HITECH Stimulus for Physicians
advertisement

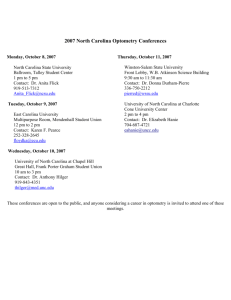
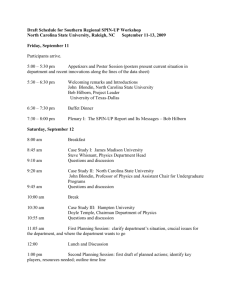
HITECH Stimulus for Physicians Samuel S. Spicer, MD I n response to the economic circumstances occurring in late 2008, on February 17, 2009 President Barack Obama signed in to law the American Recovery and Reinvestment Act of 2009 (ARRA). This act, often referred to as “The Stimulus Act,” appropriated federal expenditures to a variety of projects throughout the economy, with a large portion of the funding being allocated toward infrastructure development (such as road construction). A portion of the funding appropriated under the Act provides health care information technology (HIT) incentives and expands privacy legislation. Title XIII (Section 13001) of that legislation is termed the Health Information Technology for Economic and Clinical Health Act (HITECH) and funds $17.2 billion for incentives and $2 billion for grants. HITECH may be more of a lesson in delayed gratification than a stimulus bill. Incentive payments to physicians participating in Medicare do not start until January of 2011 for meaningful use of certified information systems. Table 1 (page 355) lists the Medicare Part B maximum yearly payments. In 2015, the law directs 1% reductions in the Medicare fee schedule followed by an additional 1% reduction in each of the next two years—2016 and 2017—for physicians who have not satisfied the requirements to qualify. When announcing the HITECH legislation, President Obama promoted an electronic health record (EHR) for all US citizens by 2014. The rationale behind having an EHR is the expectation that it will improve the quality of health care and population health while simultaneously delivering care more efficiently. EHRs have been able to deliver some operational efficiencies inside an integrated delivery network such as Kaiser Permanente1 but the effect of widespread adoption is unknown. A simplified but useful formula for incentive payment requirements is $ = EMR + HIE + QR. An EMR is an electronic medical record that includes electronic prescribing, HIE is a health information exchange which shares medical records, and QR is quality reporting. Most physicians are familiar with the concept of an office EMR and the reporting of National Quality Forum metrics through the Centers for Medicare and Medicaid Services Physician Quality Reporting Initiative. The key to payment depends upon the final definitions of meaningful use and certified.a These definitions will be issued by the Secretary of the Department of Health and Human The North Carolina Medical Board lists over 16,000 licensed physicians practicing in North Carolina. If 50% of these qualify for HITECH funds, it could contribute over $352 million to the state's economy. Services by December 31, 2009. The definitions will be based upon a recommendation by Dr. David Blumenthal, a Harvard physician and professor, who now serves as the national coordinator for the Centers for Medicare and Medicaid Service’s Office of the National Coordinator (ONC) for Health Information Technology. The Congressional Office of Budget and Management has estimated that there will be $23 billion in payouts for incentives from Medicare and $21 billion from Medicaid funds between 2009 and 2019.2 Medicaid Providers Under the HITECH Act, physicians will have a choice of receiving incentive funding through either Medicare Part B or Medicaid, but not both. Medicaid EMR incentives, which will a The latest definitions for meaningful use and certified can be found at: http://healthit.hhs.gov/portal/server.pt?open=512&objID=1325& parentname=CommunityPage&parentid=15&mode=2&in_hi_userid=11113&cached=true. Samuel S. Spicer, MD, is the president of the North Carolina Healthcare Information and Communications Alliance. He can be reached at sam.spicer (at) nhrmc.org. 354 NC Med J July/August 2009, Volume 70, Number 4 Table 1. Medicare Part B Maximum Yearly Payments Potential Medicare Payment Amount, by Year Year of Adoption 2011 2011 2012 2013 2014 2015 2016 Total $18,000 $12,000 $8,000 $4,000 $2,000 $0 $44,000 $18,000 $12,000 $8,000 $4,000 $2,000 $44,000 $15,000 $12,000 $8,000 $4,000 $39,000 $12,000 $8,000 $4,000 $24,000 1% reduction 1% reduction Variable 2% reduction Variable 2012 2013 2014 2015 2016 Table notes: There is a 10% additional payment each year for health services shortage areas. Maximum amount possible is 75% of allowed charges each year. 1% and 2% reduction refers to a reduction in Medicare fee schedule. be administered by the state, will provide payments to a range of practitioners for their meaningful use of EHRs (see Table 2). These incentives can be directed to safety net providers such as federally qualified health centers and rural health clinics, as well as practitioners including nurse practitioners, certified nurse midwives, and dentists. To qualify, providers need at least 30% of their practice to consist of medically underserved patients. Pediatricians need only 20% and will receive two-thirds of the same payment. During the first year, physicians may receive funding to be applied to EMR purchase, installation, and training. Payment is for reimbursement of expenditures, and there are no penalties such as those included in the Medicare program. Economic Impact in North Carolina The North Carolina Medical Board lists over 16,000 licensed physicians practicing in North Carolina. If 50% of these qualify for HITECH funds, it could contribute over $352 million to the state’s economy. However, there is a large gap in the number of EMRs that might qualify for incentive payments. In 2008 it was estimated that nationally 38% of physicians have a basic EMR system of some kind and 4% have a complete EMR system with features such as office notes, order entry, and decision support.3 If the definitions of certified and meaningful use incorporate very basic installations, then nearly 2,000 physicians would need to install and use a new qualifying EMR by the end of calendar year 2010 to qualify for the incentive. A more strict definition could lead to 7,000 physicians needing to upgrade their systems. It usually takes six months or more to plan, purchase, and successfully install an office EMR. Privacy and Security Provisions Privacy and security issues have had major revisions. A collaboration among 44 states and territories, including North Carolina, have developed tools for compliance including a Provider Education Toolkit that provides education regarding privacy and security for physicians in an electronic world. Both the North Carolina Medical Society and the North Carolina Academy of Family Physicians have referenced free CME at the Secure4Health website (http://www.secure4health.org). Table 2. HITECH Act: Medicaid Physician Reimbursement Plan Potential Medicaid Payment Amount, by Year 2011 2012 2013 2014 2015 Year of Adoption 2011 $25,000 $10,000 $10,000 $10,000 $10,000 2012 $0 2013 $0 $0 2014 $0 $0 $0 2015 $0 $0 $0 $0 2016 $0 $0 $0 $0 $0 2017 $0 $0 $0 $0 $0 2016 2017 2018 2019 2020 Total $0 $0 $0 $0 $0 $65,000 $0 $0 $0 $0 $65,000 $0 $0 $0 $65,000 $0 $0 $65,000 $0 $65,000 $25,000 $10,000 $10,000 $10,000 $10,000 $25,000 $10,000 $10,000 $10,000 $10,000 $25,000 $10,000 $10,000 $10,000 $10,000 $25,000 $10,000 $10,000 $10,000 $10,000 $25,000 $10,000 $10,000 $10,000 $10,000 $65,000 $0 $0 $0 $0 $0 NC Med J July/August 2009, Volume 70, Number 4 $0 355 Medical education credits may be available and are part of the offering. Health Information Exchange: The Weak Link Currently there are approximately 193 HIEs with only 57 actively transferring data in the United States.4 The western North Carolina exchange, called Data-Link, began transferring records in 2006 as a collaboration among 16 western North Carolina hospitals. It is now enrolling physician offices.5 University Health Systems of Eastern Carolina, Duke University Health System, and the University of North Carolina Health Care System are all in various stages of exchange within their own integrated delivery networks. For the vast majority of health care in North Carolina the exchange of information is limited to the use of a fax machine, patients physically carrying medical records, a CD, or hand delivery of paper. The financial value of an EMR has been proven to be somewhat successful because of its ability to assist with coding and billing efforts. Quality reporting is emerging as financially rewarding to health care practitioners with programs like Bridges to Excellence, various health plans’ centers of excellence, and the CMS Physician Quality Reporting Initiative rewarding practices for reporting quality measures and/or achieving certain quality benchmarks. Health information exchanges, however, are struggling to find a financial model. Nationally, 82% of exchanges cite the sustainable business model as a difficult challenge to implement.6 To be successful, an HIE must have the support of the collaborators who can harvest the efficiencies such as major health plans (e.g., Medicaid, Medicare, Blue Cross and Blue Shield, military health system, and the Veterans Health Administration), lab companies, and radiology practices. In addition, HIE face difficulty with access to capital, funding misalignment, lack of uniform policies, and data sharing agreements. Recognizing these difficulties has prompted North Carolina to develop a strategic plan for HIT. North Carolina Health Information Technology Strategic Planning Task Force To ensure that North Carolina is in a position to capture as much of the stimulus funding as possible, in April 2009 Governor Beverly Perdue appointed a North Carolina HIT Strategic Planning Task Force. Members represent consumer organizations, public health agencies, physicians, hospitals, mental health providers, and other health care representatives. The Task Force’s report was released June 24, 2009 with recommendations on a strategic approach for EMR, HIE, quality reporting, and health care broadband access.b On July 17th Governor Perdue charged the North Carolina Health and Wellness Trust Fund with leading North Carolina health b 356 IT efforts. A Health IT Collaborative will operate under the direction of the Trust Fund to obtain stimulus grant funds for EMR adoption, HIE operations, quality reporting, and broadband access. HITECH grant funding on a state level can be for planning or implementation efforts. Given the significant amount of groundwork that has been done by the North Carolina Healthcare Information and Communications Alliance (NCHICA), North Carolina Area Health Education Centers, the North Carolina Healthcare Quality Alliance, and other groups, North Carolina should be able to compete for implementation grants this fall as soon as criteria have been finalized by the ONC. Difficult Issues in HIT Implementation Several related issues will have a significant impact on the ability to implement the North Carolina HIT Strategic Plan Task Force report: 1) Role of personal health records and the patient-physician relationship. Patient participation and compliance can be the difference between illness and wellness. Shared decision-making and patient self-management of chronic conditions are key parts of improving health. Personal health records can add safety and reliability to providers’ medical record systems. Mutual trust is the foundation of a healthy physician-patient relationship. Physicians and consumers need to be engaged in how personal health records are incorporated into their EMR. 2) Design of EMR to assist physician workflow. Payment reform is an opportunity to reorient care and subsequently EMR design around electronic abstraction of quality metrics.7 Incentives must be properly aligned so that the EMRs are used to improve quality of care and patient health, not simply used to improve coding. If we are to reward quality, providers need tools that make it easy to deliver the best possible care with quality built into the system. 3) Improving our efficiency. Cost savings are dependent upon decreasing unnecessary testing, appropriate use of guidelines, coordination of care, better preventive care, and workflow efficiencies. Community Care of North Carolina (CCNC) is a proven mechanism for cost savings in the Medicaid population.8 Given current state budget constraints, priority should be given to enhancing CCNC’s medical home functions with health information technology. Electronic prescribing alone provided Mississippi with $1.2 million in cost savings per month in Medicaid prescriptions.9 Because of the efforts of CCNC and BCBS, North Carolina is the 6th highest e-prescribing See http://www.ncrecovery.gov for more details. NC Med J July/August 2009, Volume 70, Number 4 state with currently 15% of prescriptions transmitted electronically. Accurate measurement of the savings will also be needed to help sustain the underwriting of HIEs. 4) Coordinated statewide effort. As outlined in the HIT Task Force report, North Carolina has immense intellectual capital, strong public health programs, proactive provider organizations, excellent teaching institutions, and organizations such as CCNC, the Area Health Education Centers, The Carolinas Center for Medical Excellence, MCNC, eNC, the North Carolina Institute of Medicine, and NCHICA. All of these groups need to work in concert through the North Carolina HIT Collaborative in order to be successful in grant funding and underwriting endeavors. The continued leadership of Governor Perdue and the North Carolina General Assembly can oversee the coordination of efforts among stakeholders and ensure the success of North Carolina’s efforts. 5) In the office assistance. Even with the incentives for adoption, most EMR implementations are time and resource intensive endeavors that still lose money. Using the New York model of exchange development10 to assist providers by having on the ground and in the office expertise will dramatically increase the probability of success. North Carolina should use the existing organizations such as AHEC, CCME, and NCHICA to put resources on the ground and tip the balance in favor of adoption. The HITECH Act brings significant interest in the adoption of electronic medical records, the establishment of health information exchanges, and the enhancement of quality reporting. Providers may be eligible for $44,000 to $65,000 in incentives. Successful application of electronic medical records for meaningful use will depend upon a prompt and effective implementation of new health information exchanges. A coordinated statewide effort has started with Governor Perdue’s appointment of the North Carolina HIT Collaborative. Timely implementation of the HIT strategic plan will allow North Carolina to be competitive for additional grant funding. The result will be better health for North Carolinians. NCMJ REFERENCES 1 Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente electronic health record: transforming and streamlining modalities of care. Health Aff. 2009;28(2):323-333. 2 HHS American Recovery and Reinvestment Act (Recovery Act) implementation plan. Health information technology— Medicare and Medicaid incentives and administrative funding. US Department of Health and Human Services website. http://www.hhs.gov/recovery/reports/plans/hit_ implementation.pdf. Accessed August 19, 2009. 3 Health Information Security and Privacy Collaboration (HISPC). Health Information Technology website. http://healthit.hhs.gov/ portal/server.pt?open=512&objID=1240&parentname=Commu nityPage&parentid=2&mode=2. Accessed June 17, 2009. 4 eHealth Initiative releases results from 2008 survey on health information exchange. eHealth Initiative website. http://www.ehealthinitiative.org/HIESurvey/. Accessed June 17, 2009. 5 HIE lays foundation for longitudinal EMR in western North Carolina. The Healthcare Information and Management Systems Society website. http://www.himss.org/ASP/ ContentRedirector.asp?ContentID=68359. Accessed June 17, 2009. 6 Ambulatory health care data. National Center for Health Statistics website. http://www.cdc.gov/nchs/about/ major/ahcd/ahcd1.htm. Accessed June 17, 2009. 7 National progress report on E-prescribing. Surescripts website. http://www.surescripts.com/e-prescribing-statistics.html. Accessed June 17, 2009. 8 Mercer Consulting. CCNC/ACCESS cost savings—state fiscal Year 2007 analysis. Community Care of North Carolina website. http://www.communitycarenc.com/PDFDocs/ Mercer%20SFY07.pdf. Published February 26, 2009. Accessed August 4, 2009. 9 Preliminary estimates of electronic medical record use by office-based physicians: United States, 2008. National Center for Health Statistics website. http://www.cdc.gov/nchs/ products/pubs/pubd/hestats/physicians08/physicians08.pdf. Accessed June 17, 2009. 10 NYeC submits comments on health IT regional extension center. New York eHealth Collaborative website. http://www.nyehealth.org/node/109. Accessed June 17, 2009. NC Med J July/August 2009, Volume 70, Number 4 357