Emory University Signature Theme Deliverable PREDICTIVE
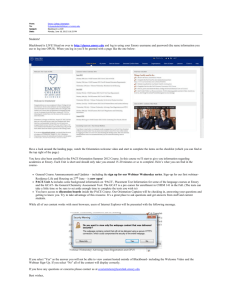
advertisement

Emory University Signature Theme Deliverable PREDICTIVE HEALTH AND SOCIETY Kenneth Brigham, M.D. and Michelle Lampl, Ph.D., M.D. Predictive Health and Society I. Statement of The Theme “Predictive Health and Society” will bring together a universe of disciplines, technologies and management skills to develop an integrated definition of health, the tools to measure it, new interventions to maintain or restore health and an Emory model care system that is health focused, science based and exportable to large populations. This theme will assimilate the University’s and the Region’s unique resources, integrating research, education and health care into a dynamic program that sustains continual discovery and translation of new knowledge into healthier individuals and a healthier society in the US and globally. Introduction America's health care system is second only to Japan ... Canada, Sweden, Great Britain ... well, all of Europe. But you can thank your lucky stars we don't live in Paraguay! - Homer Simpson America spends more on health than other countries, but the results are disappointing; we are not healthier and we are not a model for other world societies. The US spends upwards of sixteen percent of its gross domestic product on health; Japan spends about half that and health expenditures in Switzerland, Germany, France, Canada, Sweden, Australia, Netherlands, Denmark, Italy and Great Britain are all less than twelve percent of GDP. The rate at which health expenditures are increasing is also greater in the US than elsewhere---2.7% between 1990-2002 versus, for example, 1.7% in Great Britain and 0.3% in Denmark. But, we are at serious risk of losing our health while paying dearly for it. If you are a woman born in the United States you can expect to live about five years less that if you were born in Japan and several years less than if you were born in France, Italy, Australia, Sweden, Germany or Great Britain; men can expect about the same. At least by that important metric we are a less healthy people than most of the developed world and we are falling further behind. Between 1960 and 2001 expected life spans increased on average 9.2 years in those other countries and only 7.2 years in the US. The Figure 1: Interdependence of Individual and realization is dawning on thoughtful leaders that Group Health the health care system in the US is not working, not sustainable and nearing crisis. Health matters because it is inextricable from individual happiness, productivity and quality of life, but also because human beings do not Healthy thrive in units of one---individual health and Healthy People Societies societal health depend on each other (figure 1). Our health impacts our social equanimity, our competitiveness and our influence for good throughout the world. It is difficult to imagine an area with a potential to impact the human condition and civilization equal to that of enhancing individual and societal health. What are the possibilities? For the most part, we have defined health passively (being healthy is not being sick) and we have built a health care and biomedical research system that is focused on disease. That system 2 threatens to implode because remedial medicine costs too much, is too inefficient and often fails. The focus on specific diseases may have been inescapable when medicine was largely empiric, the scientific (and social) armamentarium was limited and expectations were low, but all that has changed. Rapidly expanding knowledge is continually unearthing new evidence upon which to base health care. Science, technology and sophisticated social inquiry promise opportunities for understanding ourselves and our fellows with a completeness that we have yet to comprehend Emory University can lead discovery and implementation of a new approach that will change concepts of health and health care--shift the paradigm---to the enormous benefit of people and credit to the university. We are uniquely positioned with cross-disciplinary capabilities to address this issue. We can do well by doing good. Proactive versus reactive Figure 2 illustrates the current paradigm and how it can shift to advantage health. Contemporary medicine is a disease care system, not a health care system. Applying resources to defining health, developing tools to measure it and interventions that, done early, maintain or restore health, and developing a workable implementation strategy, can produce an Figure 2: The Health/Disease Continuum efficient, cost effective, accessible system. But, that is a big task, maybe an unprecedented one. It must involve basic and applied investigators from a broad range of disciplines, from hard science to humanities, including not only geneticists, D H nanotechnologists and the like, but also I E S economic theorists, business experts, A E L epidemiologists, chemists, ethicists, social A T S scientists, health behaviorists, experts in law, H E ethics, health policy, systems biologists, and others. And this array of experts must function with a common focus and a commitment to elaborate communication; research in each area must inform all others. The research should be serious inquiry driven by the problem to be solved, sitting squarely in what Donald Stokes called “Pasteur’s Quadrant,” pursuing understanding and use together. A theory and how it could be explored is diagrammed in figure 3. There is accumulating evidence that a limited number of generic processes are harbingers of many apparently different pathologies of both soma and psyche. If those Figure 3: Predictive Health and Society processes could be easily accessed and monitored, they would define health with new depth and mark early deviations from health at a time when interventions are more likely to work. The power of this concept is that measuring generic biomarkers that predict a host of diseases makes the task of developing the analytic tools critical to predicting health less daunting than the “one marker one disease” concept. Three examples. 1) A study conducted in the Departments of Medicine and Psychiatry at Emory, found that markers of oxidant stress that can be measured in a blood sample correlate with early markers of atherosclerosis Normal Low risk Normal High risk Pre disease Early disease Late disease Predictive Health Contemporary Medicine Determinants of Health Environment Genomics/ Metabolomics/ Proteomics Genetics Population Biology Behavior Molecular Imaging Systems Biology Generic Pathways Bioinformatics Some Enabling Technologies Nanomedicine Quantitative Medicine Ethics Immunology and Inflammation Development Oxidative and Stress Senescence Public Policy Business, Finance and Economics Other Generic Regeneration and Repair Pathways Novel Therapeutics Education Specific Diseases Cardiovascular Diseases Chronic Lung Diseases Cancer Diabetes Neurological Diseases 3 Other Diseases Some Enabling Disciplines and kidney disease, but also with early signs of depression. 2) A recent study reported in the Proceedings of the National Academy of Sciences found that the social stress of caring for a loved one with a severe chronic disease caused molecular changes in blood cells that are associated with senescence (decreased telomerase activity and telomere shortening). 3) Corey Keyes in the Department of Sociology at Emory used a measure of mental health that included measures of depression and of subjective well-being and found a clear relationship between this determination of mental health as a “complete state” and cardiovascular disease. Understanding health and determining how to keep it will require all kinds of expertise. The surface has been barely scratched. Changing concepts of health and disease and of health care will both require and dictate changes in how we educate health care professionals. This approach will also create entirely new opportunities for education and research in the array of disciplines involved in the effort. The integrated, “Pasteur’s Quadrant,” concept of research that is problem focused and inquiry driven will be a fecund setting for innovations in learning and in enabling the process of discovery. Definition of the topic Predictive Health and Society should be broadly multidisciplinary, but problem focused. The effort will include investigators and thinkers from the array of disciplines mentioned above, bonded together by their conviction that individual and societal health presents great needs and challenges, but even greater opportunity---maybe the greatest opportunity to have a positive impact on humanity that will present itself to a community of scholars in our lifetime. These scholars will be committed to interdisciplinarity to an uncommon degree. They will reach well beyond their specialty, learn the multiple languages of other disciplines and commit to listening, learning and teaching as interactive processes that inform the overall effort. Health as a theme can unify University Schools, Programs and Departments, providing a major force for moving the University from a vertical model of parallel but separate endeavors to a network of investigations with a focus that is a central social value with global reach. As disparate societies become more interconnected, we share health concerns---modernization, environmental changes, homogenization of lifestyles are not always healthier. Scientific innovations from better drug development based on genetic knowledge of infectious organisms to targeted intervention in individual lifetimes are imminent. A University-based endeavor brings the science of health together with the ethics of well being and health decision-making and creates a forum for exploring societal concerns. The universe of disciplines essential to addressing these common human challenges exists only in Universities and Emory is especially well positioned. Pre-emptive health care, vis-a-vis our present medical system, has profound economic implications. For example, Figure 4 (see page 5) is a hypothetical comparison of how a disease based system (contemporary medicine) and a health based system (the Emory model) might serve a person born with a predisposition to develop coronary artery disease. Focusing on detailed health related information and early intervention will decrease demand for expensive care of failing organs and prolong high quality life. As technologies mature, the cost of obtaining, storing and interpreting health relevant information will be such that this approach will be economically feasible. These challenges demand the best minds of our Business School working in concert with other essential disciplines. This theme can launch from a population-based initiative that will accumulate a database of healthy people to be followed prospectively. This will not be a clinic for contemporary care, but rather a test site for the new biomedicine. This population will be used to develop an integrated definition of health and to determine how well candidate markers predict health, identify risk and detect premorbidity. Strategies for effectively implementing predictive health care including economic models will also be field tested in this population as will innovative interventions aimed at maintaining health, minimizing risk and restoring health prior to overt disease. This component of the theme will be an extraordinary opportunity to integrate clinical care with research and education in the many disciplines that can influence both the process and the outcome. 4 0 10 20 30 2 5 y r , n a n o s c r e e n , e le v a t e d o x s t r e s s d e t e c t e d , r e v is e d d ie t , e x e r c is e a n d t h e r a p e u t ic 40 6 2 y r s , f a t a l M I w it h 5 d a y s in I C U 5 3 y r s , f o llo w - u p P C T A 50 60 70 30 80 direct cost indirect cost $42,720 $37,920 (lost productivity) direct cost indirect cost $15,000 $12,000 (lost productivity) direct cost indirect cost $65,000 $500,000 (lost economic value x 20 yrs) Total $672,640 I n c r e a s e d lif e s p a n N e o n a t a l g e n o m ic r is k a s s e s s m e n t Emory model, risk evaluation and early intervention 20 1 8 y r , m e t a b o lo m e s c r e e n c h a n g e , p r e s c r ib e d d ie t 10 B e g i n a n n u a l p h y s e x a m s w it h m e t a b o lo m e , p s y c h o - s o c ia l e v a lu a t io n , d e p r e s s io n s c o r e a n d c o g n it iv e f u n c t io n 0 3 2 y r , c h a n g e in m e t a b o lo m e a n d n a n o s c r e e n , u p d a t e m e d ic a t io n s Conventional medicine 4 7 y r , a c u te M I 2 2 y r , s ile n t a t h e r o g e n ic changes Figure 4: Hypothetical comparison of a disease focused health care model (Conventional medicine) with a health focused system (the Emory model) for a person born with a predisposition to coronary artery disease 40 50 60 70 80 Neonatal risk assessment: direct cost indirect cost Annual physical exam direct cost indirect cost Nanoscreen added direct cost indirect cost $9,300 ($150/yr x 62 yrs) $0 (combined with annual physical Add therapeutic direct cost indirect cost $2,555 (7 yrs of drug at $1/day) $0 Revise therapeutic direct cost indirect cost $18,250 (50 yrs of drug at $1/day) $0 Total $45,605 5 $500 $0 $10,500 ($150/yr X 70 yrs) $4,500 (time off work, .25 day/60yr) II. Differentiation and Transformation What others are doing A number of academic, private and industrial institutions have initiated programs that address one or another part of the health care challenges and opportunities presented by developing science and technology. However, these tend to be either focused exclusively on developing technology, application of traditional preventive medicine programs or on commercial interests. Some examples of programs being conducted in academic settings include the following: Institute for Systems Biology This independent organization in Seattle, Washington, structured as a not-for-profit, is fully engaged in systems biology research. Not affiliated with an academic institution, but wearing some of the characteristics of academia, the institute is a purposely small, focused, interdisciplinary group of scientists. Scientific areas of expertise include biology, physics, chemistry, computing, mathematics, medicine, immunology, biochemistry and genetics, making this a technologically broad interdisciplinary group. The work is narrowly focused on developing new technologies in genomics and proteomics. The founder of this institute, Leroy Hood has written extensively about what he calls prospective, predictive, personalized medicine. The concept is not unlike what we propose, but the institute lacks both interest and expertise for translating the technology to society. Duke University The Duke healthcare model is heavily influenced by the Snyderman emphasis on prospective health care. Duke is utilizing its employee population to build a prospective medicine model utilizing personal health “coaches” to assist patients in successfully implementing their personalized health plan. There is a formal collaboration between Duke University and the Center for the Advancement of Genomics intended to create the first fully integrated practice of genomic medicine. The Institute for Genome Sciences and Policy is the Duke response to the needs of genomic medicine, and will play a key role in addressing the scientific and ethical issues surrounding this new practice of medicine. This model is heavily weighted toward traditional preventive medicine at the clinical end and genomics at the other. Broad Institute Founded in 2003, this is a joint effort between MIT, Harvard University and the Whitehead Institute. With origins in The Center for Genome Research, this center served as the flagship of the Human Genome Project, the international effort to identify the blueprint for a human being. Founded in 1990, the Center grew to become one of the largest genome centers in the world and an international leader in the field of genomics, the study of all of the genes in an organism and how they function together in health and disease. Today, the Center houses a broad range of thriving research programs combining structural genomics, medical and population genetics, and clinical medicine. The Center's annual budget is $80 million, and it employs 250 people, including scientists and medical researchers from Whitehead, MIT, and Harvard. Like many of these programs, this effort is heavily focused on genomics/genetics. Washington University The BioMed 21 initiative, designed to reorganize and reorient the biological sciences at Wash U., is intended to reshape University culture over the next 10 years. The stated goal of the initiative is to rapidly convert the knowledge of the genetic blueprint of human beings into effective, individualized treatments. This is a conventional initiative, taking place fully within the academic and financial structure of the University. It occupies four physical locations: a reconstructed area adjacent to the Genome Sequencing Center, a new 250,000 sq/ft building in the medical campus for translational research, the Farrell Learning and Teaching Center, and a 40,000 sq/ft facility designed to facilitate development of mouse models for human diseases. This is a program with the goal of 6 implementing genomics into clinical medicine with a focus on treatments aimed at established diseases. Johns Hopkins The McKusick-Nathans Institute of Genetic Medicine has as its mission to further the understanding of human heredity and genetic medicine, and use that knowledge to treat and prevent disease. To that end, the Institute is working to consolidate all relevant teaching, patient care and research in human and medical genetics at Johns Hopkins and to provide national and international leadership in genetic medicine. It serves as a focal point for interactions between diverse investigators to promote the application of genetic discoveries to human disease and genetics education to the public. It builds upon past strengths and further develops expertise in the areas of genomics, developmental genetics, and complex disease genetics. In addition, it is hoped it will catalyze the spread of human genetic perspectives to other related disciplines by collaboration with other departments within Hopkins. This organization, located within Johns Hopkins, conducts basic and translational genetic research. Their program emphasis does not extend to work beyond genetics, and does not directly tie to other Johns Hopkins departments and centers. While collaboration with other disciplines is a stated goal, it is not a hard-wired component of their structure. They have launched a national “Johns Hopkins---Imagine” advertising campaign that appears to be based on the concept of this institute. What unique resources does Emory have and how can Emory lead? Several concepts underlying a Predictive Health and Society theme at Emory differentiate this effort from others. In addition, Emory and the Atlanta area have characteristics uniquely suited to pursuing this theme. For example: • A focus on health We propose to focus this effort on health, not disease. That approach contrasts with many, possibly all, of the efforts in this area at other institutions. Even predictive models are mostly focused on identifying predictors of diseases rather than characterizing health. Emory has preeminent researchers who can re-conceptualize medicine as the definition and preservation of health. • Generic processes as definers of health Other programs in predictive/prospective/personalized medicine are aimed at identifying detectable markers of risk or pre-disease states that are specific for a given disease (e.g. cancer, heart disease, diabetes). Our hypothesis is that there are generic processes that characterize health, deviations from which indicate loss of health but are not disease specific. The power of this concept is the implication that there are generic biomarkers that might predict a host of diseases so that the task of developing the analytic tools critical to predicting health is less daunting than the “one marker one disease” concept. • A special environment Emory University, The Woodruff Health Sciences Center, Georgia Tech, the CDC, the Carter Center, the American Cancer Society and the population served by Emory HealthCare together compose an environment rich in intellectual, scientific, technological and human resources that is uniquely suited to developing and implementing a new approach to health care that will illustrate the power of integrating diverse assets to focus on a critical social issue. The “Emory Model” should become the benchmark for the new biomedicine. • Unique combination of technologies The technological expertise at Emory and Georgia Tech are cutting edge in several areas, including nanobiology, imaging, genomics/metabolomics. There already exist many collaborative efforts in these areas that are both innovative and productive. The opportunity and resources to bring these technologies together with a predictive health focus and integrated with the broader scope of expertise that we propose is unique to this environment. 7 • Integration of science, technology, ethics, humanities, law, business, health policy, economics Management challenges presented by this endeavor encompass fundamental leadership, communication, motivational and collaborative processes; ethical, legal and political issues are equally challenging. The focus not only brings science and technology together, but engages the numerous other areas of expertise that will be essential to implementing a new approach to health care and will make Emory one of a kind in the area and propel us to the forefront of efforts to change the system. With the College, the School of Public Health, the Schools of Law and Business and health systems programs at Georgia Tech, we have available a special collection of relevant resources. The theme centers a major cultural value—health---at the nexus of collaborative research among basic scientists, social scientists, and religious and legal scholars. • Systems science---cells to societies The developing Systems Biology program at Georgia Tech brings a basic approach to integrating biologic processes at a cellular level that will make major contributions to predictive health. Designing social models that will function to implement a new health care system involves a similar rigor in defining interacting networks and modeling responses to perturbations. This theme could create new synergy by bringing together experts in both areas with a common focus. • Building bridges between population health and individual health Traditionally, population based health initiatives and individual based approaches have been separate activities. A predictive model of health care should impact both approaches and development of the model should integrate information and issues across the spectrum from individuals to populations. With the School of Public Health and the CDC we have extensive involvement and expertise in population health and the opportunity to bring that perspective together with the science, technology and individual focus is special. Emory can move quickly to the vanguard of a new biomedicine by bringing together these unique concepts and resources to focus on development and design of a workable system of care that is aimed at defining and maintaining health. By integrating the range of disciplines essential to new discoveries that span the spectrum from basic science through translational research to design and proof of principle of a delivery system that is ethical, effective, economically viable and achievable in this country and elsewhere, Emory can declare itself a destination university for health related matters. What could it look like in ten years? Emory can be a global center of societal health research, modeling the importance of integrating bench innovations in technology into everyday health in a diversity of environments based on an integrated approach that respects cultural diversity in beliefs, values and goals. Emory can be a national example of the success of pre-emptive health care. Emory can become the University that contributes to society at a time when the distance between achievements of the academy in general, and science in particular, were distant from the general public. Emory can be the meeting place for challenging discussions on the human condition. A nidus of activity will exist around this theme involving international groups holding regular symposia that are not unique to any discipline, because this will have become the standard for cutting edge research. Programmatic research will include transdisciplinary seminars and regular publications of scholarly treatises addressing different aspects of the challenge of health care. Formal activities focused on predictive health and society will be central to the curriculum, involving faculty from Emory college and professional schools, Georgia Tech, the CDC and other local institutions, identifying Emory as a serious participant in design of the new biomedicine. These would be a draw for all of the Schools and would provide a destination for international collaboration. 8 A substantial investment to create a new physical space would permit the academic home for investigators from each of the key disciplines and provide resources for recruiting a few (5-10) faculty who would complement current Emory and Georgia Tech faculty committed to this endeavor would enable a quantum advance toward international preeminence in the area. Ten years hence, Emory could be the leader in establishing a new biomedicine that would redefine biomedical research and clinical care, invent new areas of scholarship by ignoring the boundaries of traditional disciplines, provide an educational experience that prepares students to lead the next generation to further advances in individual and societal health and favorably impact the productivity and well-being of the broad community. How can this theme transform Emory University? Emory: A destination university internationally recognized as an inquiry-driven, ethically engaged, and diverse community, whose members work collaboratively for positive transformation in the world through courageous leadership in teaching, research, scholarship, health care, and social action. The Predictive Health and Society theme will relate to every component of Emory’s articulated mission, contributing broadly to the transformation of the university envisioned in that statement: • • • • • • • • A destination university---Emory can become a recognized destination for the new biomedicine, a unique source of creative thought that integrates the several elements essential to a new health system. Internationally recognized---New knowledge and practical experience with health care innovation will have global implications and will identify Emory as a world leader in this area. Inquiry-driven---The entire effort will be driven by a passion for new knowledge and how it can be used to impact individual and societal health. Ethically engaged---Kathy Kinlaw says that “predictive health is fundamentally an ethical concept”. Acquisition of new categories of information about people and how that information is used, design of a delivery system that is fair and accessible, how societal resources are allocated, etc., are ethical issues that must be addressed as an integral part of the process of transforming health care. A diverse community---Scholars involved in this effort will be drawn from across the university and from other institutions in the area. The effort must address disparities in health and research under this theme will result in definitions of health related diversity that transcend traditionally defined ethnicities. Working collaboratively---The nature of the theme dictates that a broad range of disciplines must focus on the problem and dynamic interactions among a diverse group of scholars is the core of this effort. Positive transformation in the world---It is difficult to imagine an effort with as great a potential to impact every aspect of society as the development of an efficient, equitable, accessible, practicable, economically feasible system of care that preserves individual and societal health. Courageous leadership in teaching, research, scholarship, health care and social action--This is a bold theme with a grandly ambitious goal that integrates research, scholarship and education in an innovative effort aimed directly at revolutionizing care of our citizens to preserve and prolong the health of individuals and of society. 9 Realizing the potential of this theme will require both an institutional commitment and enthusiastic participation of scholars from virtually every corner of the university. Creation of a physical facility that enables multidisciplinary activities and resources for recruiting key faculty will be necessary tangible commitments. An ultimate measure of success of this effort would be an Emory model of health focused care that is widely adopted as the benchmark of the new biomedicine. The model should be universally accessible, affordable and produce healthier individuals and a healthier society. More immediate measures of success include a university wide enthusiasm for and commitment to the theme, successful attraction of dedicated resources from philanthropic sources, scholarly publications in the many areas relevant to this effort, a change in focus of education of health professionals and students in other areas to align educational experience with changing career expectations, a distinct Emory influence on public policy related to health and extensive extramural support for the unique research programs. The ability to attract high quality faculty and students into the program and to entrain them in career paths in this area would be an important measure of educational success. An innovative organizational structure that enables dynamic interactions among disparate disciplines that share focus on a goal could be an academic model that would apply to interdisciplinary research and education in general. III. Unanswered Questions Several questions that can be anticipated are as yet unanswered and no doubt additional questions will arise as the effort progresses. Some anticipated questions are: • How will we overcome the inertia of an entrenched system with a long list of vested interests? • How can the effort be structured to realize the potential synergy of interacting disciplines? • How will the health care system in academic settings and elsewhere, be transitioned from a disease focus to the Emory model while maintaining viability and continuing to deliver the best available service? • Will the change in health care occur by evolution or revolution (i.e. will the current system implode, forcing dramatic change)? • How will society in general respond to such a radical change? • Is what we propose best communicated by the term “predictive health” or is there something better? • How can the concept be articulated in a way that captures the imagination of academics and people in general? • How much will it cost and how will it be financed? IV. Next Steps to Move Forward Review of this theme as a candidate for a signature theme for Emory University will take place soon and that decision will affect the appropriate next steps. In the meantime, we should proceed with the planning activity already underway that is a collaborative effort of the Woodruff Health Sciences Center and Georgia Tech. The university decision will affect the scope and nature of the planning process as well as the people involved. 10 References Epel,ES, Blackburn,EH, Lin,J, Dhabhar,FS, Adler,NE, Morrow,JD, Cawthon,RM. Accelerated telomere shortening in response to life stress. Pro Natl Acad Sci USA 101:17312-17315, 2004. Harrison, D, et al. The markers of oxidant stress (MOST) study. In process of publication Keyes, CLM. The nexus of cardiovascular disease and depression revisited: the complete mental health perspective and the moderating role of age and gender. Aging & Mental Health 8:266-274, 2004 Stokes, DE. Pasteur’s Quadrant: Basic Science and Technological Innovation. Brookings Institution Press, Washington, DC, 1997. The health of nations. The Economist July 17, 2004, pp 3-19. 11