Cougarettes perform at every home Football and Men‘s Basketball game. AT student can attend the basketball games. Evening performances are possible at other venues (World of Dance, etc.). o Winter semester: The team will perform at all of the home Men‘s Basketball games. They perform their winter concert in February, which the student will attend, and prepare for nationals in April, which the student will not travel to. Responsibilities: o Drink preparation and clean up. o Stock and maintain the ‗practice kit‘. o Tape and provide treatment for athletes before and after practice, supervise athletes while doing established rehabilitation, accompany athletes to doc‘s office visits and report. o Attend practice without CI as first responders, when the CI is available. If not, stay in the AT room during practice to cover any injuries that may come and doctor‘s visits. o Observe and perform evaluations and formulate treatment programs under CI supervision. o Manage records. o ‗Pass off‘ taping and modality use within 2 weeks. Expectations: Learn athlete‘s names by the end of the first week. Have everything prepared for practice early so they can assist/observe by the time the athletes arrive. Keep watch for opportunities to learn and leave mundane tasks for later if those opportunities become available. Plan on being in the AT room before practices every day. They will go out to practice to set up. After Set-up if the CI cannot stay for practice the student may go back to the training room to study until the practice ends or the athletes leave practice for injury or a doctor‘s visit. Dress more formally for Men‘s Basketball performances and February concert. For men, this means shirt and tie. For women, nice slacks and blouse (check with any female staff AT at BYU for details). Perks: Unfortunately, Cougarettes does not have the same budget as football. There are usually no tangible perks such as clothing, food, etc. Experiences/exposure unique to Cougarettes: 7 time national championship winning team. Combination of jazz, ballet, modern dance and pom work. Because of the nature of the sport the body is trained differently than many other athletes and will provide the student with many opportunities to be creative with treatments and rehabilitation. Predictable hours with several game performances. Great opportunity to work with dance with the perk of the team unity rather than clinical feel. 39 BYU Athletic Training Procedures and Appendix Utah Valley University ACI – Megan Shaw Job Description: Fall- Main sport coverage will be UVU Women‘s Soccer and UVU Women‘s Basketball (starting in Nov) Spring- Main sport coverage will be UVU Women‘s Basketball and UVU Women‘s Softball (starting in March) Practice Day responsibilities: o Preparation of practice (water, Gatorade, ice chest, towels, etc). o Pre-practice treatment (stim, ultrasound, massage, stretching, taping/wrapping). o Assist ATC in injury evaluation and treatment. o Post practice clean up. o Post practice treatment (stim, ice, massage, stretching, etc). o Assist ATC in rehabs and all treatments of athletes Game Day responsibilities: o Pregame preparation (similar to practice, as well as set up work station on sidelines). o Greet opposing team‘s athletic trainer, inform them of our accommodations (water, ice, towels, doctor on site, etc). o Assist ATC in sideline injury evaluation and treatment. o Assist ATC in on field/court injury evaluation, help assist injured athlete off the field/court, assist in treatment of injury o Ensure athletes are staying hydrated o Postgame cleanup o Post game treatments o Assist ATC in rehabs and treatments throughout the day Expectations: Fall- Soccer 3-a-days start in August, be available for at least one practice a day Be available for all HOME games Studying is ok as long as all the athletes needs have been met. In-State away games-can help out if ATC is informed ahead of time Show Initiative Punctual Perks: Experience collegiate sports at a different level than BYU. UVU athletes are great to work with. Creativity comes out when working at our institution. We don‘t have a large budget so we find ways to make unique things work for our athletes. Experiences/exposure unique to UVU and Megan Shaw: Division 1 Athletics One ATC covering 3 sports… very busy ATC. There will be quite a lot of opportunities for the athletic training student to work one on one with athletes under the supervision of the ATC. Extensive opportunities to develop many athletic training skills such as: taping, modalities, massage, injury evaluation, and SOAP Note writing I‘m very easy going, if you need a day off I typically don‘t have a problem with it, just let me know in advance so I can make sure I have other help. If you have a job, we can work around it, please let me know in advance. 40 BYU Athletic Training Procedures and Appendix BYU Women’s Volleyball ACI – Gaye Merrill Fall semester: students need to be available from 2 p.m. to 7 p.m. during fall semester, practice time is 3:00 – 6:00 p.m. and is held on the main floor of the SFH. Practice begins the first part of August with 2-a-day practices, and the competitive season runs from the end of August through the first part of December. Students can travel (not required) to in-state matches, but will not travel to other matches. Any time the team is away on a road trip (usually alternate weeks), the students will have days off. Students will be expected to help provide coverage for home matches, starting at 4:30 p.m. and ending around 10 p.m. Duties are the usual: taping, treatment, rehabilitation, getting water, ice & PowerAde ready for practice, assist with clean up after practice. Expectations: Students must be able to come for the start of 2-adays and be available for all home contests (unless there are class conflicts). Students will go to practice and assist with duties as needed at practice. Winter Semester: Winter semester is the off-season for women‘s volleyball. The first 2 months (January and February) they cannot have team practice per NCAA rules, but do have individual skill instruction, starting at noon and going until 3 p.m. Team practice starts the end of February and ends the first part of April. During that time, practice is scheduled from 12:00 noon – 3:00 p.m., again on the main floor of the SFH. Students should have availability from 11 a.m. – 4 p.m. There is spring competition that does not count toward the team‘s overall record, usually lasting most of the day on several Saturdays in March and April. If it is in state, the students can travel (again, not required); if we are hosting a spring tournament, the students would be expected to help provide medical coverage. Duties: during individual drills, students will be located in the training room to provide treatment for players as they rotate in and out of practice. Generally students can rotate days of coverage during this time. Once team practice starts, students will be at practice every day the team practices. BYU Gymnastics ACI – Gaye Merrill Fall semester: Gymnastics has pre-season practice, no competition. Practice begins the second week of school, and is scheduled from 12:45 pm. – 4:30 p.m. in the gymnastics gym (149 SFH). Students should be available from 12 noon to 5:30 p.m. The team practices Monday, Tuesday, Thursday, Friday and some Saturday mornings (from 9 am – 12 noon); Wednesdays they‘re off. Treatment is held on Wednesday from 12 noon – 1 p.m. Because practice time is long, studying is allowed in the gymnastics gym during practice. Students are given one day off each week in addition to most of the day Wednesday. Duties are the usual: taping, treatment, rehabilitation, getting water, ice & PowerAde ready for practice, assist with clean up after practice. Expectations are that students would be available to assist with pre-season physicals the first week of school and start practice coverage the second week. Winter semester: competitive season begins the first part of January, with practice held during the same hours as fall semester. Meets are usually held on Friday nights, occasionally during other days of the week. Students can travel to most in-state meets (not required), but generally will not travel to other meets. Students will be expected to assist with home meets, starting at 4 p.m. and finishing around 9:30 p.m. Practice schedule varies according to the meet schedule, with more days off due to travel or to rest days. Students will usually still be given one day off per week if practical. BYU Women’s Tennis ACI – Chelsea Smith Job description: Pre-practice set up (which includes: 10 gal water, 10 gal PowerAde, ice chest (with ice bags and wrap), tennis kit, towels, tissues, cups, and water bottles) Pre-practice treatments (including: tapping, using appropriate modalities for managing/preventing injuries (ultrasound, electrical stimulation, heat/cold modalities, massage, etc.) Practice coverage (including: possible injury evaluation/treatment at practice, students are allowed to bring and do homework during this time) Post-practice treatment (same description as pre-practice treatment) Usually we don‘t have to clean up after practice, because we leave it out for Men's tennis practice Set up starts around 11:40 am, treatments from 11:45-12:15pm, practice from 12:30-2:45pm, break from 2:453:45 (while girls are lifting/conditioning in weight room), treatments from 3:45ish-4:20ish. 41 BYU Athletic Training Procedures and Appendix BYU Baseball ACI – Kaz Sakita Job description: Dealing with more upper extremity injuries and using hands-on-techniques such as PNF, shoulder stretch, and joint mobilization Learning and writing rehabilitation of upper extremity Improvement of decision-making skill Pre-treatment and field setup one hour before a practice and post-treatment one hour after a practice (only practice day) Pre-treatment and field setup 4 hours before a game and post-treatment one hour after a game (only game day) Practice will be at Miller Park and IPF in afternoon (1 - 5pm) During a season (from Feb to May), we will have 3-days (Thurs, Fri, & Sat) weekend series at least 5 times (I am expecting you to be there during the series) 42 BYU Athletic Training Procedures and Appendix UVU Track and Cross Country ACI – Spencer Mack Job Description: This assignment is specifically designed to give athletic training students experience working with track and field and cross-country athletes. Assignment schedules are usually Monday through Friday 12pm-6pm. We currently host one home cross-country race in the fall and will begin hosting track and field races in the spring upon completion of our track. At this time there is no opportunity to travel. Weekends are therefore almost all free. Fall assignments can expect to work primarily with cross-country from August to November. Track holds limited practices from October to December. In the spring Indoor Track starts the first week of January and goes into the month of March at which time outdoor track begins and continues into May or June depending on the championship scheduling. Expectations: Students assigned to cross-country and track and field will be expected to report in the fall during Physicals in August, or the first day of practice in January in the spring. This is a demanding position as there is one ATC for the team, which consists of over 100 athletes. Self-motivating students are a plus during busy peak treatment times. When the ATC is traveling, the students will be responsible for the treatments of the team members that remain at home under the supervision of the ACI in the athletic training room. This position does however offer lots of ―down time‖ which can be used to pass off assignments or work on homework. Perks: Lots of autonomy Because of the numbers of athletes seen on a daily basis, you will have the opportunity to perform evaluations, and set up treatments and rehabilitation based on the parameters you feel are appropriate and then approved by the ACI You will get to help make and define decisions with the ACI. You will get your hands dirty. Experiences/exposure unique to UVU and Spencer Mack: One of the major unique exposures that you will have is that even though you have been assigned to Cross Country/Track and Field, you will also gain experience with Wrestling, Baseball, Softball, and Women‘s Soccer, as well as helping with Doctor‘s Clinic and learn from the Chiropractor and Massage Therapist. They all work out of the same athletic training room, and because of our unique situation we will cover other sports as travel and needs dictate. It isn‘t all over use injuries and massage. It is also bloody wrestlers, broken bones, trashed knees, thrown out shoulders, major contusions etc. Bottom line is we have a ton of fun. We work like crazy at times (average 25-50 treatments per day) and we have fun and relax at others. BYU Football ACIs – Kevin Morris and Jeff Hurst Fall Semester Report Date: 1 week prior to fall practice beginning. Usually the last week of July, or first week of August Description of assignment: You will be assigned to work with a specific position group (linebackers, Oline, etc.). You will be required to follow that position during practice, have a fanny pack with supplies to assist players during practice. You will be able to evaluate injuries, and illnesses, under the direction, and supervision of an ATC, or your ACI according to your knowledge, and proficiencies. You will be assigned to do treatments, taping, and field setup daily by the Graduate Assistant over football, He/She will also assign you to be over a specific assignment such as records, knee braces, caddies, etc. You will be responsible for packing game trunks, field set up of Big Fogg Fans, you will serve as a host student athletic trainer for visiting teams, and work our sidelines at home games. 43 BYU Athletic Training Procedures and Appendix Hours: You will work 60+ hours a week during fall camp before school starts, but when classes begin you will be working around 20 hours/week excluding games, and travel. We will try to accommodate your schedule, but you should try to avoid scheduling classes after 1 p.m., or before 7 p.m. at night if at all possible. We understand that personal things will come up during the semester, and you may need to miss, but please understand that this may affect your travel opportunities. Perks: When assigned to work football there will be opportunities for travel to away games. We reward hard work, and dedication. We are limited to the number we can travel to 4, so this will be determined by the staff. If you work hard, and are here, you will be guaranteed to travel at least one game, of our choosing. Education: Football is a great opportunity to work with one of the nations top Division I football programs. You will be able to see severe injuries, observe surgeries, and work with one of the best Athletic Training Staffs in the country. If you work hard, and show dedication, we will write letters of recommendations for you if you apply for NFL internships, or after graduation for employment, or Graduate School. Winter Semester Report Date: First day of classes Description of assignment: You will be responsible for covering winter conditioning practices every afternoon, and covering treatments, and rehabilitation of injured, or post surgical athletes. During spring football practice you will be assigned to work with a specific position group (linebackers, Oline, etc.). You will be required to follow that position during practice, have a fanny pack with supplies to assist players during practice. You will be able to evaluate injuries, and illnesses, under the direction, and supervision of an ATC, or your ACI according to your knowledge, and proficiencies. You will be assigned to do treatments, taping, and field setup daily by the Graduate Assistant over football, He/She will also assign you to be over a specific assignment such as records, knee braces, caddies, etc. Hours: You will be working around 20 hours/week. We will try to accommodate your schedule, but you should try to avoid scheduling classes after 1 p.m., or before 7 p.m. at night if at all possible. Education/Perks: Football is a great opportunity to work with one of the nations top Division I football programs. You will be able to see severe injuries, observe surgeries, and work with one of the best Athletic Training Staffs in the country. If you work hard, and show dedication, we will write letters of recommendations for you if you apply for NFL internships, or after graduation for employment, or Graduate School. Orem High School ACI-Dujuan Shakespaere Job Description: Students will be responsible for paperwork. Enter information on athletes, fill out soap notes, treatment logs, etc. (SportsWare) Help athletes prepare for practices and games (taping, treatments, rehab) Attend practice and games (home and away) Assist in rehab program design Expectations: Be available for fall camp Be available for home and some away contests Most days we start at 2PM End of day time will vary from day to day (no definite stop time) Come ready to work – if you don‘t want to be here the kids will know Show initiative and desire Be creative – think outside the box Dress in appropriate athletic training attire Treat all athletes and sports equally Perks: 44 BYU Athletic Training Procedures and Appendix Good coaches that are easy to get along with Respectful athletes who appreciate you and your work Possible OHS apparel (depends on the coach) Little or NO weekend work We do NOT do water or ice – each team provides their own New athletic training room New school - Fall 2010 45 BYU Athletic Training Procedures and Appendix Utah Valley Sports Medicine ACI – Brent Rich Job Description: Intern will spend the semester experiencing the following: Observation of a physician‘s sports medicine clinic Teach exercise protocols (Jenn Frye and Lacey Lyman will teach our methods) Learn casting and splinting techniques Observe injections of various body parts Learn to call in patient prescriptions, refills and office paperwork Escort patient to doctors rooms Fitting braces and splints Organizing office supplies and maintenance of a physician office Assist in office procedures (musculoskeltal ultrasound, examinations, etc) Assist with office protocols (high school physicals, vital signs, height, weight, eye exam) Perks: Working with Utah Valley Sports Medicine!!! 46 BYU Athletic Training Procedures and Appendix APPENDIX C On-Campus BYU Emergency Action Plans 47 BYU Athletic Training Procedures and Appendix Emergency Procedure for MILLER PARK BASEBALL FIELD In case of an injury requiring the use of emergency medical services (EMS), the following procedures will be followed: 1. EMS will be activated using the telephone in the home team‘s dugout or by the ATCs cell phone. 2. An ATS will meet EMS at the gate to aid in brining the gurney onto the field to the injured athlete. The ambulance will stop at the fields edge. Ambulance will proceed east on University Parkway to the Field entrance on the third base side just prior to the 450 E. stoplight. Ambulance will pull down the concrete driveway to the field‘s edge. Prior to ambulance arrival, the following task must be performed: 1. Open gate along the sidewalk 2. Open gate to the field. Padlock to be unlocked prior to the game. 3. Move tarp out of the way. 48 BYU Athletic Training Procedures and Appendix Emergency Procedure for SOFTBALL Personnel 1. An ATC on staff will be present for all games. They will be seated n the dugout. 2. An ATS will be seated with the team in the dugout. 3. The host ATS will also sit in BYU‘s dugout but will be available tot eh other team for any of their needs. 4. An MD will be on call if not in attendance. 5. During practice, a ATS will always be present, while a ATC will either be present or will have contact with the student by radio or cell phone. 6. EMS will be summoned by calling 911. EMS is not usually present for practices or competition. Role of Personnel for Emergencies 1. The staff ATC will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will deter control to the person most qualified (e.g., MD, EMS) who is affiliated with BYU or summoned by BYU personnel. 2. If an injury occurs on the field, the staff ATC will attend to the athlete. One ATS will stand nearby and assist. One ATS will also be responsible for calls to EMS, directions to the site and retrieval of emergency equipment, as directed by the ATC. 3. If the visiting team brings a ATC, BYU personnel will assist as needed during any emergency. The host ATS will contact the BYU staff ATC to communicate any needs if there is not an obvious injury on the court. If the visiting team brings a student or does not bring any medical staff, the staff ATC will direct care. 4. During practices when a ATC is not present, the ATS will call EMS if necessary (or direct someone to do so) and initiate appropriate first aid. The ATS will contact the staff ATC as soon as possible thereafter. Location of Telephones 1. The staff ATC will have a cell phone at competitions. EMS should be requested via cell phone to ensure Provo EMS services are contacted. 2. If necessary, the nearest phone is located in the BYU locker room. The code for this door should be known to all athletic trainers working with softball. 3. If practice is held in the Indoor Practice Facility, the nearest phone is in the athletic training room. All athletic trainers working softball should know the code to enter this room. 4. Calling 911 from a BYU phone will contact BYU emergency services. The person calling should specifically point out that Provo EMS services are required for transportation. The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. Be sure that BYU EMS is not the only service sent, as BUY EMS has no ability to transport an injured athlete. Emergency Equipment 1. During practices, the emergency equipment is located in the underground storage on the BYU softball side of the stadium. This door should remain open during practice, but if it is locked, the staff ATC or the coaches all have a key. 2. During competition, the emergency equipment will be under the bench in the BYU dugout. 3. Emergency equipment includes: a. Spine Board & straps b. Cervical Collars c. Sam splints & Vacuum splints d. Crutches 49 BYU Athletic Training Procedures and Appendix e. AED 4. An AED is located in the training room during practices. Location for Arrival of EMS 1. Miller Park: EMS will be directed to enter from the back of the stadium on the road between Helaman Halls and the track. Pull into the stadium area and proceed west to the entrance between the seating and the bullpen. Back into this area, the ambulance will not fit through the fence. If transport on a spine board or stretcher are required, the gurney or the gator must be brought out on the field. The athlete will be secured to either and transported to the ambulance. A ATS will direct the ambulance from the parking lot of the stadium. Indoor Practice Facility: EMS will be directed to the northwest roll up door of the facility. The ambulance will enter through that door and go directly to the injured athlete. 50 BYU Athletic Training Procedures and Appendix Emergency Procedure for FOOTBALL I. Practice a. Phones Each staff member has a cell phone from which they can call 911 to activate EMS. The radios that we have are also able to activate EMS by turning the radio to channel 1H. This channel connects you directly to the University Police who can send EMS. Be sure to give you location, your name, and the extent of the injuries if known. Direct the ambulance to come to the East gate through which they may enter. Land based phones are located in the Athletic Training Room in the SAB (Room 123). The Head Football ATC and the Head Equipment Manager have keys to this gate in the event that they are locked. The ambulance can drive directly onto the field. b. Personnel An ATS will proceed to the East gate to wait for EMS to arrive, and direct them to the athlete. Other ATS should provide a large enough space for the treating ATC to work. They should keep athletes, media, and other non-essential personnel from interfering with the evaluation, and treatment of the injured athlete. II. Games a. GTA Responsibilities The GTA will be responsible for making sure all the emergency supplies (i.e., spine board bag, O2, air splints, crutch bag) are located at the 50 yard line of the home bench. b. EMS Liaison When the home team sideline is on the press box side, West side, a ATS will be assigned to have a radio, and be the EMS liaison. When the home team sideline is on the East side a host ATC will be given a radio and serve as the EMS liaison. The EMS liaison will accompany the staff ATC before the game to meet the EMS crew, and show them their seats at the North 20-yard line West Side. When an athlete is down the EMS liaison will position themselves on the 20 yard line and 5 yards on the field where they can see both the staff ATC and the EMS crew. If the staff ATC gives the emergency signal by circling their hand overhead the EMS liaison will notify the EMS crew personally. c. Ambulance Transportation In the event of a spinal cord injury, or a suspected spinal cord injury the ambulance crew and the ambulance will be brought on to the field directly to the location of the injured athlete. They will enter through the portal on the northwest corner of LaVell Edwards Stadium. Before the game, the ambulance will be situated in the turning lane of Canyon Road in front of LaVell Edwards Stadium on the west side. d. Medical Personnel The following medical personnel will be at each football game, whether at home, or away: Head ATC: Responsible for all medical personnel, and equipment on the sidelines. They are responsible for communication with the coaches, and the media. They are responsible for all on the field, and off the field injuries unless a physician has been asked to care for the athlete. They are also responsible for giving all signals to the 51 BYU Athletic Training Procedures and Appendix ATC assigned to receive them. The Head ATC is responsible for C-spine stabilization during care for an injured athlete, and giving directions to all involved in that situation. They will designate an ATC to assist them in removing the face mask. Team Orthopedist: The team Orthopedist is responsible for al musculoskeletal injuries occurring during the game. When asked to evaluate an injury by the Head Football ATC, the Team Orthopedist will determine return to play, X-Ray, and any other medical procedures required for the benefit of the athlete. They may ask the Team Physician for assistance with these duties when they feel it is necessary, or the Team Orthopedist is not available. Team Physician: The Team Physician is responsible for all illnesses, concussions, lacerations, or other non-musculoskeletal injuries occurring on the field, or during the game. They will administer medications, IV‘s, and any other medical procedure not covered by the Team Orthopedist. They may ask assistance from the Team Orthopedist in the care of athletes if needed. Team Chiropractor: The Team Chiropractor will be responsible for spinal mobilization, acupuncture, and other chiropractic services before, and after the game to athletes. If asked by the Team Orthopedist or Team Physician they may assist in the care of athlete injuries during the game. e. Game Day Signals The Head Football ATC and a staff ATC proceed on to the field when an athlete is injured. They may signal to the staff ATC designated to watch for these signals. However, ATS‘s should also watch so that they can assist when necessary. Each ATS must know the following signals and their meaning. The signals can be found on the following pages. 52 BYU Athletic Training Procedures and Appendix FOOTBALL SIGNALS AND COMMANDS Command Signal 1.Assistance for removal of an injured athlete from off the field. 1. Hand placed forward with a number of fingers raised designating how many people are needed to help (usually two). The designated athletic trainer on the sidelines will watch and choose two appropriate sized people. For example, two fingers raised for a 6'6" three hundred pound offensive lineman will require two large football players, not two small managers. 2. Several large circles made with the arm overhead. 3. Thumb to ear, fifth finger to mouth, other fingers flexed, as if making a telephone call. 4. Hand placed palm down on top of the head. 6.Trainer's bag to be brought to the field. 5. Signal for the doctor followed by the signal for a bag (shoulder abducted at 90 degrees, elbow bent, hand down in a fist, as if carrying a bag). 7.Stretcher and assistance. 6. 8.Cervical collar to be brought to the field. Hand placed on chest followed by the signal for a bag, as above. 7. 10.Tape or wrap to be brought to the field. Arm to the side with the elbow bent and forming a square in front of the body with the palm up. This is followed by the hand in front with a number of fingers raised indicating the number of people needed for assistance. Again, the designated athletic trainer should note the size of the athlete to be transported. 8. Hand cupped forming a C followed by grabbing the throat. 11.Ice bag needed. 9. Index finger hooked and placed in the mouth on the lower jaw, mouth open. 12.X-rays needed. 10. Hands held in front, one or two fingers extended, hands rolling around each other. Body part to be taped is pointed to. 2.Paramedics needed for a life threatening emergency. 3.Call 911. 4.Doctor to come to the field. 5.Doctor's bag to be brought to the field. 9.Airway to be brought to the field. 13.Sports chair to be brought to the field. 14.Athlete is cramping. 11. Both hands cupped, forming a snowball with each other. Plastic wrap or ace is also needed. 12. Forearms crossed in front of face. 13. Same sign as for a stretcher, followed by one hand making a rolling motion (like a wheel) at the side. 14. Shake fist, point to the body part affected. 53 BYU Athletic Training Procedures and Appendix Emergency Procedure for GYMNASTICS Gymnastics is a high risk sport for injury. Athletic training students must be prepared to handle emergency situations and be competent in the evaluation and emergency care of injuries that occur. I. Practice procedures The practice facility is located in room 147 SFH. Athletic training students should be familiar with the following: A. Location of the nearest phone - the nearest telephones to make an emergency phone call would be: 1. Cell phones which can be used to dial '911.' 2. Upstairs in the student weight room (293 SFH). Dial either '911' or '2-2222'; both calls will go to campus security when dialed from a BYU phone. 3. Athletic department weight room — located at the north end of the hall from the gymnastics gym. B. Most accessible location for ambulance transport is through the south doors of the gymnastics gym. Dispatchers should be told to have the ambulance drive up on the sidewalk between the indoor tennis courts and south side of the Smith Fieldhouse. C. Emergency equipment—vacuum splints, cervical collars and spine boards are located in the storage room of the main athletic training facility in the SFH and in the gymnastics gym at the southwest corner. Athletic training students should be familiar with their location so that they can find them quickly when needed. D. Special considerations: 1. Emergency transport of a gymnast who is lying in the foam pit involves unique circumstances. The foam is unstable, which may cause unwanted movement of the athlete, and makes it difficult for rescuers to get good footing. Prior practice of this skill is needed before attempting it in an emergency situation. 2. Be aware that the 4" and 8" foam mats are very soft, and can cause unwanted movement of the athlete if the rescuer approaches it too quickly. Take slow deliberate steps when approaching a gymnast who is lying on one of these mats. E. Medical Personnel—physicians and EMS are on call for practice. An ATC should be in the gymnastics gym at all times. II. Meet procedures Gymnastics meets are held on the main basketball floor of the SFH or in the Marriott Center. A. Location of nearest phone — the staff athletic trainer in charge of the event should have a cellular phone available on the competition floor. The women's gymnastics team coaches also have cellular phones. In the SFH, the courtesy telephone is located next to the exit doors on the northeast end of the indoor track. In the Marriott Center, the closest permanent phone is in the athletic training room. B. Most accessible location for ambulance transport: 1. From main floor of SFH—the main entrance on the north side of the building. 54 BYU Athletic Training Procedures and Appendix 2. From Marriott Center—the north side of the building (ticket office entrance). C. Emergency equipment 1. For meets in the SFH, emergency equipment is brought down out of the storage room on the south side of the indoor track. This equipment should include: cervical collars, vacuum splints, and crutches. The equipment is placed behind the curtains drawn on the west side of the competition floor. The AED should be brought from the athletic training room and placed in the same location. 2. For meets in the Marriott Center, emergency equipment will be left in the athletic training room due to its close proximity to the competition floor. Athletic training students should check the equipment the day prior to the meet to make sure proper sizes of equipment are available. ). D. A certified athletic training and a physician will be present for all meets. The ambulance is on call. 1. In case an ambulance is needed, an ATS will be designated to open the roll up door in the west side of the Marriott Center and direct the ambulance to the playing floor level. 2. A second ATS will be designated to bring the bag with emergency equipment on to the floor. 55 BYU Athletic Training Procedures and Appendix Emergency Procedure for TENNIS Outdoor Courts The nearest phone is located in the building as you walk into the tennis complex. This phone can be used to dial 911. If for some reason that phone is not in operation the next closest phone is inside the field house. As you walk in the field house from the tennis courts, the phone is located on the left hand side of the hallway in a public phone booth. This phone could also be used to dial 911. Direct the ambulance through the east gates of the tennis complex for any emergencies. Directions to the ambulance will be to go to the south parking lot and drive up the sidewalk to the main entrance. Indoor Courts The nearest phone is located in the indoor tennis office near the east doors of the building. This phone should be used to call 911. If this phone is inoperable the same phone as described above should be used inside the field house. Direct the ambulance through the northwest doors as the other entrances may be less convenient. Notes it is always advisable to familiarize yourself with the surroundings and locating the nearest phone as phone hook-ups may change. it is also advisable for one of the trainers to stay with the injured athlete until help arrives while the other trainer, coach, or player goes to meet the emergency vehicle responding to the call. This should be either at the gates of the outdoor tennis complex or at the doors of the indoor building. This will help the emergency response team to locate the athlete in need. 56 BYU Athletic Training Procedures and Appendix Emergency Procedure for SOCCER The Head ATC will normally be located on or behind team bench and will go onto the field for all injuries. The First Assistant will stay near the head trainer and go onto the field to assist the head trainer with the injury and transportation of the athlete off of the field. Also, he/she will assume the head trainer role on sideline if the head trainer is attending to other duties. The first assistant is responsible for calling EMS and will stay on the phone until they arrive, and will go with the athlete to the hospital. The Second Assistant is the courtesy athletic trainer and is responsible for making sure the visiting team has everything they need and will assist them with any injuries that might occur during the game. He/she is responsible for meeting and directing the ambulance. Also, he/she will retrieve any medical equipment or supplies needed on the field or sideline. Team physician and orthopedic physician will be on call. Emergency equipment located on site: 1. 2. 3. 4. 5. 6. Spine board Vacuum mattress Vacuum splints Sports chair Crutches Cellular phone 7. 8. 9. 10. 11. 12. Two radios Evaluation table OSHA kit CPR mask Air way Cart for transportation Emergency procedure to be followed If a player goes down on the field, the head athletic trainer and the first assistant will go onto the field to attend to the athlete. The second assistant will step on to the field to retrieve the signals for any needed equipment. In addition, he/she will be ready to assist in transporting the athlete off of the field or finding players to help carry the athlete from the field. If an ambulance is needed, the first assistant will contact EMS by using the head trainer's cellular phone and will stay on the phone with EMS until the ambulance arrives or until instructed to hang up. The ambulance will enter the field using the northwest gate. The second assistant will contact PE services to open the gate and clear the area as well as meet the ambulance and crew. The first assistant will go with the athlete to the hospital and will communicate with the head athletic trainer by radio. The head athletic trainer will be responsible for informing and communicating with the team physician or the team orthopedic physician as necessary. Procedures for practice During practice all procedures will remain the same except it will be the athletic training students who will assist the injured athlete and contact the head athletic trainer by radio if he/she is not on the field. The EMS will be contacted through the athletic training room or by cellular phone. The ambulance will enter Haws field using the northwest gate and will be opened by the key located in the athletic training kit. 57 BYU Athletic Training Procedures and Appendix Emergency Procedure for SWIMMING & DIVING Personnel A certified athletic trainer will be present for all swim/dive meets. He/she will be present on deck west of the area between the competition pool and the dive tank. An athletic training student is also usually present. Athletic trainers are not usually present for practices. Lifeguards are present near the station of their choice for both competitions and practices (usually at three separate stations during competitions: west, south, and northeast sides of Pool C). BYU coaches are trained in water safety and extrication and are qualified for inclusion in this list. They are, of course, present at all meets and most practices. Physicians are usually on call, but if present will be with the athletic trainers. Role of personnel for emergencies The certified athletic trainer will direct care and designate responsibilities for athletes injured while competing in the meet. If an athlete requires extrication from the pool, the certified athletic trainer‘s responsibility will begin after the athlete is extricated. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS) who is affiliated with BYU or summoned by BYU personnel. Lifeguards are responsible for extricating any injured athlete out of the water, and firstaid for non athletes. Whenever an athletic trainer is not present (as is the case normally during practices) lifeguards are responsible for emergencies. If there is an emergency, the lifeguard should call the athletic trainer after EMS is contacted and treatment is initiated. Lifeguards will refer athletes with nonemergency injuries to the athletic trainers. Coaches trained in water safety are present to assist the lifeguards as needed. If EMS is required, the staff athletic trainer will call by cell phone or direct someone to call. The athletic training student at the pool will stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. If the visiting team brings a certified athletic trainer or an athletic training student, BYU personnel will assist as needed during any emergency. If the visiting team does not bring any medical personnel, BYU‘s staff athletic trainer will direct care. Location of telephones The staff athletic trainer will have a cell phone at competitions. EMS should be requested via cell phone to ensure Provo EMS services are contacted. If necessary, the nearest telephone is located outside the lifeguard office near the 5 meter platform ladder. Telephones are also located inside the lifeguard office. Calling 911 from a BYU phone will contact BYU emergency services. The person calling from a BYU phone should specifically point out that Provo EMS services are required for transportation. The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. Be sure that BYU EMS is not the only service sent, as BYU EMS has no ability to transport an injured athlete. 58 BYU Athletic Training Procedures and Appendix Emergency equipment The pool spine boards are designed for use in extrication as well as stabilizing a suspected spine injury. These are located at the pool behind the 5 meter platform stairs near the lifeguard office. Lifeguards are responsible for spine boards. Sam splints, vacuum splints, crutches, and oxygen will be present at meets, and can be brought from the athletic training room for practices. The athletic trainers are responsible for this equipment. An AED will be brought for competition with the above. An AED can be used at the pool; AEDs may be used in "casual water". For a swimming pool environment, this means that the victim may be sweaty or wet or the deck where the body is lying may be wet and there is no danger. However, the guidelines recommend that, if possible, water is removed as quickly as is reasonably possible without delaying the AED procedure. At our facility, with so many towels readily available, this shouldn't be a problem. In real life situations, the victim will have most likely been removed on a spinal board (ours are fortunately wood) and the AED would be applied while the victim is still secured to the board. Location for arrival of EMS The pool entrance is an unmarked door on the west side of the RB. This door is locked from the outside, so someone will need to stand by to open the door when EMS arrives, or it must remain open. The athletic training student, a coach, or a lifeguard will open the door, watch for the ambulance, and direct EMS to the injured athlete. 59 BYU Athletic Training Procedures and Appendix Emergency Procedure for MEN’S & WOMEN’S BASKETBALL Phone: Located in the Marriott Center athletic training room (422-2955). A phone is also located at court side, which may be used in an emergency situation. The staff athletic trainer will have a cellular phone available as well. EMS can be activated by dialing 911 directly from any of the above phones. EMS coverage: During games, an ambulance will be on site. They will be available to transport injuries and assist in any critically injured athlete. The ambulance will enter through the west tunnel into the flat portion of the Marriott Center where they may park. 60 BYU Athletic Training Procedures and Appendix Emergency Procedure for VOLLEYBALL Personnel A certified athletic trainer on staff will be present for all matches. They will be seated with the team or directly behind the team on the first row in the audience. An athletic training student will be seated with the team. Another athletic training student will act as ‗host trainer‘ and will sit behind the visiting team on the first row of seats in the audience. An MD will be seated in the audience or will be on call. During practice, a athletic training student will always be present, while a certified athletic trainer will either be present or will have contact with the student by radio or cell phone. EMS will be summoned by calling 911. EMS is not usually present for practices or competition. Role of personnel for emergencies The staff athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS) who is affiliated with BYU or summoned by BYU personnel. If an injury occurs on the court, the staff athletic trainer will attend to the athlete. The athletic training student on the side of the injury will stand nearby and assist. If EMS is required, the staff athletic trainer will call by cell phone or direct someone to call. The staff athletic trainer will direct the athletic training student to get the MD if needed. The MD will come to the court and stand by or assist if their help is needed or requested. The athletic training student on the court opposite of the injury will stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. If the visiting team brings a certified athletic trainer, BYU personnel will assist as needed during any emergency. The host athletic training student will contact the BYU staff athletic trainer to communicate any needs if there is not an obvious injury on the court. If the visiting team brings a student or does not bring any medical staff, the staff athletic trainer will direct care. During practices when a certified athletic trainer is not present, the athletic training student will call EMS if necessary (or direct someone to do so) and initiate appropriate first aid. The student will contact the staff athletic trainer as soon as possible thereafter. Location of telephones The staff athletic trainer will have a cell phone at competitions. EMS should be requested via cell phone to ensure Prove EMS services are contacted. If necessary, the nearest telephone is located in 60 SFH near the main entrance where tickets are taken (the women‘s volleyball coaches‘ offices). If that door is locked, the code to open the door is 268456. A courtesy telephone is also located in the hallway near 6 SFH. If practice is moved to the RB, telephones are located in many offices adjacent to the several gyms; many of these offices are open after normal business hours: o Health and Human Performance Services, 146A RB o Lifeguards office, 147E RB. o Human Performance Resource Center, 112A RB. o Intramural activities, 145 RB. o Custodial office, 142 RB. o The men‘s and women‘s locker rooms. 61 BYU Athletic Training Procedures and Appendix o Two courtesy phones are located in the RB. One is in the hall between the men‘s locker room and the Y-Be Fit office and another is located at the northernmost end of the hall. Calling 911 from a BYU phone will contact BYU emergency services. The person calling should specifically point out that Provo EMS services are required for transportation. The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. Be sure that BYU EMS is not the only service sent, as BYU EMS has no ability to transport an injured athlete. Emergency equipment Emergency equipment is located in the upstairs cage in the storage area attached to the indoor track on the south side. The combination to that lock is 2–16–10. Some emergency equipment is stored in the SFH training room storage (marked with an asterisk*). Equipment includes o One tall/large spine board o Appropriate straps and restraints for the spine board o Cervical collars o Sam splints, vacuum splints o Crutches o *AED o *Oxygen During competition, the emergency equipment will be placed outside the court exit on the south side. The AED will be placed by the team chairs on the north side. An AED is located in the training room during practices. Location for arrival of EMS SFH: Main entrance, north side of the building. RB: Entrance at the southwest of building. Both locations are accessible without needing keys, etc. Special equipment or other considerations Besides the tall spine board appropriate for many volleyball players, no special equipment is necessary. 62 BYU Athletic Training Procedures and Appendix Emergency Procedure for CLARENCE ROBISON TRACK In case of an emergency requiring the use of EMS, the following procedures will be followed: 1. EMS will be activated using the ATC cell phone. There is no permanent phone located at the outdoor track. 2. ATS‘s will meet EMS at the South entrance and direct them to pull up the driveway, and if necessary, drive the ambulance onto the track to the athletes‘ location. The ATS‘s will aid in bringing the gurney onto the track to the injured athlete. Personnel An ATC will be present at all home meets. They will be on the infield near the Southwest turn on the track during the meet. The ATC will be available 2 hours prior to the beginning of the meet and will stay until the last even is over and all athletes are seen or treated in the training room. ATS‘s will be located on various parts of the infield during the meet. They will be in contact with the ATC via radios or cell phones. We will have one student in the athletic training room at the track at all times. Physicians are on call during track meets, but if present, will be either seated in the west bleachers, or standing with the ATC on the infield. The ATC will contact the physician if the need arises. Role of Personnel The ATC will direct all care and designate responsibilities for all injured athletes while competing in the track meet. All care will be the responsibility of the ATC until the Provo EMS or the BYU team physician arrives. All injuries on the track will be evaluated by the ATC with the ATS being called upon as needed. Anyone dealing with the emergency situation will defer control to the person most qualified (e.g., physician or EMS) who is affiliated with BYU or summoned by BYU personnel. The team physician (if needed) will be called by the ATC. If the team physician is present at the meet, they will be called upon for assistance by the ATC. ATS‘s will be called upon to help with the situation as needed. They will meet the ambulance at the South entrance of the track and direct them to the injured athlete. If visiting teams bring an ATC or an ATS, BYU personnel will assist as needed during the meet and during an emergency. If no medical personnel are present for visiting teams, BYU personnel will direct care. Emergency Equipment All emergency equipment (i.e., spine board, AED, air splints, etc.) will be located on the infield on the Southwest turn next to the Powerade cart and water station. Location of Arrival for EMS Ambulance will proceed North on Canyon Road (150 East) to the stoplight just after the Helaman Halls parking lots (approximately 1400 North). The ambulance will turn right and enter the driveway leading to the south end of the track complex. The following will be done prior to ambulance arrival: 63 BYU Athletic Training Procedures and Appendix 1. 2. 3. 4. Open padlock at the south end of the track Slide fence open in order to allow for ambulance entrance ATS at the south entrance will direct ambulance Spectators and athletes must stay clear to allow EMS passage. All transports will be taken to Utah Valley Regional Medical Center (UVRMC) unless determined otherwise by attending paramedics. The team physician will be notified of all athletes being transported to the hospital facilities for care. 64 BYU Athletic Training Procedures and Appendix Emergency Procedure for DANCE The emergency action plan for the BYU dance athletic training room is: 1. Activate EMS a. Call 911 2. Provide EMS with the following information: a. Exact location of the injured athlete b. Nature of the injury c. Other information as requested by the emergency response team 3. Provide appropriate emergency care until EMS arrives 4. Document the emergency When the emergency action plan is activated, personnel over the dance department must be notified and given the sport/dance team of the athlete involved and the nature of the injury. The decision to activate the emergency action plan should be made by the ATC on the scene, not by a coach, or by-stander. The ATC on the scene will remain in charge until EMS arrives. All other persons 1. Injuries seen by an ATC to non-Dance Department students and faculty/staff must be recorded in the appropriate injury reporting system. For these people, an injury that must be recorded is defined as ―an injury (acute or chronic) that causes a person to report to the athletic training room except non-infectious abrasions or blisters.‖ Emergency Procedures for the 4 Dance Facilities 1. Athletic Training Room a. Assess ABC‘s and other life threatening injuries b. Assign someone to call 911 (indicate to emergency personnel to come to the north door of the athletic training room in the Richards Building) c. Assign someone to meet emergency personnel in the parking lot and direct them in. d. Continue to assess and monitor the patient, beginning CPR if needed, until emergency personnel arrive. 2. Richard‘s Building Studio a. Assess ABC‘s and other threatening injuries b. Assign someone to call 911 (indicate to emergency personnel to come to the northwest door of the Richard‘s Building) c. Assign someone to meet emergency personnel in the northwest parking lot and direct them in. d. Continue to assess and monitor the patient, beginning CPR if needed, until emergency personnel arrive. 3. Harris Fine Arts Center a. Assess ABC‘s and other life threatening injuries. b. Assign someone to call 911 (indicate to emergency personnel to come to the tunnel entering the west side of the HFAC) c. Assign someone to meet emergency personnel in the parking lot at the top of the tunnel and direct them in. d. Assign someone to notify the company director. e. Continue to assess and monitor the patient, beginning CPR if needed, until emergency personnel arrive. 4. Marriott Center 65 BYU Athletic Training Procedures and Appendix a. Assess ABC‘s and other life threatening injuries. b. Assign someone to call 911 (indicate to emergency personnel to come to the tunnel entering the west side of the Marriot Center) c. Assign someone to meet emergency personnel in the parking lot at the top of the tunnel and direct them in. d. Assign someone to notify the company director. e. Continue to assess and monitor the patient, beginning CPR if needed, until emergency personnel arrive. 66 BYU Athletic Training Procedures and Appendix Emergency Procedure for EXTRAMURAL SPORTS Lacrosse, Rugby, and Soccer Practice Haws Field, RB Turf, Indoor Practice Facility, and Helaman Field Personnel ● Staff ATC A certified athletic trainer on staff will be present for all practices and games. ● Athletic training student A athletic training student may or may not be present at a practice or a game. ● Coaches Head Coach Assistant Coaches ● EMS EMS will be activated by calling 911. EMS is not usually present at practices or games. Role of Personnel During Emergency ● Staff ATC The staff athletic trainer will direct care and designate responsibilities during an emergency. If EMS is required, the staff athletic trainer will direct someone to call. The ATC will defer control to someone who is more qualified (physician or Provo EMS) when he/she feels comfortable with doing that. ● Athletic training student A athletic training student, if present, will assist by helping with an evaluation, retrieving emergency equipment, and following directions given by the ATC or team physician. ● Coaches Head and assistant coaches will assist by calling 911, directing EMS personnel to the site, providing crowd control, and giving priesthood blessings. ● EMS EMS will be called from a cell phone. The person who calls will stay on the line, give directions, and meet the EMS personnel at the gate/door to allow them in. Also, the person who calls must make sure that Provo EMS is dispatched, not just BYU EMS. Emergency Equipment ● Spineboard/Cervical Collar Located in the Extramural Sports Athletic Training Room (ESATR) in the Indoor Practice Facility (IPF) – not taken out to every practice. ● AED Extramural Sports has two. One is taken out to every practice. ● Splints/Crutches Located in the ESATR. Not taken out to every practice. ● Cell Phone Each ATC has a personal cell phone, as does each coach. Whoever calls will use their own phone. Other Considerations ● Insurance Information All Athletes insurance/emergency contact information is located in a plastic folder in the ATC's athletic training kit. ● Accompaniment An athletic training student or coach will accompany the athlete to the hospital if the practice is continuing. The ATC will go to the hospital when practice is over. Emergency Procedure for EXTRAMURAL SPORTS 67 BYU Athletic Training Procedures and Appendix Lacrosse, Rugby, and Soccer Games South Field and Helaman Field Personnel ● Staff ATC A certified athletic trainer on staff will be present for all games. ● Athletic Training Student An athletic training student may or may not be present. ● Team Physician A team physician is usually present at every home game. ● Coaches Head Coach Assistant Coaches ● EMS EMS will be activated by calling 911. EMS is not usually present at practices or games. Role of Personnel During Emergency ● Staff ATC The staff athletic trainer will direct care and designate responsibilities during an emergency. If EMS is required, the staff athletic trainer will direct someone to call. The ATC will defer control to someone who is more qualified (physician or Provo EMS) when he/she feels comfortable with doing that. Athletic Training Student An athletic training student, if present, will assist by helping with an evaluation, retrieving emergency equipment, and following directions given by the ATC or team physician. ● Team Physician A team physician will assist with any emergency when summoned by the ATC. Coaches Head and assistant coaches will assist by calling 911, directing EMS personnel to the site, providing crowd control, and giving priesthood blessings. ● EMS EMS will be called from a cell phone. The person who calls will stay on the line, give directions, and meet the EMS personnel at the gate/door to allow them in. Also, the person who calls must make sure that Provo EMS is dispatched, not just BYU EMS. Emergency Equipment ● Spineboard/Cervical Collar A spineboard and cervical collar will be located by the ―home‖ bench at every game. ● AED Extramural Sports has two. One is taken out to every game and kept by the ―home‖ bench. ● Splints/Crutches Located by the ―home‖ bench at every game. ● Cell Phone Each ATC has a personal cell phone, as does each coach. Whoever calls will use their own phone. ● Consecrated Oil A vial of consecrated oil is located in the ATC's athletic training kit. Other Considerations ● Insurance Information All Athletes insurance/emergency contact information is located in a plastic folder in the ATC's athletic training kit. ● Accompaniment 68 BYU Athletic Training Procedures and Appendix A student trainer or coach will accompany the athlete to the hospital if a family member is not present. The ATC will go to the hospital when the game is over. If Athlete Is a Visiting Team Member ● Visiting team has an ATC with them The BYU staff ATC will find out before the game if the visiting team has an ATC with them. The BYU staff ATC, student trainer, and/or team physician will assist with any emergency as needed. ● Visiting team does not have an ATC with them The BYU ATC will handle an emergency in this case the same as with any BYU athlete. When BYU Is Traveling ● Personnel A staff ATC will always travel with an Extramural team. A student trainer may or may not be present. A team physician will not be present. The staff ATC will direct care and designate responsibilities during any emergency situation. The coaches will assist by conferring with someone who can call 911 and direct EMS to the site, crowd control, giving priesthood blessings, and assisting the trainer in any way necessary. ● Emergency Equipment An AED will always be taken when traveling. Also, a bag with crutches and splints will be taken if there is not a conflict with other games at home when it might be needed. The ATC will always have a personal cell phone. When traveling internationally, the coach will have cell phone that will work. A vial of consecrated oil is kept in every ATC's athletic training kit. ● Insurance Information All athletes‘ insurance/emergency contact information is located in a plastic folder in the ATC's athletic training kit. ● Accompaniment A coach will accompany the athlete to the hospital in the event no family member is present. The ATC will go to the hospital once the game is over. 69 BYU Athletic Training Procedures and Appendix Emergency Procedure for CHEER Personnel A certified athletic trainer on staff will be present for team performances. They will follow the bulk of the team or be seated at a spot designated and known to the team. A certified athletic trainer will travel with the squad for major competitions and performances, unless the performance is with a sport staffed by a certified athletic trainer (for example, a football game competing away from home). An MD is available at football and basketball games. An MD will be present or on call during women‘s volleyball games. All athletic trainers at BYU will cover emergency care for ‗Cosmo‘ according to that sport‘s emergency protocol. While traveling for football games, cheer will contact the athletic trainers over football for any emergency needs; they will be available as per football‘s emergency protocols. Although not usual, that same guideline applies to any team cheer follows. The cheer coach will have a way to contact that athletic trainer, usually by cell phone. A certified athletic trainer will always be present during practice. EMS is usually on site during football and men‘s basketball games. EMS will be summoned by calling 911 during women‘s basketball and volleyball games, and cheer practice. Role of personnel for emergencies The certified athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS) who is affiliated with BYU or summoned by BYU personnel. If EMS is required, the staff athletic trainer will call by cell phone or direct someone to call. The staff athletic trainer will direct the coach or cheerleader to get the MD if needed, if present. The MD will come and stand by or assist if their help is needed or requested. The athletic trainer will direct someone to contact the athletic trainer over the competing team to assist in emergency care, retrieving emergency equipment, directing EMS to the site, and so on. If that athletic trainer is not available, the cheer coach will appropriately assist as needed. Telephone locations for practices Cellular phones can be used to dial '911.' Upstairs in the student weight room (293 SFH). Dial either '911' or '2-2222'; both calls will go to campus security when dialed from a BYU phone. Athletic department weight room — located at the north end of the hall from the gymnastics gym. Calling 911 from a BYU phone will contact BYU emergency services. The person calling should specifically point out that Provo EMS services are required for transportation. The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. Be sure that BYU EMS is not the only service sent, as BYU EMS has limited or no ability to transport an injured athlete. Practice procedures The practice facility is located in room 147 SFH (the gymnastics gym). The most accessible location for ambulance transport is through the south doors of the 70 BYU Athletic Training Procedures and Appendix gymnastics gym. Dispatchers should be told to have the ambulance drive up on the sidewalk between the indoor tennis courts and south side of the Smith Fieldhouse. Emergency equipment: vacuum splints, cervical collars and spine boards are located in the storage room of the main athletic training facility in the SFH and in the gymnastics gym at the southwest corner. Special considerations: o Emergency transport of a cheerleader who is lying in the foam pit involves unique circumstances. The foam is unstable, which may cause unwanted movement of the cheerleader, and makes it difficult for rescuers to get good footing. Prior practice of this skill is needed before attempting it in an emergency situation. o Be aware that the 4" and 8" foam mats are very soft, and can cause unwanted movement of the cheerleader if the rescuer approaches it too quickly. Take slow deliberate steps when approaching a cheerleader who is lying on one of these mats. 71 BYU Athletic Training Procedures and Appendix 72 BYU Athletic Training Procedures and Appendix APPENDIX D Off-Campus Emergency Action Plans 73 BYU Athletic Training Procedures and Appendix Springville High School Emergency Action Plan Personnel Head ATC: Lisa Walker ATC is available in person or by phone for all home practices/competitions. Will be seated with the team or available by phone and will go to needed venue as able. Athletic Training Students (ATS) A athletic training student may be with the team by assignment. EMS will be summoned by calling 911 Athletic Director/Administration Present at all varsity games. Available by phone. Role of Personnel During Emergency Head ATC The ATC will direct care and designate responsibilities during an emergency. Athletic Training Students (ATS) ATS will proceed under the direction of the ATC Physician (if available) will stand by or assist if their help is needed or requested. Other (coaches, EMS, etc) If the visiting team brings a certified athletic trainer, SHS personnel will assist as needed during any emergency. If the visiting team does not have an ATC, visiting team will be informed of ATC at SHS. ATC will assist the visiting team with care of the injured athlete. If the ATC is not available, responsibility of injury treatment rests on the coach or AD. SHS requires that all coaches maintain a current CPR and First Aid certification. EMS when summoned will follow local EMS protocol Location of Communication Devices Standard telephone If necessary, there is a telephone located in the Athletic Training Facility at the underground track, in any classroom or at the main office. You must dial 9 (dial tone) 9 (dial tone) to get an outside line. Cell Phone Cell phones are the best form of communication to the EMS system, as it allows for direct relay of information to the EMS. ATC, AD/ADMN carry cell phones. Location and Directions for EMS Person calling 911 will direct EMS to the correct venue/location of the injured athlete. The address of Springville High School is 1205 East 900 South, Springville. The EMS personnel should enter the large student parking lot on the West side of the main building. EMS will be met by a coach/administrator and directed to the location of the injured athlete. Location of Emergency and Specialty Equipment Spineboard — located in the athletic training facility or classroom G-3 (Walker). Splints — located in athletic training facility, under the treatment table, or classroom G-3 (Walker) in the 2nd cabinet behind the desk. Small splints may be present in Medical Kit with team. AED-NOAEDINSCHOOL Crutches — located in the athletic training facility or classroom G-3 (Walker) 74 BYU Athletic Training Procedures and Appendix Other Considerations All head coaches, AD/Admin, ATC have keys to the Athletic Training facility, outside doors and gates. ATS will have keys to the athletic training facility and the athletic department. The athlete‘s contact and health insurance information is located in the Medical kit. The ATC and the AD also have this information. All efforts will be made to notify the parent/guardian or other approved contact of the athlete with information about the whereabouts of the athlete. 75 BYU Athletic Training Procedures and Appendix Timpview Football Emergency Action Plan THS Football Field Personnel Ben Ross ATC Games: on sideline with team. Practices: on practice field with team or in Training Room. BYU Athletic Training Students Games: on sideline with team. Practices: on practice field with team or in Training Room. Dr. Scott Jackson—Team Physician Games: on sideline with team; varsity only, on call for sophomore and JV games. (He may be at some the sophomore games 2006 football season.) Practice: on call. Rogan Taylor—Physical Therapist (Or a Therapist from his office.) Games: on sideline with team. (Varsity games only; other games on call.) Practices: on call. Timpview Athletic Training Students Games: on sideline with team Practices: on field with team or in the Training Room. Other (Coaches, EMS, Administrator, etc.) Games: EMS will be motioned onto the field when needed, Varsity only. Other games EMS will be summoned by calling 911. Practice: EMS will be summoned by calling 911. Role of Personnel during Emergency ATC The athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS). Athletic Training Students Assist with athlete as needed. To get MD if needed. Stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician The MD will come onto the field and stand by or assist if their help is needed or requested. Other (Coaches, EMS, Administrator, etc.) Assist as requested and needed. If a visiting team brings a certified athletic trainer, Timpview personnel will assist as needed during any emergency. If the visiting team does not bring qualified medical staff, the Timpview ATC will direct care. 76 BYU Athletic Training Procedures and Appendix Location of Communication Devices Cell phone ATC will have a cell phone at competitions and practices. Coach Wong and others will have a cell phone on the field. Standard telephone If necessary, the nearest telephone is located in the weight room office. The weight room door is located just north of the Public Restrooms. The ATC, football coaches, administration, and janitorial staff will have keys to unlock the doors. Walkie talkie Usually administer on sideline has a walkie talkie to communicate to staff (varsity games only). Location and Directions for EMS EMS on location for varsity games only. EMS parks at the northeast corner of the track/field. For all other games call 911. The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. If using school phone dial ―9‖ (to get outside line) then dial 911. Directions Address: 3570 North 650 East (Timpview Drive). Go north of Timpview High to the corner of Timpview Drive and Quail Drive. Drive east on Quail Drive to the second parking lot. Turn right into student parking lot. Drive to the southeast corner of the parking lot until you see an opening between the seminary building and the industrial arts building. Turn up into the driving range/upper parking lot and drive to the gate and ticket booth at the southeast corner of the driving range. From there you will see football field and the road that goes down to the field. Location of Emergency and Specialty Equipment AED—located on home sideline Splint bag—located on home sideline Crutches—located on home sideline Spine board—located on home sideline or training room Other Considerations The ATC will have keys to the building doors and gates where EMS must enter. Administrators and janitorial staff will also have building and gate keys. The athlete‘s contact and health insurance information is located in the team training kit on the sideline. A coach or athletic trainer will be sent to the ER if a guardian is not available. 77 BYU Athletic Training Procedures and Appendix Timpview Baseball Emergency Action Plan THS Baseball Field Personnel Ben Ross ATC Game: In dugout with team or on call from another THS field. Practices: on practice field with team or in Training Room. BYU Athletic Training Students Game: In dugout with team Practices: on practice field with team or in Training Room. Team Physician Game: on call Practice: on call. Timpview Athletic Training Students Games: in dugout with team. Practices: on field with team or in the Training Room. Other (Coaches, EMS, Administrator, etc.) Games: EMS will be summoned by calling 911. Practice: EMS will be summoned by calling 911. Role of Personnel during Emergency ATC The athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS). Athletic Training Students Assist with athlete as needed. Get MD if needed. Stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician On call Other (Coaches, EMS, Administrator, etc.) Assist as requested and needed. If a visiting team brings a certified athletic trainer, Timpview personnel will assist as needed during any emergency. If the visiting team does not bring qualified medical staff, the Timpview ATC will direct care. Location of Communication Devices Cell phone ATC will have a cell phone at competitions and practices. Coaches and others will have a cell phone. Standard telephone If necessary, the nearest telephone is located in the training room. The ATC, BYU SAT, administration and janitorial staff will have keys to unlock the doors if needed. 78 BYU Athletic Training Procedures and Appendix Location and Directions for EMS EMS Call 911: The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. If using school phone dial ―9‖ (to get outside line) then dial 911. Directions Address: 3570 North 650 East (Timpview Drive). The Baseball field is south of the High School. From the intersection of 3230 North and Timpview Drive just past the first house to your right heading north on Timpview Drive turn right heading east into a gated road that goes up past the city park around the back of the baseball field, and brings you onto the field by the dugouts. Location of Emergency and Specialty Equipment AED—located on home dugout or at another THS field Splint bag—located on home sideline or at another THS field. Crutches—located in training room. Spine board—located in training room. Other Considerations The ATC will have keys to the building doors and gates where EMS must enter. Administrators and janitorial staff will also have building and gate keys. The athlete‘s contact and health insurance information is located in the team training kit on the sideline or coaches bag. A coach or athletic trainer will be sent to the ER if a guardian is not available. 79 BYU Athletic Training Procedures and Appendix Timpview Boys’ & Girls’ Soccer Emergency Action Plan THS Football/Soccer Field Personnel Ben Ross ATC Games: on sideline with team. Practices: on practice field with team or in Training Room. BYU Athletic Training Students Games: on sideline with team. Practices: on practice field with team or in Training Room. Team Physician Games: on call Practice: on call. Timpview Athletic Training Students Games: on sideline with team Practices: on field with team or in the Training Room. Other (Coaches, EMS, Administrator, etc.) Games: EMS will be summoned by calling 911. Practice: EMS will be summoned by calling 911. Role of Personnel during Emergency ATC The athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS). Athletic Training Students Assist with athlete as needed. To get MD if needed. Stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician On call Other (Coaches, EMS, Administrator, etc.) Assist as requested and needed. If a visiting team brings a certified athletic trainer, Timpview personnel will assist as needed during any emergency. If the visiting team does not bring qualified medical staff, the Timpview ATC will direct care. Location of Communication Devices Cell phone ATC will have a cell phone at competitions and practices. Coaches and others will have a cell phone on the field. Standard telephone If necessary, the nearest telephone is located in the weight room office. The weight room door is located just north of the Public Restrooms. The ATC, coaches, administration, and janitorial staff will have keys to unlock the doors. 80 BYU Athletic Training Procedures and Appendix Location and Directions for EMS EMS Call 911: The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. If using school phone dial ―9‖ (to get outside line) then dial 911. Directions Address: 3570 North 650 East (Timpview Drive). Go north of Timpview High to the corner of Timpview Drive and Quail Drive. Drive east on Quail Drive to the second parking lot. Turn right into student parking lot. Drive to the southeast corner of the parking lot until you see an opening between the seminary building and the industrial arts building. Turn up into the driving range/upper parking lot and drive to the gate and ticket booth at the southeast corner of the driving range. From there you will see football/soccer field and the road that goes down to the field. Location of Emergency and Specialty Equipment AED—located on home sideline Splint bag—located on home sideline Crutches—located on home sideline or training room. Spine board—located in training room. Other Considerations The ATC will have keys to the building doors and gates where EMS must enter. Administrators and janitorial staff will also have building and gate keys. The athlete‘s contact and health insurance information is located in the team training kit on the sideline. A coach or athletic trainer will be sent to the ER if a guardian is not available. 81 BYU Athletic Training Procedures and Appendix Timpview Softball Emergency Action Plan THS Softball Field Personnel Ben Ross ATC Game: In dugout with team or on call from another THS field. Practices: on practice field with team or in Training Room. BYU Athletic Training Students Game: In dugout with team Practices: on practice field with team or in Training Room. Team Physician Game: on call Practice: on call. Timpview Athletic Training Students Games: in dugout with team. Practices: on field with team or in the Training Room. Other (Coaches, EMS, Administrator, etc.) Games: EMS will be summoned by calling 911. Practice: EMS will be summoned by calling 911. Role of Personnel during Emergency ATC The athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS). Athletic Training Students Assist with athlete as needed. Get MD if needed. Stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician On call Other (Coaches, EMS, Administrator, etc.) Assist as requested and needed. If a visiting team brings a certified athletic trainer, Timpview personnel will assist as needed during any emergency. If the visiting team does not bring qualified medical staff, the Timpview ATC will direct care. Location of Communication Devices Cell phone ATC will have a cell phone at competitions and practices. Coaches and others will have a cell. Standard telephone If necessary, the nearest telephone is located in the main office of the school which is across the street east of the softball field. Administration and janitorial staff will have keys to unlock the doors if needed. 82 BYU Athletic Training Procedures and Appendix Location and Directions for EMS EMS Call 911: The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. If using school phone dial ―9‖ (to get outside line) then dial 911. If using main office phone push a number key to get an open line. Directions Address: 3570 North 650 East (Timpview Drive). The Softball field is directly across the street west of the front of the High School. Location of Emergency and Specialty Equipment AED—located on home dugout or at another THS field Splint bag—located on home sideline or at another THS field. Crutches—located in training room. Spine board—located in training room. Other Considerations The ATC will have keys to the building doors and gates where EMS must enter. Administrators and janitorial staff will also have building and gate keys. The athlete‘s contact and health insurance information is located in the team training kit on the sideline or coaches bag. A coach or athletic trainer will be sent to the ER if a guardian is not available. 83 BYU Athletic Training Procedures and Appendix Timpview Boys’ & Girls’ Basketball and Volleyball Emergency Action Plan THS Thunderdome Personnel Ben Ross ATC Games: on bench with team. Practices: in gym with team or in Training Room. BYU Athletic Training Students Games: on bench with team. Practices: in gym with team or in Training Room. Team Physician Games: on call; quite often in stands. Practice: on call. Timpview Athletic Training Students Games: on bench with team or in the stands behind the bench. Practices: in gym with team or in the Training Room. Other (Coaches, EMS, Administrator, etc.) Games: EMS will be summoned by calling 911. Practice: EMS will be summoned by calling 911. Role of Personnel during Emergency ATC The athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS). Athletic Training Students Assist with athlete as needed. Get MD if needed. Stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician On call. If in stands will assist when requested or if obviously needed without request. Other (Coaches, EMS, Administrator, etc.) Assist as requested and needed. If a visiting team brings a certified athletic trainer, Timpview personnel will assist as needed during any emergency. If the visiting team does not bring qualified medical staff, the Timpview ATC will direct care. Location of Communication Devices Cell phone ATC will have a cell phone at competitions and practices. Coaches and others will have a cell phone. Standard telephone If necessary, the nearest telephone is located in the coaches‘ offices. The offices are located at the south end of the Thunderdome upper level. The ATC, coaches, administration, and janitorial staff will have keys to unlock the doors. Walkie-talkie Usually administer in the gym has a walkie-talkie to communicate to staff (varsity games only). Location and Directions for EMS 84 BYU Athletic Training Procedures and Appendix EMS on call. Call 911: The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. If using school phone dial ―9‖ (to get outside line) then dial 911. Directions Address: 3570 North 650 East/(Timpview Drive). Go north of Timpview High to the corner of Timpview Drive and Quail Drive. Drive east on Quail Drive to the second parking lot. Turn right into student parking lot. Drive to the southeast corner of the parking lot until you see an opening between the seminary building and the industrial arts building. Turn up into the driving range/upper parking lot and drive to the gate and ticket booth at the southeast corner of the driving range. Go through the gate and follow the road down the hill to the back doors of the Thunderdome. This is very close to the court and the training room. Location of Emergency and Specialty Equipment AED—located at home bench. Splint bag—located at home bench or in training room. Crutches—located in training room. Spine board—located in training room. Other Considerations The ATC will have keys to the building doors and gates where EMS must enter. Administrators and janitorial staff will also have building and gate keys. The athlete‘s contact and health insurance information is located in the team training kit at the team bench. A coach or athletic trainer will be sent to the ER if a guardian is not available. 85 BYU Athletic Training Procedures and Appendix Timpview Boys’ & Girls’ Track Emergency Action Plan THS Track Personnel Ben Ross ATC Meet: at north end of track by high jump Practices: on practice field with team or in Training Room. BYU Athletic Training Students Meet: at north end of track by high jump Practices: on practice field with team or in Training Room. Team Physician Meets: on call Practice: on call. Timpview Athletic Training Students Games: at north end of track by high jump Practices: on field with team or in the Training Room. Other (Coaches, EMS, Administrator, etc.) Games: EMS will be summoned by calling 911. Practice: EMS will be summoned by calling 911. Role of Personnel during Emergency ATC The athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS). Athletic Training Students Assist with athlete as needed. Get MD if needed. Stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician On call Other (Coaches, EMS, Administrator, etc.) Assist as requested and needed. If a visiting team brings a certified athletic trainer, Timpview personnel will assist as needed during any emergency. If the visiting team does not bring qualified medical staff, the Timpview ATC will direct care. Location of communication Devices Cell phone ATC will have a cell phone at competitions and practices. Coaches and others will have a cell phone on the field. Standard telephone If necessary, the nearest telephone is located in the weight room office. The weight room door is located just north of the Public Restrooms. The ATC, coaches, administration, and janitorial staff will have keys to unlock the doors. 86 BYU Athletic Training Procedures and Appendix Location and Directions for EMS EMS Call 911: The person calling should wait for verification from dispatch that Provo EMS has been contacted and is en route. If using school phone dial ―9‖ (to get outside line) then dial 911. Directions Address: 3570 North 650 East (Timpview Drive). Go north of Timpview High to the corner of Timpview Drive and Quail Drive. Drive east on Quail Drive to the second parking lot. Turn right into student parking lot. Drive to the southeast corner of the parking lot until you see an opening between the seminary building and the industrial arts building. Turn up into the driving range/upper parking lot and drive to the gate and ticket booth at the southeast corner of the driving range. From there you will see the track and the road that goes down to the field. Location of Emergency and Specialty Equipment AED—located on home sideline Splint bag—located on home sideline Crutches—located on home sideline or training room. Spine board—located in training room. Other Considerations The ATC will have keys to the building doors and gates where EMS must enter. Administrators and janitorial staff will also have building and gate keys. The athlete‘s contact and health insurance information is located in the team training kit on the sideline. A coach or athletic trainer will be sent to the ER if a guardian is not available. 87 BYU Athletic Training Procedures and Appendix Pleasant Grove High School Athletics Emergency Action Plan Personnel Head ATC: Kristin Pond ATC is available in person or by phone for all home practices/competitions. Will be seated with the team or available by phone and will go to needed venue as able. Athletic Training Students (ATS) An athletic training student may be with the team by assignment. EMS Will be summoned by calling 911. An ambulance will only be on site for home football games. Athletic Director/Administration Present at all varsity games. Available by phone. Role of Personnel During Emergency Head ATC The ATC will direct care and designate responsibilities during an emergency. Athletic Training Students (ATS) ATS will proceed under the direction of the ATC EMS When summoned, will follow local EMS protocol. Other (coaches, physician, administration, etc) If the ATC is not available, responsibility of injury treatment rests on the coach or AD. SHS requires that all coaches maintain a current CPR and First Aid certification. Physician (if available) will stand by or assist if their help is needed or requested. AD/Administration will assist as needed. Visiting Teams If the visiting team brings a certified athletic trainer, PGHS personnel will assist as needed during any emergency. If the visiting team does not have an ATC, visiting team will be informed of ATC at PGHS. ATC will assist the visiting team with care of the injured athlete. Location of Communication Devices Cell Phone Cell phones are the best form of communication to the EMS system, as it allows for direct relay of information to the EMS. ATC, AD/ADMN carry cell phones. Standard telephone If necessary, there is a telephone located in the Training Room in the C gym, in any coach‘s office, in any classroom or at the main office. You must dial 9 to get an outside line. 88 BYU Athletic Training Procedures and Appendix Location and Directions for EMS Person calling 911 will direct EMS to the correct venue/location of the injured athlete. The address of Pleasant Grove High School is 700 East, 200 South in Pleasant Grove City. Ambulance entrances: Football, Soccer, Basketball, Wrestling, Tennis, Track/Field—enter through northwest gate (―top of the drag‖ by the football field.) Baseball or Softball fields—enter through Battlecreek Park, east of the school. EMS will be met by a coach/administrator and directed to the location of the injured athlete. Location of Emergency and Specialty Equipment Spineboards — located in Room 182 (Kristin Pond‘s classroom.) Splints — Far right lower cupboard in training room (near whirlpool) or Room 182 in the cupboard under the window. AED — NO AED IN SCHOOL Crutches – located behind the door in training room or Room 182 next to filing cabinet. Other Considerations All head coaches, AD/Admin, ATC have keys to the Training Room, outside doors and gates. ATS will have keys to the Training Room and the athletic department. Coaches have copies of their athlete‘s contact and health insurance information. Transporting Athletes with EMS: If a parent/guardian is present, they will accompany athlete in ambulance. If no parent, a coach or assistant coach will ride in ambulance with the student athlete. ATC will follow as permitted. All efforts will be made to notify the parent/guardian or other approved contact of the athlete with information about the whereabouts of the athlete. 89 BYU Athletic Training Procedures and Appendix Orem High School Emergency Action Plan Personnel Head ATC A certified athletic trainer will be present for all home athletic events competitions. They will be seated with the team or directly behind the team on the first row in the audience. If there is more than one event at the same time, and the certified athletic trainer is not present at the time of injury, the ATC will need to be contacted via cell phone. Other ATC No other ATC Athletic Training Students (ATS) An athletic training student will be seated with head athletic trainer at all events and competitions. Team Physician An MD will be on call. An MD is not usually present for practices or competitions. Other (coaches, administrators, EMS, etc.) EMS will be summoned by calling 911. EMS is not usually present for practices or competition. Role of Personnel During Emergency Head ATC The certified athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (for example, to a qualified physician or EMS) who is summoned by the head athletic trainer. If an injury occurs on the field or court, the head athletic trainer will attend to the athlete. The athletic training student on the side of the injury will stand nearby and assist when requested. If EMS is required, the head athletic trainer will call by cell phone or direct someone to call. Other ATC No other ATC Athletic Training Students (ATS) Athletic training student to contact the MD if needed. The athletic training student on the field or court opposite of the injury will stand by to retrieve emergency equipment, direct EMS to the site, or assist as necessary. Team Physician The MD will come to the field or court when called and stand by to assist if their help is needed or requested. Other (coaches, administrators, EMS, etc.) If the visiting team brings a certified athletic trainer, the home ATC will assist as needed during any emergency. The host athletic training student will contact the head home athletic trainer to communicate any needs if there is not an obvious injury on the field or court. If the visiting team brings a student or does not bring any medical staff, the head athletic trainer will direct care as needed. The school officer or administrator on duty will direct EMS once they have arrived and will unlock any gates or doors necessary. Coaches will need to contact the certified athletic trainer if there is more than one athletic event occurring simultaneously and the head athletic trainer is not present when an injury occurs. Location of Communication Devices Standard telephone If necessary, the nearest telephone is located in the training room at the north 90 BYU Athletic Training Procedures and Appendix end of the Fieldhouse. The ATC, student trainer, coaches, and administrators will have keys to access this room. You must dial two ―9‖s in order to dial out. Pay phone Not available Cell phone The certified athletic trainer will have a cell phone available at competitions. Emergency phone Not available Walkie talkie Not available Location and Directions for EMS Calling 911 will contact Orem emergency services. The person calling should wait for verification from dispatch that EMS has been contacted and is en route for transportation of the injured athlete. Location Not applicable Directions The address for Orem High School is 175 S. 400 E. Specific destinations for arrival of EMS is divided into 4 separate destinations or entrances. Football practice, soccer, and softball fields. EMS should arrive on the east side behind the school on Campus Drive. Someone will be waiting at the fence to allow them through the gate and further direct EMS. Football and wrestling competitions. EMS should arrive at the main parking lot from 400 E. and drive east toward the football field, between the main high school and technology buildings. Someone will be waiting at the gate to unlock it and further direct EMS. Baseball field. EMS should arrive on 400 E. at the entrance between the high school and seminary buildings. Someone with keys will be waiting at the gate to allow entrance and further direct EMS. Basketball and volleyball competitions, or Tiger Fieldhouse location. EMS should enter through the main parking lot and head east between the high school and technology buildings. The Fieldhouse is then north from this point. Someone will be waiting to open the gate to allow entrance to the Fieldhouse and further direct EMS. Location of Emergency and Specialty Equipment Spineboard—located behind the ―home‖ bench or in the football training room Splint bag—located behind the ―home‖ bench or in the football training room AED—none available Crutches—located behind the ―home‖ bench, or in the Fieldhouse training room Scoop stretcher—none available Lightning detector—none available Other Considerations The head ATC, athletic training student, coaches, and administrators will have keys to the training room. School administrators or the school officer on duty will have keys to the outside gates and building doors where the EMS must enter. The athlete‘s contact and health insurance information is located in the Fieldhouse training room or in the head ATC‘s athletic training kit for football. It is positioned behind the end of the ―home‖ bench. All coaches must be certified in basic emergency procedures. If the head athletic trainer is needed at another event, coaches will need to call EMS and will need to notify the 91 BYU Athletic Training Procedures and Appendix head ATC. Administrators and the athletic director must be present at all home events and competitions to direct EMS and to unlock necessary gates and entrances. Athlete's parents will be notified of any emergency involving their child. If a guardian is not present at the competition, a coach will be sent with the athlete. 92 BYU Athletic Training Procedures and Appendix American Fork High School Football Emergency Action Plan NOTE: An ambulance will be on site for all home Varsity football games, but not for JV/Sophomore. Dr. Michael Callahan, will also be present for most varsity games. A coaching staff member who has keys to the compound gate, the outside doors to the school and the training room needs to be present at every game, for the entire game. It would also be helpful if they had a cell phone. In the event of an emergency, the Certified Athletic Trainer (ATC) will be summoned if not already on site. If the ATC is not available, the head coach is now in charge. Emergency Personnel Certified Athletic Trainer Coaches (Should all be CPR and First Aid certified) Other First-aid/CPR trained staff Emergency Communication Individual cell phones are best. If you have one, please bring it to the games. Land-line phone in the training room. Dial 9 to get out of the system and then 9-1-1 Phone number for the training room is (801) 756-8547 Ext. 238 To get into the training room you will possibly need three keys, one for the outer doors to the school (TE8), one to the east gym (1) and one for the training room (TR). Emergency Equipment Team medical kit (on field) Crutches—Right hand wall of training room storage closet Air Splints—Last shelf, left hand side of training room storage closet Ice cooler with bags—on the field and in the training room; bags on left hand side of ice machine Role of First Responder #1 Immediate care of injured or ill student-athlete Activation of emergency medical system (EMS) if needed Call 911. Provide your name, address, telephone number, number of individuals injured, age, conditions and other information as requested. Notify administration during school hours Notify the student-athlete‘s parents. Locate the athletes physical in the team physical folder included in the medical kit. The physicals should be in alphabetical order. Role of First Responder #2 Emergency equipment retrieval Direction of EMS to the scene Open appropriate gates (Compound gate key will be needed here.) Designate or be the individual to ―flag down‖ EMS and direct them to the scene Scene control: Limit scene to first aid providers and move bystanders and teammates away from the area Venue Directions 93 BYU Athletic Training Procedures and Appendix For any injuries on the football fields, direct EMS to come to the south end of the school to the compound gate. Have them come to their right to the football field (or give them further information as to where you are specifically.) It may be necessary to recruit the help of others to keep the crowd back so the ambulance can get in. Medical Emergencies Include but are not limited to: An athlete who is not breathing with or without a pulse Severe difficulty breathing, whistling sound while breathing, gurgling sound, high pitched wheeze Loss of consciousness or altered mental state longer than 10 minutes Allergic reaction (bee sting, something ingested) Broken bones, especially those through the skin Severe bleeding Other 94 BYU Athletic Training Procedures and Appendix American Fork High School Soccer Emergency Action Plan An administrator/athletic director who has keys to the compound gate, the outside doors to the school and the training room needs to be present at every game, for the entire game. It would also be helpful if they had a cell phone. In the event of an emergency, the Certified Athletic Trainer (ATC) will be summoned if not already on site. If the ATC is not available, the head coach is now in charge. Emergency Personnel Certified Athletic Trainer Coaches (Should all be CPR and First Aid certified) Other First-aid/CPR trained staff Athletic directors Administrators Emergency Communication Individual cell phones are best. If you have one, please bring it to the games. Land-line phone in the training room. Dial 9 to get out of the system and then 9-1-1 Phone number for the training room is (801) 756-8547 Ext. 238 To get into the training room you will possibly need three keys, one for the outer doors to the school (TE8), one to the east gym (1) and one for the training room (TR). Emergency Equipment Team medical kit (on field) Crutches—Right hand wall of training room storage closet Air Splints—Last shelf, left hand side of training room storage closet Ice cooler with bags—on the field and in the training room; bags on left hand side of ice machine Role of First Responder #1 Immediate care of injured or ill student-athlete Activation of emergency medical system (EMS) if needed Call 9-1-1. Provide your name, address, telephone number, number of individuals injured, age, conditions and other information as requested. Notify administration during school hours Notify the student-athlete‘s parents. Locate the athletes physical in the team physical folder included in the medical kit. The physicals should be in alphabetical order. Role of First Responder #2 Emergency equipment retrieval Direction of EMS to the scene Open appropriate gates (Compound gate key will be needed here.) Designate or be the individual to ―flag down‖ EMS and direct them to the scene Scene control: Limit scene to first aid providers and move bystanders and teammates away from the area Venue Directions 95 BYU Athletic Training Procedures and Appendix For any injuries on the soccer fields, direct EMS to come to the south end of the school to the compound gate. Have them come to their right to the football field fence and follow the fence around the south end heading north around the bleachers. The soccer field is northeast of the school. Give them further information as to where you are specifically. It may be necessary to recruit the help of others to keep the crowd back and to help direct the ambulance to the proper location. Medical Emergencies Include but are not limited to: An athlete who is not breathing with or without a pulse Severe difficulty breathing, whistling sound while breathing, gurgling sound, high pitched wheeze Loss of consciousness Allergic reaction (bee sting, something ingested) Broken bones, especially those through the skin Severe bleeding Other 96 BYU Athletic Training Procedures and Appendix American Fork High School Volleyball/Basketball/Wrestling Emergency Action Plan An administrator/athletic director who has keys to the compound gate, the outside doors to the school and the training room needs to be present at every game, for the entire game. It would also be helpful if they had a cell phone. In the event of an emergency, the Certified Athletic Trainer (ATC) will be summoned if not already on site. If the ATC is not available, the head coach is now in charge. Emergency Personnel Certified Athletic Trainer Coaches (Should all be CPR and First Aid certified) Other First-aid/CPR trained staff Athletic directors, and Administrators Emergency Communication Individual cell phones are best. If you have one, please bring it to the games. Land-line phone in the training room. You will need a (1) key to access this phone. Dial 9 to get out of the system and then 9-1-1. Phone number for the training room is (801) 756-8547 Ext. 238 Land-line phone in coaches‘ office through the varsity boys‘ locker room. You will need a (1) key to access this phone Emergency Equipment Team medical kit (on court) Crutches—Right hand wall of training room storage closet Air Splints—Last shelf, left hand side of training room storage closet Ice cooler with bags—on the field and in the training room; bags on left hand side of ice machine Role of First Responder #1 Immediate care of injured or ill student-athlete Activation of emergency medical system (EMS) if needed Call 911. Provide your name, address, and telephone number, number of individuals injured, age, conditions and other information as requested. Notify administration during school hours Notify the student-athlete‘s parents. Locate the athletes physical in the team physical folder included in the medical kit. The physicals should be in alphabetical order. Role of First Responder #2 Emergency equipment retrieval Direction of EMS to the scene Open appropriate gates (Compound gate key will be needed here.) Designate or be the individual to ―flag down‖ EMS and direct them to the scene Scene control: Limit scene to first aid providers and move bystanders and teammates away from the area Venue Directions 97 BYU Athletic Training Procedures and Appendix For any injuries on the court, direct EMS to come to the south end of the school to the compound gate. Have them come straight in to the main gym doors, and then into the main gym (to their right.) Have someone meet the ambulance crew to direct them to an auxiliary gym if needed. It may be necessary to recruit the help of others to keep the crowd back so the ambulance can get in. If the injury occurred in the wrestling room, direct emergency personnel to the south east gym doors, in between the main and east gyms. Medical Emergencies Include but are not limited to: An athlete who is not breathing with or without a pulse Severe difficulty breathing, whistling sound while breathing, gurgling sound, high pitched wheeze Loss of consciousness Allergic reaction (bee sting, something ingested) Broken bones, especially those through the skin Severe bleeding Other 98 BYU Athletic Training Procedures and Appendix Mountain View High School Emergency Action Plan Personnel Head ATC—will be present for all home athletic events and competitions. They will be seated with the team and if more then one event is going on will be available by cell phone. Other ATC—none Athletic Training Student (ATS) —will be seated with head ATC. Team Physician—is on call EMS—available by calling 911 if needed Athletic Director/Administration—is present at all varsity competitions Role of Personnel During Emergency Head ATC—administer direct care of injury and designate responsibilities if needed during emergency. Other ATC—none Athletic Training Student (ATS) —assist ATC with any needs deemed necessary. Team Physician—if present will be available to assist if help is needed or requested. EMS—if summoned will follow their protocol. Athletic Director/Administration—will be available for assistance if needed or to call EMS and provide keys for EMS access to the field. They may also assist crowd control. Coaches—if ATC is not available they are now in charge. Visiting Teams—if they have an ATC present then MV ATC will assist them if necessary, but if their ATC is not present then MV ATC will proceed as normal. Location of Communication Devices Standard telephone—located in training room and you must press 9 to dial out. Pay phone—none Cell phone—ATC carries one. Emergency phone—none Walkie-talkie—AD/Administration carry them as well as the police officer. Location and Directions for EMS Mountain View High school is located at 645 West Center Street in Orem. Specific directions for individual destinations are as follows: Football Practice—EMS should turn on the road west of the school and enter faculty parking lot. Someone will be waiting to guide them further. Football Games—EMS should turn into main parking lot east of the school and drive to the northwest corner of the stadium where someone with keys will meet them at the gate and direct them further. Soccer Field—EMS should turn on the road west of the school and continue through until the stop sign where they will turn left. This road leads directly to the soccer field where a person will be waiting to guide them further. Softball/Baseball Fields—EMS should come up on 400 South and turn north onto the road just west of Orem elementary school. This road leads directly to the fields and someone will meet them there to guide them further. Basketball/Volleyball/Wrestling—EMS should turn on the road just west of the school and continue to the blue doors facing north. Someone will meet them there to let them in and guide them further. Location of Emergency and Specialty Equipment Spineboard—none 99 BYU Athletic Training Procedures and Appendix Splint bag—with ATC or in training room on shelves under taping table. AED—none Crutches—in training room by the ice machine. Scoop Stretcher—none Lightening Detector—none Other Considerations Keys—AD/Administration and coaches have keys to the stadium as well as the school. ATC has keys to the school and training room. Location of contact information for the following: Athlete‘s Parents—ATC carries info on sheet in bag and is also located on physical form in AD‘s office. If a parent is not available or cannot be reached then a coach will accompany the athlete when being transported by EMS. Head ATC—AD/Administration as well as coaches have phone numbers. Athletic Training facility—AD/Administration have the phone numbers as well as coaches. Custodians—AD/Administration have these phone numbers. Coaches—AD/Administration as well as ATC have their phone numbers. They are also listed on a sheet in the desk drawer in the training room. Athletic Director (AD) or Administration—ATC has their phone numbers. Athlete‘s Insurance—this information is listed on their physical in the AD‘s office and also on a sheet in the ATC‘s bag. 100 BYU Athletic Training Procedures and Appendix Lehi High School Emergency Action Plan Personnel Who will be present and location of each individual at the venue? Head ATC: Katie Habecker Other ATC: Steve Orrock Athletic Training Students (ATS): as assigned Team Physician: none Other (coaches, EMS, etc.): Dan Rice, sports med teacher Role of Personnel During Emergency Describe each member‘s role in detail. State the location of all emergency and specialty equipment. Who will retrieve the equipment during an emergency? Head ATC: will attend to the situation along with other trained staff Other ATC Athletic Training Students (ATS): will retrieve equipment and assist the head ATC Team Physician: isn‘t usually present Other (coaches, EMS, etc.): will assist in helping ATC, crowd control, alerting EMS etc. Location of Communication Devices State the devices that will be used at the venue in case of emergency and where they will be located. Please state where the closest land line phone will be located in addition to any cell phone. Standard telephone: front office Pay phone: Cell phone: with me at all times Emergency phone Walkie-talkie: staff and administrators have these at all times; they can call EMS from these radios Location and Directions for EMS Location EMS are on-site for football games only; they are parked at the north end of the track Directions EMS can enter through a gate on the south end of the school, near the track. This gives access to all gyms. They can also enter on the northeast side of the school to access track, football field, soccer field, softball, and baseball fields. Location of Emergency and Specialty Equipment Spineboard: athletic training room Splint bag: athletic training room AED: school nurse‘s office Crutches: none Scoop stretcher: none Lightning detector: none 101 BYU Athletic Training Procedures and Appendix Other Considerations Answer the following questions that apply. Please include any other special considerations you feel are important in case of an emergency. Who has the keys — Doug Webb, Principal; Lynn Allan, AD; other administrators Contact information (State this information or where you can find this information? Please do not state phonebook or campus directory.) Athlete‘s parent: on info card in office ATC: all coaches and administrator should have it Athletic training facility: no telephone Custodial: contact via radio Coaches Athletic director or Administrator Athlete‘s insurance: on info card in office Who goes with the athlete to the ER? Usually a parent 102 BYU Athletic Training Procedures and Appendix Emergency Plan for Timpanogos High School Personnel Head Certified Athletic Trainer — Joshua Robinson A certified athletic trainer will be present for all athletic events. They will be seated/standing with the team. In the event that the ATC is covering multiple events occurring simultaneously at the high school, the ATC will cover the event with the highest probability of incident, and will be in communication via cell phone and/or two-way radio with the other events. Athletic Training Students When present, athletic training students are not allowed to interact with athletes without the presence of an ATC. Athletic training students will assist the ATC during an emergency. Team Physician — Dr. Karl Weenig Team physician will attend football games or be on call, standing on the sideline. Physician will be on call for all athletic events Coaches, etc. Coaches will be on the sideline/bench with their team EMS EMS will be activated by calling 911. EMS usually not in attendance. Role of Personnel During an Emergency Head ATC The head athletic trainer will direct care and designate responsibilities during an emergency. Anyone dealing with an emergency situation will defer control to the person most qualified (i.e., qualified physicians, certified athletic trainers, or EMS). If an injury occurs, the staff athletic trainer will attend to the athlete; athletic training students and assistant coaches will stand by and assist the head ATC. If EMS is needed, the ATC will call or direct someone to activate EMS. Athletic Training Students Student trainers will assist and accompany the head ATC onto the field/court. Student trainers will accompany the injured athlete to the hospital, doctor‘s office, etc. if parents are unable to be contacted. Coaches, Assistant Coaches, etc. If student trainers are unavailable, assistant coaches will assume the responsibilities of the student trainer. Coaches will have medical/contact information readily available. If an injury occurs, they will contact the parents/guardians of the injured athlete. Team Physician The attending team physician will come to the field/court or assist if needed or requested by the head ATC. School Administrators The school‘s administrators present at the events will ensure that all gates, roadways, and doors are unlocked and clear of spectators to provide open access for EMS vehicles and personnel. Location of Communication Devices Cell Phones will be the main source of communication. A list of cell numbers of athletic trainers, team physicians, etc. will be in the training bags of each team. 103 BYU Athletic Training Procedures and Appendix A land line phone is located in the athletic training room (Room 101) at Timpanogos High School. Dial 9 to dial to an outside line, and then dial the number. Two-way walkie talkie radios will be used by the athletic events staff and the school‘s administration. Location and Directions for EMS Timpanogos High School is located at 1450 North 200 East in Orem, Utah. To access the school from the south and west use Main St. to Timberwolf Blvd. (1430 North) or 1600 North to 150 East; from the east, use 400 East to Timberwolf Blvd. (about 1430 North). The football, soccer, and baseball fields are located on the south side of the school. EMS access is available. Speed bumps are in place on the road that leads to the fields behind the school. The gyms are located on the southeast side of the school. Doors allow for direct outside entrance into the gym for EMS personnel. Location of Emergency Equipment Spine board—located behind the ―home‖ bench Vacuum Splint Bag—located behind the ―home‖ bench Crutches—located behind ―home‖ bench Medical/contact information—will be in the athletic trainer‘s bag or with the coach. 104 BYU Athletic Training Procedures and Appendix Physical & Sports Therapy Services — Springville Emergency Action Plan Personnel Physical Therapists Office Staff Aides Role of Personnel Physical Therapists: in charge during any emergency and will give directions to others when needed Office Staff: assist physical therapists and aides when needed Aides: assist the patients Location of Telephones Front desk Office (2) Back sink Stereo cabinet Directions for EMS Address Professional Arts Medical Center 380 East 400 South, Springville Directions Head east on 400 South past 300 East. Turn right at the driveway before the intersection of 400 East and 400 South (directly before the gas station). Follow the parking lot to the back building. Location of Emergency Equipment Fire extinguisher on the wall of the x-ray room Crutches in x-ray room Splints in cast room First Aid supplies in stereo cabinets 105 BYU Athletic Training Procedures and Appendix Performance Rehab Clinics, Orem Emergency Action Plan Personnel • Physical Therapists • Aides Role of Personnel • Physical Therapists Responsibilities include safety of patients and aides in emergent situations, providing directions and/or instructions in order to preserve health, safety, and well-being of all individuals in the clinic. • Aides Assist the physical therapist and patients as needed, promoting health and safety. Location of Telephones • Front desk • Office • Treatment area Location of Emergency Equipment • Two fire extinguishers: One on the wall of treatment area, next to scale and drinking fountain, one next to fire exit, in rehab equipment area • Pocket masks: top drawer of every examination room of adjoining occ-med clinic • Crutches: supply room • Splints: supply room • First Aid supplies in trauma room Address and Directions for EMS Address 607 N 1200 W, Orem, UT 84057 Directions • Head north on 1200 West • Turn left into the parking lot just before 600 North 106 BYU Athletic Training Procedures and Appendix APPENDIX E Athletic Training Course Descriptions and Learning Outcomes 107 BYU Athletic Training Procedures and Appendix EXSC 302 Philosophical and ethical issues common to exercise sciences majors. Concept of mind, body, spirit Outcomes: Tenets of Philosophy Concerning Multicultural Traditions Learn contemporary tenets of philosophy that will serve as a basis for understanding important ideas in our own cultural tradition as well as that of others. Philosophical Worldviews Comprehend philosophical worldviews to facilitate respectful relationships with others. Beliefs and Values Pursue truth, think clearly and communicate effectively one‘s own beliefs and values; deepen one‘s understanding of the nature of being. The Gospel of Jesus Christ Comprehend and apply the truths of the gospel of Jesus Christ. Reflect devout love of God and a loving, genuine concern for the welfare of others in the learning environment Spirituality Acquire/reinforce a profound respect for the divine nature of one‘s own life, a reverence for one‘s value, the purpose of one‘s life and a desire to live a healthy lifestyle. Valuing the Entire Self Articulate one‘s valuing of the entire self, bodymindspirit, with particular focus on the meaning and importance of the physical body. Formulating Personal and Professional Philosophy Strengthen the formulation of own personal and professional philosophy establishing clear standards of integrity. Improve the communication of one‘s beliefs, written and verbal. Ethical Analysis and Behavior Analyze contemporary issues from an ethical standpoint. Demonstrate own professional ethical behavior, think critically and take an informed position on an issue. EXSC 320 Recognition, evaluation, and care of athletic injuries. Techniques in taping, preventing, and rehabilitating injuries Outcomes: Responsibilities, Roles, and Tasks Review general responsibilities, roles, and tasks of athletic trainers, physical therapists, and other allied health professionals involved in sports medicine. Musculoskeletal Injuries Learn assessment, first aid, and treatments for common musculoskeletal injuries. Injury Prevention Examine methods of injury prevention including conditioning principles, environmental hazards, and protective equipment. Resources Learn and utilize resources available to sports medicine professionals. Application Apply knowledge to practical situations. EXSC 321 Basic Athletic Training Lab Outcomes: Taping Demonstrate competency and proficiency in taping the ankle, foot, lower leg, knee, thigh/hip, shoulder, elbow, wrist, thumb, and finger joints. Wrapping Demonstrate competency and proficiency in wrapping the ankle, foot, lower leg, thigh/hip, shoulder, elbow, wrist, thumb, and finger joints. Wound Care Management Demonstrate competency and profiency in wound care management. Injury Evaluation Demonstrate competency and profiency in injury evaluation. Injury Treatment Management Demonstrate competency and profiency in injury treatment management. 108 BYU Athletic Training Procedures and Appendix Spineboarding and Splinting Demonstrate competency and profiency in spineboarding and splinting. EXSC 362 Kinesiology and Biomechanics Outcomes: Physical Laws and Human Performance Demonstrate application of physical laws to human performance. Kinematics of Human Motion Calculate kinematics of human motion. Projectile Motion Equations Show comprehension of projectile motion equations. Changes of Motion Determine changes of motion due to forces. Fluids Generating Force Demonstrate understanding of how fluids generate force. EXSC 394 Classroom and field experience. Orientation to athletic training program and clinical expectations. Modules include emergency care, taping skills, and basic modalities. Outcomes: Administrative Roles and Policies of Various Health Care Org After completing this course, the student will be able to understand the administrative roles and policies of various health care organizations including: a. CAATE b. NATA c. BOC Accurate Record Keeping Skills Demonstrate the skills necessary for accurate record keeping including SOAP notes and correct documentation of HOPS Purchasing Policies Understand purchasing policies for supplies Emergency Action Plans Correctly devise and implement emergency action plans Emergency Conditions Demonstrate the necessary skills for care of emergency conditions Treating Open Wounds Demonstrate care and necessary skills for treating open wounds Therapeutic Modalities 1. Demonstrate correct use, including indications and contraindications for therapeutic modalities including:a. Hot Packs b. Ultrasound Evaluating Lower Extremities 1. Demonstrate correct evaluation techniques of lower extremities including: a. Foot b. Ankle c. Lower Leg d. Knee e. Hip EXSC 395 Classroom and field experience. Modules include taping skills, assessment, and modalities Outcomes: Rehabilitation Skills Demonstrate rehabilitation skills, including aquatic therapy, joint mobilizations, proprioception, neuromuscular control, and agility exercises. Taping and Bracing Demonstrate competency and clinical proficiency in taping and bracing. Evaluation Skills of Caring for Upper Extremity Injuries Demonstrate the skills necessary to properly evaluate and care for upper extremity injuries including shoulder, elbow, forearm, wrist, hand, head and face, and thorax and abdomen. Alter G Machine and Rebounder Demonstrate the use of the following rehabilitation tools: Alter G machine and Rebounder EXSC 400 Advanced examination of structure and function of skeletal, articular, muscular, and peripheral nervous systems with clinical applications; cadaver lab included Outcomes: 109 BYU Athletic Training Procedures and Appendix Anatomical Terms Upon completion of this class students will be able to accomplish the following: Be familiar with the anatomical terms and their meanings for the human skeletal, peripheral nervous, articular, and muscular systems in relation to movement and orthopaedics. Movement Identify and discuss the structures, functions and inter-relationships of the human skeletal, peripheral nervous, articular, and muscular systems with respect to movement. EXSC 414 Advanced athletic training skills, including taping, bracing and splinting, custom-fitted equipment, massage and stretching techniques, and emergency splinting and transport Outcomes: CAATE Competencies At the end of this course, the student will demonstrate competency in each of the following CAATE competencies: Select and fit appropriate standard protective equipment on the patient for safe participation in sport and/or physical activity. This includes but is not limited to: Shoulder Pads, Helmet/Headgear, Footwear, Mouthguard, Prophylactic Knee Brace, Prophylactic Ankle Brace, Other Equipment (as appropriate Special Protective Procedures and Devices Select, fabricate, and apply appropriate preventive taping and wrapping procedures, splints, braces, and other special protective devices. Procedures and devices should be consistent with sound anatomical and biomechanical principles. Environmental Data Obtain, interpret, and make decisions regarding environmental data. This includes, but is not limited to the ability to:RM-P6.2. Formulate and implement a comprehensive, proactive emergency action plan specific to lightening safety Apply and Document Special Tests and Instruments Apply commonly used special tests and instruments (e.g., otoscope, stethoscope, ophthalmoscope, peak flowmeter, chemical ―dipsticks‖ [or similar devices]) and document the results for the assessment of: Vital signs including respiration (including asthma), pulse and circulation, and blood pressure Emergency Treatment Strategies Implement appropriate emergency treatment strategies, including but not limited to:AC-P3c Establish and maintain an airway in a patient wearing shoulder pads, headgear or other protective equipment and/or with a suspected spine injury Techniques for Therapeutic Exercises Instruct the patient in proper techniques of commonly prescribed therapeutic exercises. Risk Management Plans for Safe and Efficient Health Care Facility Develop risk management plans, including facility design, for safe and efficient health care facilities. Risk Management Plan for Security and Protection Develop a risk management plan that addresses issues of liability reduction; security, fire, and facility hazards; electrical and equipment safety; and emergency preparedness. Athletic Training Policies and Procedures Within a Health Care Facility Develop policy and write procedures to guide the intended operation of athletic training services within a health care facility. EXSC 415 Hydrotherapy, massage, traction, radiant energy, heat, cold, and electrotherapy Outcomes: Cryotherapy The student will demonstrate the ability to properly select the appropriate parameters, prepare, and apply a(n): a.cold whirlpool treatment b.controlled cold therapy unit c.ice bag d.vapo-coolant spray e.ice immersion f.ice massage g.contrast bath h.cryokinetics Thermotherapy The student will demonstrate the ability to properly select appropriate parameters, prepare, and apply a(n): a.moist heat pack b.paraffin treatment c.warm whirlpool treatment d.fluidotherapy e.diathermy f.infrared Electrotherapy The student will demonstrate the ability to properly select appropriate parameters, prepare, and apply a(n): a.sensory-level pain control treatment b.noxious-level pain control treatment c.motor-level pain control treatment d.muscle re-education treatment e.muscle pumping treatment f.acute edema treatment g.chronic edema treatment 110 BYU Athletic Training Procedures and Appendix h.muscle spasm treatment i.muscle splinting treatment j.muscle atrophy retardation treatment k.iontophoresis treatment l.MENS treatment Electrical Stimulation Units The student will demonstrate proficiency in the setup and application of the following types of electrical stimulation units: a.Monophasic stimulator (e.g., high volt stimulation) b.Biphasic stimulator (e.g., TENS, NMES) c.Direct current (e.g., iontophoresis) d.Alternating current (e.g., interferential, NMES) Ultrasound The student will demonstrate the ability to properly select appropriate parameters, prepare, and apply a: a.thermal direct/indirect ultrasound treatment b.non-thermal direct/indirect ultrasound treatment c.combination electric-stimulation/ultrasound treatment d.phonophoresis treatment Traction The student will demonstrate the ability to properly select appropriate parameters, prepare, and apply: a.mechanical traction b.manual traction c.positional traction Intermittent Compression The student will demonstrate the ability to properly select appropriate parameters, prepare, and apply intermittent compression. Massage The student will demonstrate the ability to prepare and apply a massage treatment. The student will demonstrate the ability to properly perform massage strokes. a.effleurage b.petrissage c.friction d.tapotement e.vibration EXSC 416 Basic principles of injury evaluation; evaluation techniques specific to lower-extremity injuries. Outcomes: Instructing and Interpretting Fitness Tests Instruct the patient how to properly perform fitness tests to assess his or her physical status and readiness for physical activity. Interpret the results of these tests according to requirements established by appropriate governing agencies and/or a physician. These tests should assess: Muscular Endurance, Agility, Speed. Appropriate Fitness Programs for Patients Develop a fitness program appropriate to the patient‘s needs and selected activity or activities that meet the requirements established by the appropriate governing agency and/or physician for enhancing: Cardiovascular Endurance, Speed Inspection/Observation of the Clinical Signs Associated with Perform inspection/observation of the clinical signs associated with common injuries including deformity, posturing and guarding, edema/swelling, hemarthrosis, and discoloration. Palpate the bones and soft tissues to determine normal or pathological characteristics. Measure the active and passive joint range of motion using commonly accepted techniques, including the use of a goniometer and inclinometer. Grade the resisted joint range of motion/manual muscle testing and break tests. Apply appropriate stress tests for ligamentous or capsular stability, soft tissue and muscle, and fractures. Apply appropriate special tests for injuries to the specific areas of the body as listed above. Assess neurological status, including cranial nerve function, myotomes, dermatomes and reflexes, and circulatory status. Document the results of the assessment including the diagnosis. Patient's Prior and Present Medical History Obtain a medical history of the patient that includes a previous history and a history of the present condition. Perform a visual observation of the clinical signs associated with common injuries and/or illnesses including deformity, edema/swelling, discoloration, and skin abnormalities. Palpate the bones and soft tissues, including the abdomen, to determine normal or pathological characteristics. EXSC 417 Injury evaluation techniques specific to the upper extremities and trunk Outcomes: Mechanisms of Common Injuries in Various Sports Upon completion of this course, the student will understand and be able to explain and/or demonstrate by performance on an exam: Mechanisms of common injuries in various sports. Evaluation and Diagnostic Terminology Basic principles of evaluation and diagnostic terminology. 111 BYU Athletic Training Procedures and Appendix Upper Extremity Injuries Signs and symptoms of upper extremity injuries. Injury Evaluation Specific steps in injury evaluation. Evaluation Techniques for Upper Extremity Injuries Evaluation techniques, including special tests, used to identify and assess degree of disability of the upper extremity. Manual Muscle Testing Proficiency in performing manual muscle testing of the upper extremity. Girth and Goniometric Measurements Proficiency in performing girth and goniometric measurements of the upper extremity. On-the-Field/Off-the-Field Injury Management Basic on-the-field/off-the-field injury management. EXSC 418 Basic principles, techniques, and progression of orthopedic/musculoskeletal rehabilitation Outcomes: Tissue Healing Understand tissue healing and how therapeutic exercise affects tissue healing. Functional Progression Understand the concept of functional progression and how it guides individual rehabilitation protocols. Rehabilitation is not a recipe that fits all people. Therapeutic Exercise, Range of Motion, and Manual Therapy Te Apply and understand therapeutic exercise, range of motion, and manual therapy techniques to enhance the goals within a rehabilitation plan for athletic injury. Goals of Rehabilitation Synthesize the different goals of rehabilitation to be combined for any injury and condition to return the patient to full activity. EXSC 419 Discussion of current medical issues in athletic training, with guest lectures by medical specialists Outcomes: Exposure to a Variety of Medical Conditions Advanced seminar type class for exposure to a variety of medical conditions, given from MD‘s point of view. Common Athlete illnesses Learn a medical doctor‘s approach to illnesses which athletes commonly experience. Athletic Trainer's Responsibility Integrate the athletic trainer‘s responsibility as it pertains to a team approach with the physician. EXSC 423 Management and administration of athletic training facilities and staff members Outcomes: Planning, Coordinating, and Supervising Explain the importance of planning, coordinating, and supervising in the administration of an athletic training room/program. Budgeting Systems Explain various budgeting systems and develop budgets for high school and collegiate athletic training programs. Athletic Training Facilities Design athletic training facilities to meet specific needs. State Regulation and 3rd Party Reimbursement Explain the significance of state regulation for the athletic training profession and its relationship to 3rd party reimbursement. The Impact of Insurance and 3rd Party Reimbursement Explain the impact that insurance and 3rd party reimbursement has on athletic training. Emergency Plans Be able to develop emergency plans for athletic training settings. Negligence Explain the elements of negligence and to understand legal issues facing athletic trainers, as well as the role of risk management. Pre-Participation Exams Explain how to efficiently and effectively organize pre-participation exams. 112 BYU Athletic Training Procedures and Appendix Personnel Management Explain key concepts in personnel management, including communication, motivation, evaluations, e Technology and Information Management Explain the role of technology and information management in athletic training settings. Leadership Skills Develop and incorporate individual leadership skills; as well as increase personal awareness, gain self-confidence, and foster cohesive and caring relationships EXSC 460 Fundamentals of body mechanics and therapeutic exercise, coupled with kinesiological principles for detection and correction of basic neuromusculoskeletal anomalies Outcomes: Basic Othopedic Terminology Upon completion of this class students will be able to accomplish the following: Demonstrate an understanding of basic orthopedic terminology dealing with posture, movement and pathology. Osteokinematic and Arthrokinematic Movement Demonstrate an understanding of traditional, osteokinematic and arthrokinematic movement Therapeutic Exercise Demonstrate an understanding of therapeutic exercise particularly active-resistive exercise and manual muscle testing and manual passive exercise and stretching. Postural Evaluation Be able to perform a postural evaluation, both grossly and at individual joints Etiology Demonstrate an understanding of the etiology, clinical significance and treatment of congenital and acquired orthopedic impairments of the upper and lower extremities and trunk. Writing Therapeutic Exercise Programs Where applicable, be able to write a therapeutic exercise program for the orthopedic impairments discussed in class. Normal and Pathologic Gait Demonstrate an understanding of normal and pathologic gait. EXSC 463 The function of the physiological systems and their responses to acute and chronic exercise Outcomes: Anaerobic and Aerobic Metabolic Pathways the substrates used, amount and rate of ATPresynthesized, metabolic end products, and controlof anaerobic and aerobic metabolic pathways. Physical Conditioning the responses to acute bouts of exercise and themechanisms of the observed response, and thephysiological adaptations which occur as a resultof physical conditioning. Principles of Physical Conditioning the physiological rationale for applying the eight principles of physical conditioning to improve health, fitness, and performance. Depolarization of Skeletal Muscle the depolarization of skeletal muscle beginning atthe spinal cord and ending with the contraction ofthe muscle fiber. Transportation and Diffusion of O2 and CO2 the transportation and diffusion of O2 and CO2through the pulmonary and systemic circuits atrest and during exercise. Skeletal Muscle Fiber Types the physiological and functional differences between the three skeletal muscle fiber types. Restand Interaction the interaction of the nervous, muscle, cardiovascular,pulmonary, and metabolic systems at restand during exercise. Cardiovascular System the normal anatomy and physiology of the heart, blood, and blood vessels. Describe the normal function of the cardiovascular system at rest and during exercise. Appreciation for How the Human Body Functions You will gain a greater appreciation for how thehuman body functions during the increased metabolicdemands of exercise. During this course youwill study the nervous, muscle, cardiovascular,pulmonary, and metabolic systems and their integration.This course takes an incremental approach tothe study of exercise physiology. By the end of thiscourse, you should be able to describe• the function of sympathetic, parasympathetic, andsomatic motor neurons, including differences instructure, neurotransmitters, receptors and efferentorgans. 113 BYU Athletic Training Procedures and Appendix EXSC 464 Introduction of laboratory and field methods; applying principles of exercise physiology to assessing physical fitness and physiological responses to exercise Outcomes: Applying Knowledge of Exercise Physiology The purpose of this class is to apply knowledge of exercise physiology to the assessment of the five components of health related physical fitness. The labs are the means to review and apply the physiology of exercise and to develop and practice fundamental skills related to the assessment of physical fitness. EXSC 468 Applying scientific principles to problems in conditioning Outcomes: Writing Prescriptions of Activity At the conclusion of the course, the student will be able to write prescriptions of activity for individuals of selected levels of age and fitness for the following: A. Endurance 1. Speed/Explosive endurance 2. Anaerobic endurance 3. Aerobic endurance B. Strength 1. Beginners 2. Athletes 3. Body builders C. Nutrition D. Weight Control 1. Weight loss 2. Weight gain E. Flexibility F. Plyometricssion of the course, the student will be able to write prescriptions of activity for EXSC 494 Classroom and field experience. Modules include injury assessment and management, rehabilitation skills, and knowledge of general medical conditions. Outcomes: Administrative Policies and Procedures After completing this course, the student will be able to understand and apply administrative policies and procedures. General Medical Assessment Skills Demonstrate general medical assessment skills. Care and Prevention Understand how to care for and prevent various general medical (respiratory, cardiac, gastric, genitourinary) pathologies. EXSC 495 Classroom and field experience. Modules include injury assessment and management, rehabilitation skills, nutrition, and dermatology. Outcomes: Pharmacology After completing this course, the student will: Demonstrate understanding of pharmacology, pharmacological processes, and the university‘s medication policies and procedures. Basic Nutrition Guidelines Demonstrate knowledge of basic nutrition guidelines for athletes. Eating Disorders Demonstrate knowledge of eating disorders and disordered eating and possess the ability to intervene with athletes who suffer from such disorders. Upper Extremity Injuries Demonstrate the skills necessary to properly evaluate, care for, rehabilitate, and prevent upper extremity injuries. General Medical Pathologies 114 BYU Athletic Training Procedures and Appendix Demonstrate the skills necessary to properly evaluate, care for, and prevent various general medical (common syndromes and diseases, dermatology) pathologies. EXSC 498 Synthesizing and integrating student classroom and clinical experiences in preparation for BOC examination resulting in certification of allied health professionals. Outcomes: BOC Exam Registration Process Explain, describe and complete the BOC exam registration process. Exam Preparation Schedule Design and follow athletic training content exam preparation schedule. Possibilities of Practice in AT Understand the possibilities of practice in AT. Significance of BOC Certification Explain the significance of BOC certification and state regulation for the athletic training profession. Deficiencies in Knowledge and Skills Define deficiencies in you athletic training education knowledge and skills. Emergency Plans Develop and implement emergency plans in the practice of athletic training Legal Issues Explain legal issues facing athletic trainers. Technology and Information Management Explain the role of technology and information management in athletic training settings. Requirements to Maintain BOC Certification Understand the requirements to maintain BOC certification. NATA Education Council Competencies Have completed all NATA Education Council competencies. EXSC 501 Sports medicine pathologies and related pharmacology for a variety of sports medicine/allied health care professions. NOTE: Meets required NATA athletic training educational competencies. Outcomes: Basic Knowledge of Human Anatomy and Physiology After completing this course, the student will:1. Synthesize basic knowledge of human anatomy and physiology to develop knowledge of the causes, pathophysiology, and clinical features of the various conditions affecting the body. Considering you have completed a physiology course you will be required to recall that information Pharmacokinetics and Pharmacodynamics Principles Understand basic pharmacokinetics and pharmacodynamics principles. Administration of Prescription and Nonprescription Drugs Describe proper maintenance and documentation of records for the administration of prescription and nonprescription drugs. Routes Used to Administer Medications Understand advantages and disadvantages of common routes used to administer medications. Pharmacological Intervention Analyze relationships between inflammation, repair, regeneration, and healing as they relate to pharmacological intervention. Reference Sources for Pharmacological Information Utilize reference sources for pharmacological information. Patient Information for Prescription and Nonprescription Age Synthesize patient information for prescription and nonprescription agents associated with the treatment and relief of symptoms from illness and injuries. Clinical use of Various Prescription and Nonprescription Age Understand clinical use of various prescription and nonprescription agents associated with the treatment and relief of symptoms from illnesses and injuries. Clinico-Pathological Signs and Symptoms Evaluate clinico-pathological signs and symptoms for specific medical conditions that assist the sport medicine/allied health care clinician in correlating findings in determining the course of action for illness and disease Current Banned-Drug Lists Identify sources of current banned-drug lists published by various associations. 115 BYU Athletic Training Procedures and Appendix Drug Testing and Screening Program Describe basic concepts of organizing and coordinating a drug testing and screening program. HLTH 320 In-depth coverage of first aid procedures for injuries and sudden illness. Leads to first aid and CPR certifications. Outcomes: CPR, AED, Bandaging, and Splinting Demonstrate the skills involving cardiopulmonary rescuitation (CPR), automated external defibrillation (AED), bandaging, and splinting. Importance of First Aid Identify the importance of first aid and emergency care Emergency Problems Recognize specific emergency problems (i.e., heart attack, fracture, open wound, burn insect sting) through their signs and symptoms. Emergency Decisions Identify the decisions involved during an emergency. First Aid and Emergency Care Procedures Describe proper first aid and emergency care procedures for specific emergency problems. MMBIO 221 Microbial world, emphasizing communicable diseases, their causes and control. NDFS 310 Scientific basis for the role of nutrition in human performance. Critical evaluation of popular practices; making optimal food choices for physical activity. Outcomes: Nutrition and Physical Performance Students will apply their current understanding of nutrition to aspects of physical performance. Scientific Research and Evaluation Demonstrate ability to search, interpret, and summarize original scientific information. Evaluate nutritional claims for scientific accuracy Evidence-based Nutrition Recommendations Demonstrate knowledge of evidence-based nutrition recommendations. Critical Thinking and Data Analysis Demonstrate critical thinking skills in problem identification and data analysis, and in recognizing the implications of decisions. Sports Nutrition Evaluation Develop critical thinking skills in evaluating nutritional claims regarding sports performance Energy Systems Describe the factors (exercise intensity, duration, substrate availability, and endocrine) that affect the ability of the body to utilize energy systems. PDBIO 220 Structure and function of the human body. Lab included Outcomes: Body Organs and Organ Systems Students will be able to list the name, location, and function of each of the body‘s organs and organ systems. Tissue Structures Students will demonstrate an understanding of the basic microscopic underpinnings of tissue structures and be able to name them. Appreciating the Human Body Students will demonstrate a greater understanding and appreciation for the human body, it‘s overall design and connections to other living organisms, and what a marvelous creation it is. PDBIO 305 Function of body organ systems. PSYCH 111 Basic course in modern scientific psychology. Outcomes: Knowledge of theoretical perspectives Objective: Demonstrate a broad knowledge of the basic theoretical perspectives that guide psychological inquiry. 116 BYU Athletic Training Procedures and Appendix Measurement:Examinations, quizzes, comprehensive final examination that includes questions common to all Psychology 111 sections. Applying psychological principles Objective: Apply psychological principles to personal and social issues and problems. Measurement:Examinations, quizzes, comprehensive final examination that includes questions common to all Psychology 111 sections, response papers to essays written by practicing research psychologists or term paper. Research methods Objective: Understand the basic research methods used in psychology, including classical and current experiments. Measurement:Examinations, quizzes, comprehensive final examination that includes questions common to all Psychology 111 sections, response papers to essays written by practicing research psychologists or term paper, participation as a subject in actual psychological research. STAT 221 Stemplots, boxplots, histograms, scatterplots; central tendency, variability; confidence intervals and hypothesis testing involving one and two means and proportions; contingency tables, simple linear regression. STDEV 170 Overview of health professions: medical, dental, and other specialties. Primary focus on guest lectures from various practitioners and clinicians. Outcomes: Gain a basic understanding of a significant number of health professions. Increase knowledge of health professions through conversing with health care professionals. Learn more about health care provision through service learning in preparation for service-oriented health professions. Increase awareness of the requirements to enter various health professions and where to find additional information about their preferred health care field. Links to Requirements MAP 117 BYU Athletic Training Procedures and Appendix APPENDIX F Competencies and Clinical Proficiencies 118 BYU Athletic Training Procedures and Appendix Competency Code Competency EBP Evidence Based Practice EBP-1 EBP-2 Define evidence-based practice as it relates to athletic training clinical practice. Explain the role of evidence in the clinical decision making process. EBP-3 Describe and differentiate the types of quantitative and qualitative research, research components, and levels of research evidence. EBP-4 Describe a systematic approach (eg, five step approach) to create and answer a clinical question through review and application of existing research. EBP-5 Develop a relevant clinical question using a pre-defined question format (eg, PICO= Patients, Intervention, Comparison, Outcomes; PIO = Patients, Intervention, Outcomes). EBP-6 Describe and contrast research and literature resources including databases and online critical appraisal libraries that can be used for conducting clinically-relevant searches EBP-7 Conduct a literature search using a clinical question relevant to athletic training practice using search techniques (eg, Boolean search, Medical Subject Headings) and resources appropriate for a specific clinical question. EBP-9 Use standard criteria or developed scales (eg, Physiotherapy Evidence Database Scale [PEDro], Oxford Centre for Evidence Based Medicine Scale) to critically appraise the structure, rigor, and overall quality of research studies. EBP-10 Determine the effectiveness and efficacy of an athletic training intervention utilizing evidence-based practice concepts. EBP-11 Explain the theoretical foundation of clinical outcomes assessment (eg, disablement, health-related quality of life) and describe common methods of outcomes assessment in athletic training clinical practice (generic, diseasespecific, region-specific, and dimension-specific outcomes instruments). EBP-12 Describe the types of outcomes measures for clinical practice (patient-based and clinician-based) as well as types of evidence that are gathered through outcomes assessment (patient-oriented evidence versus disease-oriented evidence). EBP-13 Understand the methods of assessing patient status and progress (eg, global rating of change, minimal clinically important difference, minimal detectable difference) with clinical outcomes assessments. Apply and interpret clinical outcomes to assess patient status, progress, and change using psychometrically sound outcome instruments. EBP-14 PHP Prevention and Health Promotion PHP-1 Describe the concepts (eg, case definitions, incidence versus prevalence, exposure assessment, rates) and uses of injury and illness surveillance relevant to athletic training. 119 BYU Athletic Training Procedures and Appendix PHP-2 Identify and describe measures used to monitor injury prevention strategies (eg, injury rates and risks, relative risks, odds ratios, risk differences, numbers needed to treat/harm). PHP-3 Indentify modifiable/non-modifiable risk factors and mechanisms for injury and illness. PHP-4 Explain how the effectiveness of a prevention strategy can be assessed using clinical outcomes, surveillance, or evaluation data. PHP-5 Explain the precautions and risk factors associated with physical activity in persons with common congenital and acquired abnormalities, disabilities, and diseases. PHP-6 Summarize the epidemiology data related to the risk of injury and illness associated with participation in physical activity. PHP-7 Implement disinfectant procedures to prevent the spread of infectious diseases and to comply with Occupational Safety and Health Administration (OSHA) and other federal regulations. PHP-8 Identify the necessary components to include in a preparticipation physical examination as recommended by contemporary guidelines (eg, American Heart Association, American Academy of Pediatrics Council on Sports Medicine & Fitness). PHP-9 Explain the role of the preparticipation physical exam in identifying conditions that might predispose the athlete to injury or illness. PHP-10 Explain the principles of the body’s thermoregulatory mechanisms as they relate to heat gain and heat loss. PHP-11 Explain the principles of environmental illness prevention programs to include acclimation and conditioning, fluid and electrolyte replacement requirements, proper practice and competition attire, hydration status, and environmental assessment (eg, sling psychrometer, wet bulb globe temperatures [WBGT], heat index guidelines). PHP-12 Summarize current practice guidelines related to physical activity during extreme weather conditions (eg, heat, cold, lightning, wind). PHP-13 Obtain and interpret environmental data (web bulb globe temperature [WBGT], sling psychrometer, lightning detection devices) to make clinical decisions regarding the scheduling, type, and duration of physical activity. PHP-14 Assess weight loss and hydration status using weight charts, urine color charts, or specific gravity measurements to determine an individual’s ability to participate in physical activity in a hot, humid environment. PHP-15 Use a glucometer to monitor blood glucose levels, determine participation status, and make referral decisions. PHP- 16 Use a peak-flow meter to monitor a patient’s asthma symptoms, determine participation status, and make referral decisions. 120 BYU Athletic Training Procedures and Appendix PHP-17 Explain PHP-17. Explain the etiology and prevention guidelines associated with the leading causes of sudden death during physical activity, including but not limited to: PHP-17i. Lightning strike PHP-17a. Cardiac arrhythmia or arrest PHP-17b. Asthma PHP-17c. Traumatic brain injury PHP-17d. Exertional heat stroke PHP-17e. Hyponatremia PHP-17f. Exertional sickling PHP-17g. Anaphylactic shock PHP-17h. Cervical spine injury PHP-17i. Lightning strike PHP-18 Explain strategies for communicating with coaches, athletes, parents, administrators, and other relevant personnel regarding potentially dangerous conditions related to the environment, field, or playing surfaces. PHP-19 Instruct clients/patients in the basic principles of ergodynamics and their relationship to the prevention of illness and injury. PHP-20 Summarize the basic principles associated with the design, construction, fit, maintenance, and reconditioning of protective equipment, including the rules and regulations established by the associations that govern its use. PHP-21 Summarize the principles and concepts related to the fabrication, modification, and appropriate application or use of orthotics and other dynamic and static splints. PHP-22 Fit standard protective equipment following manufacturers’ guidelines. PHP-23 Apply preventive taping and wrapping procedures, splints, braces, and other special protective devices. PHP-24 Summarize the general principles of health maintenance and personal hygiene, including skin care, dental hygiene, sanitation, immunizations, avoidance of infectious and contagious diseases, diet, rest, exercise, and weight control. PHP-25 Describe the role of exercise in maintaining a healthy lifestyle and preventing chronic disease. PHP-26 Indentify and describe the standard tests, test equipment, and testing protocols that are used for measuring fitness, body composition, posture, flexibility, muscular strength, power, speed, agility, and endurance. PHP-27 Compare and contrast the various types of flexibility, strength training, and cardiovascular conditioning programs to include expected outcomes, safety precautions, hazards, and contraindications. Add activites for AT? 121 BYU Athletic Training Procedures and Appendix PHP-28 Adminster and interpret fitness tests to assess a client’s/patient’s physical status and readiness for physical activity. PHP-29 Explain the basic concepts(clarify) and practice (of fitness and wellness screening). Y-BE-Fit? PHP-30 Design a fitness program to meet the individual needs of a client/patient based on the results of standard fitness assessments and wellness screening. Health Promotion? PHP-31 Instruct a client/patient regarding fitness exercises and the use of muscle strengthening equipment to include correction or modification of inappropriate, unsafe, or dangerous lifting techniques. Add Activities for AT? PHP-32 Describe the role of nutrition in enhancing performance, preventing injury or illness, and maintaining a healthy lifestyle. PHP-33 Educate clients/patients on the importance of healthy eating, regular exercise, and general preventative strategies for improving or maintaining health and quality of life. Health Promotion Class PHP-34 Describe contemporary nutritional intake recommendations and explain how these recommendations can be used in performing a basic dietary analysis and providing appropriate general dietary recommendations. PHP-35 Describe the proper intake, sources of, and effects of micro- and macronutrients on performance, health, and disease. PHP-36 Describe current guidelines for proper hydration and explain the consequences of improper fluid/electrolyte replacement. PHP-37 Identify, analyze, and utilize the essential components of food labels to determine the content, quality, and appropriateness of food products. PHP-38 Describe nutritional principles that apply to tissue growth and repair. PHP-39 Describe changes in dietary requirements that occur as a result of changes in an individual’s health, age, and activity level. PHP-40 Explain the physiologic principles and time factors associated with the design and planning of pre-activity and recovery meals/snacks and hydration practices. PHP-41 Identify the foods and fluids that are most appropriate for pre-activity, activity, and recovery meals/snacks. PHP-42 Explain how changes in the type and intensity of physical activity influence the energy and nutritional demands placed on the client/patient. PHP-43 Describe the principles and methods of body composition assessment to assess a client’s/ patient’s health status and to monitor changes related to weight management, strength training, injury, disordered eating, menstrual status, and/or bone density status. ? PHP-44 PHP-45 Assess body composition by validated techniques. Describe contemporary weight management methods and strategies needed to support activities of daily life and physical activity. Health Promotion 122 BYU Athletic Training Procedures and Appendix PHP-46 Identify and describe the signs, symptoms, physiological, and psychological responses of clients/patients with disordered eating or eating disorders. PHP-47 Describe the method of appropriate management and referral for clients/patients with disordered eating or eating disorders in a manner consistent with current practice guidelines. PHP-48 Explain the known usage patterns, general effects, and short- and long-term adverse effects for the commonly used dietary supplements, performance enhancing drugs, and recreational drugs. PHP-49 Identify which therapeutic drugs, supplements, and performance-enhancing substances are banned by sport and/or workplace organizations in order to properly advise clients/patients about possible disqualification and other consequences CE Clinical Examination and Diagnosis CE-1 Describe the normal structures and interrelated functions of the body systems. CE-2 Describe the normal anatomical, systemic, and physiological changes associated with the lifespan. CE-3 Identify the common congenital and acquired risk factors and causes of musculoskeletal injuries and common illnesses that may influence physical activity in pediatric, adolescent, adult, and aging populations. CE-4 Describe the principles and concepts of body movement, including normal osteokinematics and arthrokinematics. CE-5 Describe the influence of pathomechanics on function. CE-6 Describe the basic principles of diagnostic imaging and testing and their role in the diagnostic process. EBM/EBP? CE-7 Identify the patient’s participation restrictions (disabilities) and activity limitations (functional limitations) to determine the impact of the condition on the patient’s life. CE-8 Explain the role and importance of functional outcome measures in clinical practice and patient health-related quality of life. CE-9 Identify functional and patient-centered quality of life outcome measures appropriate for use in athletic training practice. CE-10 Explain diagnostic accuracy concepts including reliability, sensitivity, specificity, likelihood ratios, prediction values, and pre-test and post-test probabilities in the selection and interpretation of physical examination and diagnostic procedures. EBP CE-11 Explain the creation of clinical prediction rules in the diagnosis and prognosis of various clinical conditions CE-12 Apply clinical prediction rules (eg, Ottawa Ankle Rules) during clinical examination procedures. CE-13 Obtain a thorough medical history that includes the pertinent past medical history, underlying systemic disease, use of medications, the patient’s perceived pain, and the history and course of the present condition 123 BYU Athletic Training Procedures and Appendix CE-14 Differentiate between an initial injury evaluation and follow-up/reassessment as a means to evaluate the efficacy of the patient's treatment/rehabilitation program, and make modifications to the patient's program as needed. CE-15 Demonstrate the ability to modify the diagnostic examination process according to the demands of the situation and patient responses. CE-16 Recognize the signs and symptoms of catastrophic and emergent conditions and demonstrate appropriate referral decisions. CE-17 Use clinical reasoning skills to formulate an appropriate clinical diagnosis for common illness/disease and orthopedic injuries/conditions. CE-18 Incorporate the concept of differential diagnosis into the examination process. CE-19 Determine criteria and make decisions regarding return to activity and/or sports participation based on the patient’s current status. CE-20 Use standard techniques and procedures for the clinical examination of common injuries, conditions, illnesses, and diseases including, but not limited to: CE-20a. history taking CE-20b. inspection/observation CE-20c. palpation CE-20d. functional assessment CE-20e. selective tissue testing techniques / special tests CE-20f. neurological assessments (sensory, motor, reflexes, balance, cognitive function) CE-20g. respiratory assessments (auscultation, percussion, respirations, peakflow) CE-20h. circulatory assessments (pulse, blood pressure, auscultation) CE-20i. abdominal assessments (percussion, palpation, auscultation) CE-20j. other clinical assessments (otoscope, urinalysis, glucometer, temperature, opthalmoscope) CE-21 Assess interpret findings from a physical examination that is based on the patient’s clinical presentation. This exam can include: CE-21a. Assessment of posture, gait, and movement patterns CE-21b. Palpation CE-21c. Muscle function assessment CE-21d. Assessment of quantity and quality of osteokinematic joint motion CE-21e. Capsular and ligamentous stress testing CE-21f. Joint play (arthrokinematics) CE-21g. Selective tissue examination techniques / special tests CE-21h. Neurologic function (sensory, motor, reflexes, balance, cognition) CE-21i. Cardiovascular function (including differentiation between normal and abnormal heart sounds, blood pressure, and heart rate) 124 BYU Athletic Training Procedures and Appendix CE-21j. Pulmonary function (including differentiation between normal breath sounds, percussion sounds, number and characteristics of respirations, peak expiratory flow) CE-21k. Gastrointestinal function (including differentiation between normal and abnormal bowel sounds) CE-21l. Genitourinary function (urinalysis) CE-21m. Ocular function (vision, ophthalmoscope).. CE-22 CE-21n. Function of the ear, nose, and throat (including otoscopic evaluation) CE-21o. Dermatological assessment CE-21p. Other assessments (glucometer, temperature) Determine when the findings of an examination warrant referral of the patient. CE-23 Describe current setting-specific (eg, high school, college) and activity-specific rules and guidelines for managing injuries and illnesses. AC Acute Care of Injuries and Illnesses AC-1 Explain the legal, moral, and ethical parameters that define the athletic trainer's scope of acute and emergency care. Differentiate the roles and responsibilities of the athletic trainer from other prehospital care and hospital-based providers, including emergency medical technicians/paramedics, nurses, physician assistants, and physicians. AC-2 AC-3 Describe the hospital trauma level system and its role in the transportation decision-making process. AC-4 Demonstrate the ability to perform scene, primary, and secondary surveys. AC-5 Obtain a medical history appropriate for the patient’s ability to respond. AC-6 When appropriate, obtain and monitor signs of basic body functions including pulse, blood pressure, respiration, pulse oximetry, pain, and core temperature. Relate changes in vital signs to the patient’s status. AC-7 Differentiate between normal and abnormal physical findings (eg, pulse, blood pressure, heart and lung sounds, oxygen saturation, pain, core temperature) and the associated pathophysiology. AC-8 Explain the indications, guidelines, proper techniques, and necessary supplies for removing equipment and clothing in order to access the airway, evaluate and/or stabilize an athlete’s injured body part. AC-9 Differentiate the types of airway adjuncts (oropharygneal airways [OPA], nasopharyngeal airways [NPA] and supraglottic airways [King LT-D or Combitube]) and their use in maintaining a patent airway in adult respiratory and/or cardiac arrest. Establish and maintain an airway, including the use of oro- and nasopharygneal airways, and neutral spine alignment in an athlete with a suspected spine injury who may be wearing shoulder pads, a helmet with and without a face guard, or other protective equipment. Determine when suction for airway maintenance is indicated and use according to accepted practice protocols. AC-10 AC-11 125 BYU Athletic Training Procedures and Appendix AC-12 AC-13 Identify cases when rescue breathing, CPR, and/or AED use is indicated according to current accepted practice protocols. Utilize an automated external defibrillator (AED) according to current accepted practice protocols. AC-14 Perform one- and two- person CPR on an infant, child and adult. AC-15 Utilize a bag valve and pocket mask on a child and adult using supplemental oxygen. AC-16 Explain the indications, application, and treatment parameters for supplemental oxygen administration for emergency situations. AC-17 Adminster supplemental oxygen with adjuncts (eg, non-rebreather mask, nasal cannula). AC-18 Assess oxygen saturation using a pulse oximeter and interpret the results to guide decision making. AC-19 Explain the proper procedures for managing external hemorrhage (eg, direct pressure, pressure points, tourniquets) and the rationale for use of each. AC-20 Select and use the appropriate procedure for managing external hemorrhage. AC-21 Explain aseptic or sterile techniques, approved sanitation methods, and universal precautions used in the cleaning, closure, and dressing of wounds. AC-22 Select and and use appropriate procedures for the cleaning, closure, and dressing of wounds, identifying when referral is necessary. AC-23 Use cervical stabilization devices and techniques that are appropriate to the circumstances of an injury. AC-24 Demonstrate proper positioning and immobilization of a patient with a suspected spinal cord injury. AC-25 Perform patient transfer techniques for suspected head and spine injuries utilizing supine log roll, prone log roll with push, prone log roll with pull, and liftand-slide techniques. AC-26 Select the appropriate spine board, including long board or short board, and use appropriate immobilization techniques based on the circumstance of the patient’s injury. AC-27 Explain the role of core body temperature in differentiating between exertional heat stroke, hyponatremia, and head injury. AC-28 Differentiate the different methods for assessing core body temperature. AC-29 AC-30 Assess core body temperature using a rectal probe Explain the role of rapid full body cooling in the emergency management of exertional heat stroke. AC-31 Assist the patient in the use of a nebulizer treatment for an asthmatic attack. AC-32 Determine when use of a metered-dose inhaler is warranted based on a patient’s condition. AC-33 Instruct a patient in the use of a meter-dosed inhaler in the presence of asthmarelated bronchospasm. 126 BYU Athletic Training Procedures and Appendix AC-34 Explain the importance of monitoring a patient following a head injury, including the role of obtaining clearance from a physician before further patient participation. AC-35 Demonstrate the use of an auto-injectable epinephrine in the management of allergic anaphylaxis. Decide when auto-injectable epinephrine use is warranted based on a patient’s condition. AC-36 Identify the signs, symptoms, interventions and, when appropriate, the return-toparticipation criteria for: AC-36a. sudden cardiac arrest AC-36b. brain injury including concussion, subdural and epidural hematomas, second impact syndrome and skull fracture AC-36c. cervical, thoracic, and lumbar spine trauma AC-36d. heat illness including heat cramps, heat exhaustion, exertional heat stroke, and hyponatremia AC-36e. exertional sickling associated with sickle cell trait AC-36f. Rhabdomyolysis AC-36g. internal hemorrhage AC-36h. diabetic emergencies including hypoglycemia and ketoacidosis AC-37 AC-36i. asthma attacks AC-36j. systemic allergic reaction, including anaphylactic shock AC-36k. epileptic and non-epileptic seizures AC-36l. Shock AC-36m. hypothermia, frostbite AC-36n. toxic drug overdoses AC-36o. local allergic reaction Select and apply appropriate splinting material to stabilize an injured body area. AC-38 Apply appropriate immediate treatment to protect the injured area and minimize the effects of hypoxic and enzymatic injury. AC-39 Select and implement the appropriate ambulatory aid based on the patient’s injury and activity and participation restrictions. AC-40 Determine the proper transportation technique based on the patient’s condition and findings of the immediate examination. Identify the criteria used in the decision-making process to transport the injured patient for further medical examination. AC-41 AC-42 Select and use the appropriate short-distance transportation methods, such as the log roll or lift and slide, for an injured patient in different situations. AC-43 Instruct the patient in home care and self-treatment plans for acute conditions. 127 BYU Athletic Training Procedures and Appendix TI Therapeutic Interventions TI-1 Describe and differentiate the physiological and pathophysiological responses to inflammatory and non-inflammatory conditions and the influence of these responses on the design, implementation, and progression of a therapeutic intervention. TI-2 Compare and contrast contemporary theories of pain perception and pain modulation. TI-3 Differentiate between palliative and primary pain-control interventions. TI-4 Analyze the impact of immobilization, inactivity, and mobilization on the body systems (eg, cardiovascular, pulmonary, musculoskeletal) and injury response. TI-5 Compare and contrast the variations in the physiological response to injury and healing across the lifespan. TI-6 Describe common surgical techniques, including interpretation of operative reports, and any resulting precautions, contraindications, and comorbidities that impact the selection and progression of a therapeutic intervention program. TI-7 Identify patient- and clinician-oriented outcomes measures commonly used to recommend activity level, make return to play decisions, and maximize patient outcomes and progress in the treatment plan. TI-8 Explain the theory and principles relating to expected physiological response(s) during and following therapeutic interventions. TI-9 Describe the laws of physics that (1) underlay the application of thermal, mechanical, electromagnetic, and acoustic energy to the body and (2) form the foundation for the development of therapeutic interventions (eg, stress-strain, leverage, thermodynamics, energy transmission and attenuation, electricity TI-10 Integrate self-treatment into the intervention when appropriate, including instructing the patient regarding self-treatment plans. TI-11 Design therapeutic interventions to meet specified treatment goals. TI-11a. Assess the patient to identify indications, contraindications, and precautions applicable to the intended intervention. TI-11b. Position and prepare the patient for various therapeutic interventions. TI-11c. Describe the expected effects and potential adverse reactions to the patient. TI-11d. Instruct the patient how to correctly perform rehabilitative exercises. TI-11e. Apply the intervention, using parameters appropriate to the intended outcome. TI-11f. Reassess the patient to determine the immediate impact of the intervention. TI-12 Use the results of on-going clinical examinations to determine when a therapeutic intervention should be progressed, regressed or discontinued. 128 BYU Athletic Training Procedures and Appendix TI-13 Describe the relationship between the application of therapeutic modalities and the incorporation of active and passive exercise and/or manual therapies, including therapeutic massage, myofascial techniques, and muscle energy techniques. TI-14 Describe the use of joint mobilization in pain reduction and restoration of joint mobility. TI-15 Perform joint mobilization techniques as indicated by examination findings. TI-16 Fabricate and apply taping, wrapping, supportive, and protective devices to facilitate return to function. TI-17 Analyze gait and select appropriate instruction and correction strategies to facilitate safe progression to functional gait pattern. TI-18 Explain the relationship between posture, biomechanics, and ergodynamics and the need to address these components in a therapeutic intervention. TI-19 Identify manufacturer, institutional, state, and/or federal standards that influence approval, operation, inspection, maintenance and safe application of therapeutic modalities and rehabilitation equipment. TI-20 Inspect therapeutic equipment and the treatment environment for potential safety hazards. TI-21 Explain the federal, state, and local laws, regulations and procedures for the proper storage, disposal, transportation, dispensing (administering where appropriate), and documentation associated with commonly used prescription and nonprescription medications TI-22 Identify and use appropriate pharmaceutical terminology for management of medications, inventory control, and reporting of pharmacological agents commonly used in an athletic training facility. TI-23 Use an electronic drug resource to locate and identify indications, contraindications, precautions, and adverse reactions for common prescription and nonprescription medications. TI-24 Explain the major concepts of pharmacokinetics and the influence that exercise might have on these processes. TI-25 Explain the concepts related to bioavailability, half-life, and bioequivalence (including the relationship between generic and brand name drugs) and their relevance to the patient, the choice of medication, and the dosing schedule. TI-26 Explain the pharmacodynamic principles of receptor theory, dose-response relationship, placebo effect, potency, and drug interactions as they relate to the mechanism of drug action and therapeutic effectiveness. TI-27 Describe the common routes used to administer medications and their advantages and disadvantages. TI- 28 Properly assist and/or instruct the patient in the proper use, cleaning, and storage of drugs commonly delivered by metered dose inhalers, nebulizers, insulin pumps, or other parenteral routes as prescribed by the physician. Nurses equipment? 129 BYU Athletic Training Procedures and Appendix TI-29 Describe how common pharmacological agents influence pain and healing and their influence on various therapeutic interventions. TI-30 Explain the general therapeutic strategy, including drug categories used for treatment, desired treatment outcomes, and typical duration of treatment, for the following common diseases and conditions: asthma, diabetes, hypertension, infections, depression, GERD, allergies, pain, inflammation, and the common cold. TI-31 Optimize therapeutic outcomes by communicating with patients and/or appropriate healthcare professionals regarding compliance issues, drug interactions, adverse drug reactions, and sub-optimal therapy. PS Psychosocial Strategies and Referral PS-1 Describe the basic principles of personality traits, trait anxiety, locus of control, intrinsic and extrinsic motivation, and patient and social environment interactions as they affect patient interactions. PS-2 Explain xplain the theoretical background of psychological and emotional responses to injury and forced inactivity (eg, cognitive appraisal model, stress response model). PS-3 Describe how psychosocial considerations affect clinical decision-making related to return to activity or participation (eg, motivation, confidence). PS-4 Summarize and demonstrate the basic processes of effective interpersonal and cross-cultural communication as it relates to interactions with patients and others involved in the healthcare of the patient. PS-5 Summarize contemporary theory regarding educating patients of all ages and cultural backgrounds to effect behavioral change. PS-6 Explain the importance of educating patients, parents/guardians, and others regarding the condition in order to enhance the psychological and emotional well-being of the patient. PS-7 Describe the psychological techniques (eg, goal setting, imagery, positive self-talk, relaxation/anxiety reduction) that the athletic trainer can use to motivate the patient during injury rehabilitation and return to activity processes. PS-8 Describe psychological interventions (eg, goal setting, motivational techniques) that are used to facilitate a patient's physical, psychological, and return to activity needs. PS-9 Describe the psychosocial factors that affect persistent pain sensation and perception (eg, emotional state, locus of control, psychodynamic issues, sociocultural factors, personal values and beliefs) and identify multidisciplinary approaches for assisting patients with persistent pain. PS-10 Explain the impact of sociocultural issues that influence the nature and quality of healthcare received (eg, cultural competence, access to appropriate healthcare providers, uninsured/underinsured patients, insurance) and formulate and implement strategies to maximize client/patient outcomes. PS-11 Describe the role of various mental healthcare providers (eg, psychiatrists, psychologists, counselors, social workers) that may comprise a mental health referral network. 130 BYU Athletic Training Procedures and Appendix PS-12 Identify and refer clients/patients in need of mental healthcare. PS-13 Identify and describe the basic signs and symptoms of mental health disorders (eg, psychosis, neurosis; sub-clinical mood disturbances (eg, depression, anxiety); and personal/social conflict (eg, adjustment to injury, family problems, academic or emotional stress, personal assault or abuse, sexual assault or harassment) that may indicate the need for referral to a mental healthcare professional. PS-14 Describe the psychological and sociocultural factors associated with common eating disorders. PS-15 Identify the symptoms and clinical signs of substance misuse/abuse, the psychological and sociocultural factors associated with such misuse/abuse, its impact on an individual’s health and physical performance, and the need for proper referral to a healthcare professional. PS-16 Formulate a referral for an individual with a suspected mental health or substance abuse problem. PS-17 Describe the psychological and emotional responses to a catastrophic event, the potential need for a psychological intervention and a referral plan for all parties affected by the event. PS-18 Provide appropriate education regarding the condition and plan of care to the patient and appropriately discuss with others as needed and as appropriate to protect patient privacy. HA HA-1 Healthcare Administration Describe the role of the athletic trainer and the delivery of athletic training services within the context of the broader healthcare system. HA-2 Describe the impact of organizational structure on the daily operations of a healthcare facility. HA-3 Describe the role of strategic planning as a means to assess and promote organizational improvement. HA-4 Describe the conceptual components of developing and implementing a basic business plan. HA-5 Describe basic healthcare facility design for a safe and efficient clinical practice setting. HA-6 Explain components of the budgeting process including: purchasing, requisition, bidding, request for proposal, inventory, profit and loss ratios, budget balancing, and return on investments. Assess the value of the services provided by an athletic trainer (eg, return on investment). HA-7 HA-8 Develop operational and capital budgets based on a supply inventory and needs assessment; including capital equipment, salaries and benefits, trending analysis, facility cost, and common expenses. HA-9 Identify the components that comprise a comprehensive medical record. HA-10 Identify and explain the statutes that regulate the privacy and security of medical records. 131 BYU Athletic Training Procedures and Appendix HA-11 Use contemporary documentation strategies to effectively communicate with patients, physicians, insurers, colleagues, administrators, and parents or family members. HA-12 Use a comprehensive patient-file management system for appropriate chart documentation, risk management, outcomes, and billing. HA-13 Define state and federal statutes that regulate employment practices. HA-14 Describe principles of recruiting, selecting, hiring, and evaluating employees. HA-15 Identify principles of recruiting, selecting, employing, and contracting with physicians and other medical and healthcare personnel in the deployment of healthcare services. HA-16 Describe federal and state infection control regulations and guidelines, including universal precautions as mandated by the Occupational Safety and Health Administration (OSHA), for the prevention, exposure, and control of infectious diseases, and discuss how they apply to the practicing of athletic training. HA-17 Identify key regulatory agencies that impact healthcare facilities, and describe their function in the regulation and overall delivery of healthcare. HA-18 Describe the basic legal principles that apply to an athletic trainer’s responsibilities. HA-19 Identify components of a risk management plan to include security, fire, electrical and equipment safety, emergency preparedness, and hazardous chemicals. HA-20 Create a risk management plan and develop associated policies and procedures to guide the operation of athletic training services within a healthcare facility to include issues related to security, fire, electrical and equipment safety, emergency preparedness, and hazardous chemicals. HA-21 Develop comprehensive, venue-specific emergency action plans for the care of acutely injured or ill individuals. HA-22 Develop specific plans of care for common potential emergent conditions (eg, asthma attack, diabetic emergency). HA-23 Identify and explain the recommended or required components of a preparticipation examination based on appropriate authorities’ rules, guidelines, and/or recommendations. HA-24 Describe a plan to access appropriate medical assistance on disease control, notify medical authorities, and prevent disease epidemics. HA-25 Describe common health insurance models, insurance contract negotiation, and the common benefits and exclusions identified within these models. HA-26 Describe the criteria for selection, common features, specifications, and required documentation needed for secondary, excess accident, and catastrophic health insurance. Describe the concepts and procedures for revenue generation and reimbursement. HA-27 132 BYU Athletic Training Procedures and Appendix HA-28 Understand the role of and use diagnostic and procedural codes when documenting patient care. HA-29 Explain typical administrative policies and procedures that govern first aid and emergency care. HA-30 Describe the role and functions of various healthcare providers and protocols that govern the referral of patients to these professionals. PD PD-1 Professional Development and Responsibility Summarize the athletic training profession’s history and development and how current athletic training practice has been influenced by its past. PD-2 Describe the role and function of the National Athletic Trainers’ Association and its influence on the profession. PD-3 Describe the role and function of the Board of Certification, the Commission on Accreditation of Athletic Training Education, and state regulatory boards. PD-4 Explain the role and function of state athletic training practice acts and registration, licensure, and certification agencies including (1) basic legislative processes for the implementation of practice acts, (2) rationale for state regulations that govern the practice of athletic training, and (3) consequences of violating federal and state regulatory acts. PD-5 Access, analyze, and differentiate between the essential documents of the national governing, credentialing and regulatory bodies, including, but not limited to, the NATA Athletic Training Educational Competencies, the BOC Standards of Professional Practice, the NATA Code of Ethics, and the BOC Role Delineation Study/Practice Analysis. PD-6 Explain the process of obtaining and maintaining necessary local, state, and national credentials for the practice of athletic training PD-7 Perform a self-assessment of professional competence and create a professional development plan to maintain necessary credentials and promote life-long learning strategies. PD-8 Differentiate among the preparation, scopes of practice, and roles and responsibilities of healthcare providers and other professionals with whom athletic trainers interact. PD-9 Specify when referral of a client/patient to another healthcare provider is warranted and formulate and implement strategies to facilitate that referral. PD-10 Develop healthcare educational programming specific to the target audience (eg, clients/patients, healthcare personnel, administrators, parents, general public). PD-11 Identify strategies to educate colleagues, students, patients, the public, and other healthcare professionals about the roles, responsibilities, academic preparation, and scope of practice of athletic trainers. PD-12 Identify mechanisms by which athletic trainers influence state and federal healthcare regulation. 133 BYU Athletic Training Procedures and Appendix CIP Clinical integration Proficiencies CIP-1.1 1. Administer testing procedures to obtain baseline data regarding a client’s/patient’s level of general health (including (a) nutritional habits, (B) physical activity status, and(C) body composition). CIP-1.2 2.Use this data to design, implement, evaluate, and modify a program specific to the performance and health goals of the patient. This will include instructing the patient in the proper performance of the activities, recognizing the warning signs and symptoms of potential injuries and illnesses that may occur, and explaining the role of exercise in maintaining overall health and the prevention of diseases. CIP-1.3 3. Incorporate contemporary behavioral change theory when educating clients/patients and associated individuals to effect health-related change. CIP-1.4 4. Refer to other medical and health professionals when appropriate. CIP-2.1 1. Select, apply, evaluate, and modify appropriate standard protective equipment,(a) taping, (b) wrapping, (c) bracing, (d) padding, and (e) other custom devices for the client/patient in order to CIP-2.2 2. Prevent and/or minimize the risk of injury to the (a) head, (b) torso, (c)spine, and (d) extremities for safe participation in sport or other physical activity. CIP-3.1 1. Develop, implement, and monitor prevention strategies for at-risk individuals (eg, persons with asthma or diabetes, persons with a previous history of heat illness, persons with sickle cell trait) and large groups to allow safe physical activity in a variety of conditions. CIP-3.2 2. This includes obtaining and interpreting data related to potentially hazardous (a) environmental conditions, (b) monitoring body functions (eg, (c) blood glucose, (d) peak expiratory flow, (e)hydration status), and CIP-3.3 3. Making the appropriate recommendations for individual safety and activity status. CIP-4.1 1. Perform a comprehensive clinical examination of a patient with an (a) upper extremity, (b) lower extremity, (c) head, (d) neck, (e) thorax, and/or (f) spine injury or condition. This exam should incorporate clinical reasoning in the selection of assessment procedures and interpretation of findings in order to formulate a differential diagnosis and/or diagnosis, determine underlying impairments, and identify activity limitations and participation restrictions. CIP-4.2 2. Based on the assessment data and consideration of the patient’s goals, provide the appropriate initial care and establish overall treatment goals. CIP-4.3 3. Create and implement a therapeutic intervention that targets these treatment goals to include, as appropriate, (a) therapeutic modalities, (b) medications (with physician involvement as necessary), and (c) rehabilitative techniques and procedures 134 BYU Athletic Training Procedures and Appendix CIP-4.4 4. Integrate and interpret various forms of standardized documentation including both(a) patient-oriented and clinician-oriented outcomes measures to recommend activity level, (b) make return to play decisions, and (c) maximize patient outcomes and progress in the treatment plan. CIP-5.1 1. Perform a comprehensive clinical examination of a patient with a common illness/condition that includes appropriate(a) clinical reasoning in the selection of assessment procedures and(b) interpretation of history and physical examination findings in order to (c) formulate a differential diagnosis and/or diagnosis. Based on the history, physical examination, and patient goals, implement the appropriate treatment strategy to include medications (with physician involvement as necessary). CIP-5.2 2. Determine whether patient referral is needed, and identify potential restrictions in activities and participation. CIP-5.3 3.Formulate and communicate the appropriate return to activity protocol. CIP-6 1. Clinically evaluate and manage a patient with an emergency injury or condition to include the assessment of (a) vital signs and (b) level of consciousness, (c) activation of emergency action plan, (d) secondary assessment, (e)diagnosis, and (f) provision of the appropriate emergency care (eg, CPR, AED, supplemental oxygen, airway adjunct, splinting, spinal stabilization, control of bleeding). CIP-7 1. Select and and integrate appropriate psychosocial techniques into a patient’s treatment or rehabilitation program to enhance rehabilitation adherence, (a) return to play, and(b) overall outcomes. This includes, but is not limited to, (c) verbal motivation, (d) goal setting, (e) imagery, (f) pain management, (g) self-talk, and/or (h) relaxation. CIP-8 1. Demonstrate the ability to recognize and refer at-risk individuals and individuals with psychosocial disorders and/or mental health emergencies. (a) As a member of the management team, develop an appropriate management plan (including recommendations for patient safety and activity status) (b) that establishes a professional helping relationship with the patient, (e) ensures interactive support and education, and(d) encourages the athletic trainer’s role of informed patient advocate in a manner consistent with current practice guidelines. CIP-9.1 1. Utilize documentation strategies to effectively communicate with: (a) patients, (b) physicians, (c) insurers, (d) colleagues, (e) administrators, and (f) parents or family members while using appropriate terminology and complying with statues that regulate privacy of medical records. CIP-9.2 2. This includes using a comprehensive patient-file management system: (including diagnostic and procedural codes) for (a) appropriate chart documentation, (b) risk management, (c) outcomes, and (d) billing. 135 BYU Athletic Training Procedures and Appendix 136