Care of the Patient with Respiratory Needs Study Module
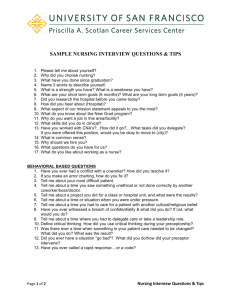
advertisement

Title: Regional Hospital: Care of the Patient with Respiratory Needs Study Module for the Certified Nursing Assistant Purpose: A. B. C. Provide quality of care to the respiratory patient To ensure the Certified Nursing Assistant recognizes respiratory distress The Certified Nursing Assistant identifies measures and devices to use and promote oxygenation Competency: To provide essential patient care to the patient with compromised respiratory function Objectives: Upon completion of this study module the Certified Nursing Assistant will be able to: A. Recognize normal respiratory function B. Define normal respirations that need reporting to the nurse C. Recognize signs and symptoms of hypoxia and altered respiratory function D. Identify common disorders that lead to deficiency of oxygen, dyspnea, and difficulty completing ADL’s. E. Identify factors that alter oxygen needs F. Monitoring with pulse oximetry G. Describe types and devices for oxygen delivery H. Identify guidelines for safe oxygen therapy I. Identify ways to promote oxygenation Content: A. B. C. D. E. F. G. H. Respiratory function and definitions of abnormal respirations Hypoxia; Signs and symptoms of hypoxia and altered respiratory functions Common Disorders Factors affecting oxygen needs; pulse oximetry Oxygen delivery systems/devices Safe oxygen therapy Oxygenation promotion References Required Activities: A. Read and study the module B. Read the text Mosby’s using pulse oximetry (pg. 638 & 639) and setting up for oxygen administration (pg. 649) C. Provide care to patients with respiratory distress D. Complete post-test with 85% accuracy Approved By: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction: The respiratory and cardiovascular systems must function properly for cells to get enough oxygen. Oxygen is needed for survival. The respiratory system brings oxygen into the lungs and eliminates carbon dioxide. Any disease, injury, or surgery affects the body’s ability to take in oxygen and deliver it to the cells. Serious illnesses occur with oxygen deficit. Additional oxygen may need to be given to meet the body’s needs. Safe and effective care must be provided to patient with respiratory compromise and oxygen needs. Overview: Respiratory system function involves three processes: A. Air moving into and out of lungs B. Oxygen and carbon dioxide exchanged at alveoli C. Blood transports o2 to the cells and removes Co2 from them. Respiratory function is altered if any of these three processes are affected 1. The process of supplying the cells with oxygen and removing carbon dioxide from them is called respiration 2. Respiration involves inhalation (breathing in) and exhalation (breathing out) 3. Normal adult respirations are smooth, regular, and unlabored with a rate of 18-20 per minute. Both sides of chest rise and fall equally. 4. Infants and children have higher respiratory rates. 5. Count respirations by watching the rise and fall of the chest Content: A. Symptoms of respiratory distress 1. 2. 3. 4. 5. Fast breathing-Rate increase, over 24 per minute Slow breathing-Rate less than 16 Labored breathing-Short of breath/gasping Apnea-Absence of breathing Irregular-Patient is irregular B. Hypoxia-deficiency of oxygen in the cells Signs and symptoms of hypoxia 11. Restlessness 12. Dizziness 13. Disorientation 14. Confusion 15. Behavior/personality changes 16. Difficulty concentrating and following directions 17. Apprehension/anxiety 18. Fatigue 19. Agitation 20. Increased pulse rate 21. Increased rate/depth of respiration 22. Sitting position-often lean forward 23. Cyanosis-blue color to skin, lips, mucous membrane and nail bed 24. Dyspnea 25. Air hunger 26. Licking lips Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ C. Common Disorders that lead to oxygen deficits 1. Severe COPD 2. Asthma 3. Pneumonia 4. Bronchitis 5. Croup 6. RSV 7. CHF D. Factors affecting oxygen needs 1. Respiratory system status 2. Cardiovascular system function 3. Blood counts 4. Intact nervous system 5. Aging 6. Exercises 7. Fever 8. Pain 9. Medications 10. Smoking 11. Allergies 12. Pollutant exposure 13. Nutrition 14. Substance abuse E. Devices for oxygen delivery- for those who need oxygen therapy 1. Nasal cannula Two prongs that project from the tubing that are inserted a short distance into nostrils. Prongs point upward. Tubing is brought behind the ears to keep the cannula in place. Simple to use, but limited to lower percent oxygen delivery 2. Simple facemask Covers nose and mouth, has small holes in the side of the mask for carbon dioxide to escape during exhalation. Room air enters with inspiration. This mask is able to deliver a high percent oxygen and humidity. This mask can be uncomfortable because it is hot and irritating to skin. It can cause claustrophobia, and prevents normal talking and eating. 3. Partial rebreather mask A reservoir bag is added to the simple mask. The reservoir bag is for exhaled air. The bag should not totally deflate with inhalation. 4. Non-rebreather face mask Prevents exhaled air from entering reservoir bag. Bag must not totally collapse during exhalation. 5. Venturi mask Delivers exact oxygen percentage with high humidity. There is less mucous membrane irritation 6. Oxygen tent Delivers high humidity, but is claustrophobic 7. Oxygen Flow rate is usually 2-15 liters/minute. Desired rate is ordered by provider and applied by nursing staff. Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ F. Safe Oxygen Therapy- Oxygen is necessary for life 1. Guidelines for safe Oxygen use: a. Observe no smoking signs b. Know location of fire extinguishers c. Never use oxygen near electrical equipment, (shaver) d. Monitor proper flow rate e. Check o2 tank level when using portable tank 2. Comfort measures for Oxygen therapy use: a. Check ear, nose, mouth, or chin area for dryness, discomfort or soreness b. Use humidifier c. Check cannula/mask for proper fit and comfort d. Offer extra liquids to drink e. Provide frequent oral/nasal care f. Provide increased reassurance and support g. Report signs and symptoms of hypoxia, respiratory distress, or abnormal breathing patterns to the nurse G. Measures to promote oxygenation 1. Positioning a. Head of bed 300 b. Frequent position changes are important 2. Coughing and deep breathing a. Promotes air movement 3. Incentive Spirometry a. Device to promote deep breathing 4. Head of bed will usually need to be elevated with someone on oxygen therapy. 5. Oxygen can be very drying and uncomfortable 6. Dry oxygen thickens the respiratory secretions making breathing more difficult 7. Oxygen may be passed through a humidifier (water bottle) to increase moisture 8. Fill humidifier with sterile water, as tap water increases the risk of contracting Legionnaire’s Disease 9. Oxygen saturation of 90% or greater need to be monitored to insure adequate oxygenation. This may be monitored by pulse oximetry-a machine that measures oxygen concentration in arterial blood. A sensor or probe can be attached to the finger, toe, earlobe, nose or forehead. Summary: Oxygen is taken in through the air we breathe. Some conditions/diseases make it difficult to take in enough oxygen. Additional oxygen may be ordered and delivered either intermittently or continuously. Page 4 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Name: ______________________ Score: ______________________ Regional Hospitals: Respiratory Final Exam for the Certified Nursing Assistant 1) Name 2 devices for oxygen delivery 1. _____________________________ 2. _____________________________ 2) List 3 common disorders of the Respiratory System 1. _____________________________ 2. _____________________________ 3. _____________________________ 3) List 4 signs and systems of hypoxia (lower-oxygen) 1. _____________________________ 2. _____________________________ 3. _____________________________ 4. _____________________________ 4) Measures to promote oxygenation A. Positioning B. Coughing/deep breathing C. Incentive Spirometry D. All of the above 5) Flow rate of a nasal cannula is 10-15 liters True or False 6) You may use an electric razor if the oxygen is turned off? True or False /CBO/NURSE ASSIST/HCMH/8/13/2004/ Regional Hospitals: Respiratory Final Exam for the Certified Nursing Assistant 7) List 4 factors that affect oxygen needs 1. _______________________________ 2. _______________________________ 3. _______________________________ 4. _______________________________ 8) When a patient is short of breath, the Certified Nursing Assistant should keep the head of the bed flat True or False 9) Normal respiratory rate is: A. 8-20 B. Over 24 C. Less than 8 D. None of the above 10) Oxygen saturation level of 89 percent or below is normal True or False /CBO/NURSE ASSIST/HCMH/8/13/2004/ Respiratory Final Exam Answer Key 1. Devices for oxygen delivery- for those who need oxygen therapy 1. Nasal cannula Two prongs that project from the tubing that are inserted a short distance into nostrils. Prongs point upward. Tubing is brought behind the ears to keep the cannula in place. Simple to use, but limited to lower percent oxygen delivery. 2. Simple facemask Covers nose and mouth, has small holes in the side of the mask for carbon dioxide to escape during exhalation. Room air enters with inspiration. This mask is able to deliver a high percent oxygen and humidity. This mask can be uncomfortable because it is hot and irritating to skin. It can cause claustrophobia, and prevents normal talking and eating. 3. Partial rebreather mask A reservoir bag is added to the simple mask. The reservoir bag is for exhaled air. The bag should not totally deflate with inhalation. 4. Non-rebreather facemask Prevents exhaled air from entering reservoir bag. Bag must not totally collapse during exhalation. 5. Venturi mask Delivers exact oxygen percentage with high humidity. There is less mucous membrane irritation. 6. Oxygen tent Delivers high humidity, but is claustrophobic. 7. Oxygen Flow rate is usually 2-15 liters/minute. Desired rate is ordered by provider and applied by nursing staff. 2. Common Disorders that lead to oxygen deficits 1. 2. 3. 4. 5. 6. 7. 3. Severe COPD Asthma Pneumonia Bronchitis Croup RSV CHF Hypoxia-deficiency of oxygen in the cells Signs and symptoms of hypoxia 1. Restlessness 2. Dizziness 3. Disorientation 4. Confusion 5. Behavior/personality changes 6. Difficulty concentrating and following directions 7. Apprehension/anxiety 8. Fatigue 9. Agitation 10. Increased pulse rate /CBO/NURSE ASSIST/HCMH/8/13/2004/ 11. 12. 13. 14. 15. 16. Increased rate/depth of respiration Sitting position-often lean forward Cyanosis-blue color to skin, lips, mucous membrane and nail bed Dyspnea Air hunger Licking lips 4. D 5. F 6. T 7. Factors affecting oxygen needs 1. Respiratory system status 2. Cardiovascular system function 3. Blood counts 4. Intact nervous system 5. Aging 6. Exercises 7. Fever 8. Pain 9. Medications 10. Smoking 11. Allergies 12. Pollutant exposure 13. Nutrition 14. Substance abuse 8. F 9. A 10. F /CBO/NURSE ASSIST/HCMH/8/13/2004/ Title: Regional Hospital: Care for the Dying Patient Study Module for the Certified Nursing Assistant Purpose: This module addresses certified nursing assistant’s measures to support the dying patient and the family Competency: Promotes physical comfort and peace in the final phase of life Objectives: Upon completion of the study module the Certified Nursing Assistant will be able to: A. Identify the characteristics of the dying process and interventions for direct care B. Identify what is meant by DO NOT RESUSCITATE C. State guidelines for providing emotional support. Content: A. B. C. D. Dying Process General signs, symptoms and interactions Understanding DNR orders Giving emotional support Summary: Required Activities: A. Read and study The Care for the Dying Patient Study Module B. Complete the final exam with 85% accuracy C. Provide care to a dying patient and their family Approved By: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction: Dying is the final event in life. Death is a precious, private journey that may be measured in time by months to weeks. The priority of care frequently shifts during this time to focus on the dying process with an emphasis on end-of-life decision making and care that supports physical, emotional, spiritual comfort and death that is consistent with the values and wishes expressed by the patient. The certified nursing assistant will focus on comfort care, which helps keep people at their best possible comfort levels when any cure and maintenance of function is impossible and their condition irreversibly approaches the moment of death. Dying ends when all body functions cease. Overview: As certified nursing assistants play an important role in acknowledging the grief responses that patients and family/caregivers may be having. There are three response times in the grief process where patients and families need support. The first time is one of shock and disbelief. The second is developing an awareness of the loss and what it will mean. The third response is reorganization and recovery. Staff will need to identify the stage the patient and family are in and then provide interventions to offer the support needed. Content: The Dying Process During the dying process, the body and its physical and mental functions progressively slow down. This is a natural normal process in which the body prepares for and transitions towards death. Certified nursing assistants should be aware of the common signs and symptoms associated with the dying process in order to increase presence, support, and comfort measures to the patient and family as the patient approaches and is in the dying process. There are certain physical sign and symptoms that may indicate that the patient is approaching the dying process and/or actively dying. General signs and symptoms are as follows: A. Pain When the patient is actively dying, the characteristics of the pain may change and the pain intensity may increase or decrease. 1. Report changes in symptoms to the nurse 2. Provide comfort measures B. Confusion and Disorientation At times, the patient may be confused about the time, place, and identity of people surrounding him/her, including family members and close and familiar people. Intervention Educate family members to speak in a calm, clear manner to the patient. To make communication with confused and disoriented patients more effective certified nursing assistants should identify who they are upon entering room and speak clearly and truthfully when something important needs to be communicated to the patient. Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ C. Decreased or Lack of Swallow Reflex The swallow reflex may diminish or become absent during the imminent stage and aspiration could result due to forcing of fluids and food. The need for food and fluid decreases as patients approach death, and they often want little or no food or fluid. According to current research, terminal dehydration may not be distressing, but actually beneficial to the patient in the terminal stages. Intervention • Offer patient small sips of liquids of choice or ice chips to wet mouth • Frequent oral care • Lip lubrication D. Restlessness and Terminal Agitation Agitation may be due to pain, a full bladder, fecal impaction, respiratory distress, and/or spiritual distress. The patient may make restless and repetitive motions, such as pulling at the bed linen or clothing. Safety measures are instituted. If the patient is close to death and is experiencing terminal agitation, comfort measures should be instituted immediately. Terminal agitation requires sedation. Assure families that restlessness is part of the dying process for most patients and is not due to anything they have done or not done. Intervention • Provide safety measures • Pain: provide comfort measures • Spiritual: call patient’s pastor or chaplain • Family or volunteers to sit with patient E. Fever (>102 degrees) The patient is treated if he/she is experiencing signs and symptoms of discomfort associated with elevated temperature. Under most circumstances, low-grade fevers will not cause discomfort to the patient and need to be treated. Intervention • Report fevers to the nurse • Provide comfort measures F. Decubitus Ulcer/Wounds Not Healing For patients who are dying, some may have decubitus ulcers and wounds that may not heal regardless of the treatment plan. Turning and lotioning the patient every two hours not only prevents complications, but it also provides comfort to the patient by relieving pressure on those sensitive and sometimes painful areas. Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Intervention • Reposition and lotion skin care every 2 hours G. Constipation/Diarrhea Changes in bowel patterns may occur during the dying process. The body slows down its natural functioning, and bowel patterns are often affected by this slowing. Intervention • H. Report complaints to nurse. Provide comfort measures Incontinence The patient may lose control of the bowel and bladder as muscles begin to relax in the Spinchters. Intervention • Report incontinence to the nurse • Change pads and institute skin care measures I. Cold and Mottled Extremities The patient’s hands, arms, feet and legs may be increasingly cool to the touch. At the same time, the color of the skin may change. The underside of the body, or the body parts lying against the bed, may become darkened. Nail beds and lips may take on a bluish appearance, and extremities become mottled (patches of bluish discolorations). This is a normal indication that the circulation of blood is decreasing to the body’s extremities and being used by the most vital organs. Covering the patient with additional blankets may increase agitation. Intervention • Reposition and lotion every 2 hours. J. Respiratory Congestion Respiratory congestion is known as the Adeath rattle@ and/or Arespiratory bubbling@. Patients who are dying may not be able to expectorate their secretions because they are too week and/or comatose. Their breathing becomes noisy and rattling. While the patient may not be uncomfortable, this Arattle@ can be very frightening for the family members. Most patient’s experiencing the Adeath rattle@ are not aware of their surrounding or noisy breathing. Intervention • Reposition patient every 2 hours. • Frequent oral hygiene Page 4 K. Breathing Pattern Changes /CBO/NURSE ASSIST/HCMH/8/13/2004/ The patient’s regular breathing patterns may change as he/she approaches death. A particular pattern consists of shallow, irregular breathing with periods of apnea for 5 to 30 seconds or longer. The patient may also experience periods of rapid, shallow pant-like breathing. Intervention • Elevate the head of the bed • Use circulating fans • Reposition side to side L. Understanding DNR-Do Not Resuscitate Orders When death is imminent some patients may choose to be on “DNR” status. This means no life sustaining measures are to take place to prolong life. The certified nursing assistant will receive report form the charge nurse of the patient’s status. The certified nursing assistant may also find a patient’s status by reviewing the cardex. Review Text pages 818 in Mosby’s. Giving Emotional Support All caregivers find themselves in the position of providing emotional support to someone in crisis. That includes patients or their family/caregivers. The following are guidelines for professionals providing emotional support to persons facing serious illness. • Before you begin, close your eyes and take a few, slow, deep breaths. This allows you a moment to relax and become focused. • Acknowledge the situation. This communicates you care, and are open to hearing the details of the pain. Stay in the present moment as much as possible. • Be honest about your own thoughts, concerns, and feelings-particularly your helplessness and your honest desire to support that person in whatever manner best meets his/her needs. • Validate the person’s feelings. In a crisis, people need to know that the intense sadness, confusion, anger, fear, numbness, and helplessness, etc. are normal reactions to the abnormally stressful event of their loss. Summary: The certified nursing assistant can provide the family with care to assure that changing needs and goals are met to facilitate communication and continuity of care. Certified nursing assistants can help create a supportive, reassuring environment when the patient is dying. Each patient and family is unique in this experience. Warmth, understanding of patient/family needs sensitivity and emotional support during the dying process can be the greatest gift we can give to patients and families. Page 5 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Title: Regional Hospital: Care of the Surgical Patient Study Module for the Certified Nursing Assistant Purpose: This study module outlines basic Certified Nursing Assistant care provided to the surgical patient Competency: Provides all essential aspects of Certified Nursing Assistant care to the surgical patient Objectives: Upon completion of this module, the Certified Nursing Assistant will be able to: A. Prepare patient room B. Discuss changes in vital signs C. Observe respiratory function postoperatively D. Assess status of circulatory system postoperatively E. Discuss circulatory assessment in the patient room F. Ensure post-op ambulation G. Provide appropriate nutrition and fluids H. Promote comfort and maintain safety postoperatively Content: Post-Operative Phase A. Preparation on the Clinical Unit B. The Initial Assessment C. Respiratory Care D. Circulatory E. Urine Output F. Activity G. Nutrition and Fluids H. Comfort and Safety Required Activities: A. Provide care to patients B. Complete final exam with minimum score of 85% C. Read and study the Care of the Surgical Patient Study Module Approved By: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction: Many surgical patients are admitted to the hospital the morning of surgery. Occasionally, a patient scheduled for a major surgical procedure, may be admitted for preoperative care one to two days prior to surgery. The typical surgical patients seen here are hernia, hemorrhoids, D&C, gallbladder and abdominal surgery. Content: Post-operative Phase A. Preparation of the Clinical Unit 1. The patient room must be readied for the return of the patient. Prepare the bed by fan folding linen back and place cloth absorbent pad on bed. Then raise the bed to the high position for ease of transfer from the surgical cart to the bed. Place all equipment that is needed in the room (intermittent suction, PCA pump, infusion pump, CPM, oxygen and cardiac monitor). 2. Upon patient arrival to the room, the family may be asked to step outside until the patient has been transferred to the bed and assessment has been obtained. Obtain a report from the nurse. B. The Initial Assessment-This is to be done as soon as the patient is settled in bed. The assessment should include the following: 1. Urine output 2. Breathing 3. Blood Pressure/ TPR 4. O2 level 5. Bleeding, dressing, drainage 6. Side rails 7. Equipment C. Respiratory Care 1. Incentive Spirometry-Breathe in through mouthpiece as deeply as possible, hold breath 3 seconds, exhale; work at increasing respiratory effort. 2. Deep Breathing-Assist the patient to a semi-Fowler position with pillows supporting his back and shoulders. Instruct the patient to breathe out gently and fully as his ribs sink down and inward toward the midline. Instruct the patient to take a deep breath through his nose, letting his abdomen rise as the lungs fill with air. Instruct the patient to hold this for five counts. Repeat this sequence 5 to 10 times with a short rest after each group of five, being careful not to hyperventilate. 3. Coughing-Assist the patient to lean forward into a sitting position. A sitting position is the best position for matching ventilation and perfusion, for reducing abdominal pressure on the diaphragm, and for minimizing the risk of aspiration in patients-particularly those with nasogastric tubes. Instruct the patient to splint his incision with laced fingers or a pillow. Once sitting, take a deep breath through his nose, and then breathe out through his mouth. The patient should do this 3 times, holding the air for 3 seconds. After the third exhalation, the patient, with his mouth open, should take a quick deep breath and immediately cough strongly once or twice; follow coughing with another maximal deep breath to reinflate collapsed alveoli. Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ D. Circulatory-Deep Vein Thrombosis (blood clot) occurs in pelvic veins or in veins of the lower extremities 1. A blood clot is most common following general thoracic or abdominal surgery. Risk factors include: obesity, prolonged immobility, smoking, cancer, varicose veins, and dehydration. Apply TED’s or SCD’s if ordered. E. Urine output 1. Observing the ability to void is common in the post-operative period. If findings of retention, notify a nurse. 2. Observe and report urine output<30 cc per hour 3. Observe color F. Activity 1. Early ambulation has been a significant factor in hastening post-operative recovery and preventing post-operative complications. Numerous benefits are derived from the exercise of getting in and out of bed and walking during the early post-operative recovery. With each ambulation, the patient must be encouraged to walk farther. 2. Effects of early post-operative ambulation are as follows: a. Promotion of expulsion of flatus b. Prevention of abdominal distention and gas pains c. Prevention of constipation 3. Before the patient is to ambulate the first few times, assess the patient’s level of alertness/ability to follow directions, cardiovascular status, and motor status. 4. Be aware of any limitations to ambulation that were present pre-operatively. 5. When initially ambulating, place the patient in an almost upright position in bed until all dizziness has passed. Then, slowly assist the patient to a dangling position with legs hanging over the side of the bed. When the patient has fully adjusted to this position, he may be helped to stand at the bedside, and then walk. The Certified Nursing Assistant should be at his side to give both physical and moral support. It is a wise idea to have more than one person present to assist the patient during the first ambulation. 6. Adjust all tubing prior to ambulation. Clamp off the NG tube while the patient ambulates, then reconnect. 7. Maintain the urinary collection bag in a position lower than the bladder. Attach all IV bags to moveable posts. Be certain you have enough help to handle the patient and the equipment being moved, especially if the patient is weak. G. Nutrition and Fluids 1. Diet-start the patient with ice chips, then go to clear liquids. If the patient tolerates this, then you can try full liquids (soup, pudding, toast) 2. Diet will progress as ordered by the provider Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ H. Comfort and Safety 1. Level of Comfort-pain is common after nearly all types of surgical procedures in which there has been cutting, pulling and manipulation of tissues 2. The patient is asked for symptoms of discomfort after having been transferred to the bed and positioned in supportive body alignment 3. Assist the patient to rate the pain on the 1-10 pain scale 4. Observe the patient for signs of pain with movement, facial grimacing, and moaning 5. If the patient is using a PCA pump, reinstruct the patient the patient in its use. (As requested by the patient) 6. Safety-Bed side rails are kept raised until the patient is fully awake and responding to prevent the heavily medicated patient from falling 7. The patient is instructed early regarding the permissibility of ambulation and the need to call for assistance for initial attempts 8. The call light should be easily accessible to the patient Summary: In conclusion the Certified Nursing Assistant works closely with the RN to monitor and support recovery Page 4 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Name: _____________________ Score: _____________________ Regional Hospitals: Care of the Surgical Patient Final Exam for the Certified Nursing Assistant 1. The patient room is ready for the return of the patient by: A. B. C. D. Fan folding linen back and raising the bed Place all equipment needed in the room Obtain a report from the nurse All of the above 2. When the patient is transferred to the bed the initial assessment should include the Following: (list 3) A. ___________________________________________________________ B. ___________________________________________________________ C. ___________________________________________________________ 3. Respiratory care includes: A. ________________________________________ B. ________________________________________ C. ________________________________________ 4. True or False With a risk factor of blood clots you can apply TED hose or SCD’s. 5. True or False Urine output < than 30 cc/ per hour should be reported to the nurse 6. True or False Ambulation helps improve recovery and reduce complications 7. True or False Progression in diet is full liquids, clear liquids, ice chips. 8. Measures to promote comfort and safety include: A. B. C. D. Support body alignment Observe signs of pain Side rails up and call light in reach All of the above /CBO/NURSE ASSIST/HCMH/8/13/2004/ Care of Surgical Patient- Final Exam Answer Key 1. D 2. A. B. C. D. E. F. G. Urine output Breathing Blood pressure/TPR Oxygen level Bleeding, dressing, drainage Side rails Equipment 3. A. Incentive Spirometry B. Deep breathing C. Coughing 4. True 5. True 6. True 7. False 8. D Title: Regional Hospitals: Time Management Study Module for the Certified /CBO/NURSE ASSIST/HCMH/8/13/2004/ Nursing Assistant Purpose: A: This module focuses on organizational and time management skills. Competency: Provides all essential aspects of nursing care in an organized and timely manner. Objectives: Upon completion of this module the orientee will be able to: A. Discuss how to prioritize patient care. B. Discuss organizational skills related to patient care. C. Review time management format for each shift. D. Review intershift report guidelines. E. Complete time management format for each shift. Content: A. B. C. D. E. Time Management Concepts Priority-Setting Delegating Intershift Report Guidelines Conclusion Required Activities: A. B. Complete the reading material in this module. Complete the post-test with 90% accuracy. Approved By: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction: Since the eleventh century, society has treated the clock as a necessity. It is unusual to find people who do not wear wristwatches. Western culture is especially stringent on timeliness and not very forgiving of tardiness. In addition, a family’s view of time influences its members’ time management skills. Ours is a time-oriented society; faster is better. How we manage time can make us feel good and confident about ourselves or it can make us feel inadequate. Each of us has 24 hours or 1440 minutes in each day. Learning to control time instead of allowing time to control us is key to success. Many think time management is about doing more. If, in fact, doing more simply means having to do more work; there may be less desire to change. Time management does mean gaining maximum return on time invested. Managing time effectively results in taking less time to accomplish meaningful pursuits of work or leisure. Managing time effectively isn’t a simple skill; it’s a whole way of thinking, a way of approaching each day. It involves planning, organizing, delegating, and prioritizing. No matter how adept you get at time management, the human element that makes each day unique can upset the best of plans. Learn to control the chaos enough to enjoy the constantly changing environment in which you work. That is the challenge faced by all health care workers. A. Time Management Concepts When it comes to time management, an individual has two choices-organize or agonize. Everyone has the same number of hours in each day; each person chooses to use those hours in his/her own way. Time management is the use of personal and professional strategies to achieve desired goals in a designated time frame. Six time management principles are: • • • • • • Common • • • Write down your goals and prioritize them. Write down a list of daily activities that support the goals Do the most important activities first Ask what is the best us of time right now Handle each piece of paper only once Don’t procrastinate; do things now. obstacles to managing time effectively and to meeting goals are (Yoder-Wise, 1995): Interruptions Procrastination Perfection People can develop strategies to deal with these obstacles. Effective strategies for dealing with interruptions are: • Provide a momentary delay – “I can talk with you in five minutes, unless if it an emergency.” • Set up appointment – “I know I have assigned you some difficult tasks. Let’s check with each other at 0100 and 0230 unless something urgent comes up.” • Set a psychological framework – “How long do you think this will take?” • Stand, if you have been sitting to encourage the interrupter to be brief. • Use better screening – (to unit clerk) “I am going down the hall to see Mr. Jones; but I’ve put a call in to Dr. Anderson. If he calls, please get me.” Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • • • • • • • • • • Listen actively. Focus on the problem and action to take, not on who is at fault or how something went wrong. Reorganize your work area. Anticipate known deadlines and plan accordingly. Set goals Acknowledge your frustration; don’t let it take over. Complete one task at a time. Learn to say “No.” End conversations effectively. Say “Thank you.” Then stand and walk away. Use resources-e.g. unit clerk or another nurse-to take messages if you don’t want to be interrupted. Procrastination and perfectionism are time-consuming habits. Overcoming perfectionism takes a conscious effort. Always do your best, but best is not always perfect. Strategies for dealing with procrastination include: • • • Break a project/job into workable parts so the project/job is not overwhelming. Write notes to yourself to stay on target. Set a short time frame (i.e.- determine what can be done in the next five minutes and do it) Following are time management strategies: • • • • • • • • • • • • • • Chart someone other than in the place where you’ll be most accessible. Close your door or work elsewhere to prevent interruptions. Ask people to put their comments in writing-don’t let them catch you “on the run.” Let the unit clerk know the information you need immediately. Conduct a conversation in the hall to help keep it short or in a separate room to keep from being interrupted. When involved in a long procedure, ask someone else to cover your other responsibilities. Break projects into small, manageable tasks. Keep interruptions short-e.g., stand during phone calls. Keep your manager informed. Be aware if one person is typically your source of interruption. Have a to-do list that plans for you to be done early-e.g. 1 hour early. In hospitals, knowing transfers come at the end of a shift, be prepared. Be positive. Recognize that crises and interruptions are part of the job. Additional aids to time management include: • • • • • • Write things down—it is much easier to write things on a patient chart as they are done than to try and remember them later. Learn to say “NO”—one of the most difficult things for a sensitive caregiver to do is to say: no”. Before saying “no”, however, consider the amount of time the task will reasonably require. Also, weigh how much you value the activity you are declining. Use energy effective—define the time of day when you energy is highest. You might want to undertake the priority tasks at these times. Find privacy—it is important to have uninterrupted quiet time. Minimize interruptions—interruptions can break a thought process in such a way as to increase the amount of time it takes to complete a task. Identify your primary interruptions, whether they are telephone calls, visitors, or other interruptions. It is often difficult to avoid interruptions; you may need to be assertive in informing others that you need time alone to perform certain tasks. Avoid paper shuffling—many experts in time management state that a person should only “touch a paper once”. This principle helps avoid the time-consuming tendency of stacking papers or notes or re-stacking them. Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • • • • • B. Limit socializing—health care is difficult and our social contacts at work are important to job satisfaction and our mental health. Good time managers do not ignore the importance of socialization, but strike a balance that leaves time for completing job duties effectively. Limit phone calls—endless social calls are time wasters. Control your own outgoing calls and the time spent on incoming ones. You could say, “I only have a couple of minutes to talk.” Delegate—four guidelines for successful delegation are: • Be able to psychologically let go of the task • Choose a capable person to whom to delegate • Clearly describe what is to be done • Give praise when the task is accomplished A health care team works best when there is mutual delegation. Being a “team player” means being considerate of others and accepting appropriate duties delegated to you. It is only fair that if you delegate to others you are also willing to accept an appropriate take that is delegated to you. Avoid procrastination—procrastination is defined as the chronic delay in implementing actions that accomplish important tasks. Procrastination is neither good nor bad. When nurses procrastinate in areas related to patient care, supervisors and co-workers may view the procrastinator as undependable and incompetent. The trust relationship between the nurse and patient may also be severed because the nurse feels the patient request is unimportant. Tasks can be more manageable when broken into pieces and done one part at a time. An important step is to make a personal commitment for completion of a task by a deadline. Audio taping intershift report—taping the intershift report is a time saver. Taping has many advantages, such as eliminating social and unrelated comments from listeners. It can be done at a convenient time near the end of the shift. Nurses can remain on the unit after taping report to meet patient needs while the next shift listens to report. The disadvantage is the ability to clarify information while listening to report. Making notes ahead of time can be useful. Priority-Setting Stephen Coven (1990) has developed the following classification of priorities. IMPORTANT URGENT Cell A Items: Cell B Items: Cell C Items: Cell D Items: Yes Yes A No C No B D Must be done as they are urgent and important (i.e., passing a stat medication) These items are important, but not urgent. Responding to these items is the real key to productivity (i.e., walking a patient) These items are urgent but not important and may not contribute to overall goal (i.e., - responding to a personal phone call) Neither important nor urgent (i.e., - cleaning the coffee pot) Page 4 C. Delegating /CBO/NURSE ASSIST/HCMH/8/13/2004/ Delegation is critical in the health care system today. The American Nurses Association (1994) has defined delegation as the transfer of responsibility, but not accountability, for the performance of an activity to another individual. Advantages of delegation (Hansten and Washburn, 1998) are as follows: • Patients receive high-quality care when they wouldn’t have had as much attention without assistive personnel. Nurses have better opportunities for patient management, discharge planning, and communication with families and other health care team members. Both nurses and assistants enhance their sense of participation and belonging. The work team is more efficient and productive, with a subsequent reduction in overtime. Delegation brings about a sense of increased support—nurses feel less pressured to do everything alone. • • • • Hansten • • • • • • • • • • • • • • and Washburn (1998) also identified barriers to delegation experienced by nurses: Not wanting to take the risk. Not trusting others to do the jobs assigned. Letting go of some of the amenities or technical tasks. Fear of loss of control. Overcoming old habits. Needing to cross tasks off the list. If I don’t do what I’m used to doing, what’s left for me to do. Needing help with organization of work. Wondering if you can still be a nurse if you don’t do it all.(Super nurse syndrome). Wanting to be liked. Assuming the other staff is too busy to be bothered (Super martyr syndrome). Uncertain about rules/regulations. Feeling you can do better by yourself (Am I a real nurse when I delegate?). Thinking it takes too much time to teach other personnel. When delegating, remember the five rights: (National Council of State Boards of Nursing, 1990) • Right task—one that can be delegated. • Right person—one qualified to do the job. • Right direction/communication-clear, concise description of the objective and your expectations. • Right supervisor/feedback—evaluation in a timely manner, during and after the task is completed. • Right circumstances-appropriate patient status and provider capabilities. Trust is crucial to the delegation process. Whenever patient care is provided by someone other than a registered nurse, the accountability for the care remains with the delegate. In addition. assistive personnel must accept the delegated task and be competent at completing the task. Feedback to the delegated is necessary. D. Intershift Report Guidelines In • • • the acute care and skilled care settings, intershift report is an important communication tool. Identify the room number, patient’s name, patient’s age, and patient’s doctor(s). Identify patient’s diagnosis-list procedures or surgeries-no code status is applicable. Give pertinent information: • IV solution and IV credit • Appearance of dressing, time of dressing change if applicable • Surgical drains (types of drainage and amount) Page 5 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • E. • Pain medication given and patient’s response • Circulation and neuro checks • Most recent vital signs • Change in patient condition, calls to M.D., actions taken • Restrictions, (i.e., NPO for a test for fasting labs, fluid restriction) • Accu-check readings—oral agent or insulin administered • Patient’s emotional status if pertinent • Activity level and patient’s tolerance • Breath and bowel sounds if applicable • Patient/family education needs Make your information organized before you start report. Give report in a logical and concise manner. Stick to the facts. Conclusion There is less time available for each of us to do all things. We are just in the habit of using our time in much less productive ways. Did you ever stop to realize that we each have: • • • • 24 hours per day 168 hours per week 720 hours per month 8,760 hours per year According to Henry Ford, “People who have no time don’t think. The more you think, the more time you have". REFERENCES American Nurses Association (1994). Registered Professional Nurses and Unlicensed Assistive Personnel. Washington, D.C.: Author. Ball, K. (May/June 1999). Putting first things first. Today’s Surgical Nurse, 3-5. Covey, S.R. (1990). The seven habits of highly effective people: Powerful lessons in personal change. New York: Simon and Schuster. Dawes, B.S.G (September 1999). Perspectives on priorities, time management, and patient care. Aorn Journal, 374-377. Hansten, R.I. & Washburn, M.J. (1998). Clinical delegation skills: A handbook for nurses. Gaithersburg, MD: Aspen. Huber, D. (2000). Leadership and nursing care management. Philadelphia: W.B. Saunders. Lombardi, D.N. (2001). Handbook for the new health care manager. Chicago: Jossey-Bass. National Council of State Boards of Nursing. (1990). Concept paper on delegation. Chicago: Author. Page 6 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Name: _____________________ Score: _____________________ Regional Hospitals: Time Management Final Exam for the Certified Nursing Assistant Identify each as an appropriate or inappropriate time management tool: 1. Appropriate Inappropriate Write down your goals and prioritize them. 2. Appropriate Inappropriate Procrastinate. 3. Appropriate Inappropriate Review all pieces of paper, shuffle them into piles alphabetically, and then go on break 4. Appropriate Inappropriate Do the most important things first. 5. Appropriate Inappropriate Ask what is the best use of time right now. 6. Appropriate Inappropriate Focus on the problem and what actions to take. not on who is at fault. 7. Appropriate Inappropriate Say Ayes=to every request that comes your way. 8. Appropriate Inappropriate Anticipate known deadlines and plan accordingly. 9. Appropriate Inappropriate Accept only perfectionism. 10. Appropriate Inappropriate Break a project or job into workable parts. 11. Appropriate Inappropriate Chart in a place where you will receive minimal disruptions. 12. Appropriate Inappropriate Keep your manager informed. 13. Appropriate Inappropriate Be positive. 14. Appropriate Inappropriate Recognize that crisis and interruptions are part of the job. 15. Appropriate Inappropriate Take and make personal phone calls frequently throughout the shift. Page 1 Regional Hospitals: Time Management Final Exam for the Certified Nursing Assistant /CBO/NURSE ASSIST/HCMH/8/13/2004/ 16-20. Identify the five rights of delegation; • • • • • 21. Prioritize the following patients according to their need to be seen: a. _____ A patient with CHF requesting a laxative for complaint of constipation x 3 days. b. _____ A patient receiving blood that had complained of some of some shortness of of breath on the previous shift. c. _____ A patient on fluid restrictions requesting ice chips. d. _____ A patient with cancer who rates his pain level at an I on the scale. 22. The a. b. c. d. following is/are an obstacle(s) to managing time effectively: Interruptions Procrastination Perfectionism All of the above 23. T F Trust is essential to the delegation process. 24. T F It is difficult to walk to Pharmacy to get medications you need that are not in in the patient’s medication drawer. 25. T F Nursing staff is to take a one-half hour lunch/supper/dinner break. /CBO/NURSE ASSIST/HCMH/8/13/2004/ Time Management Final Exam Answer Key 1. Appropriate 2. Inappropriate 3. Inappropriate 4. Appropriate 5. Appropriate 6. Appropriate 7. Inappropriate 8. Appropriate 9. Inappropriate 10. Appropriate 11. Appropriate 12. Appropriate 13. Appropriate 14. Appropriate 15. Inappropriate 16-20. Right task Right person Right direction/communication Right supervision/feedback Right circumstances 21. A-3 B-1 C-4 D-2 22. D 23. T 24. F 25. T /CBO/NURSE ASSIST/HCMH/8/13/2004/ Title: Regional Hospitals: Loss and Grief Study Module for the Certified Nursing Assistant Purpose: Most people relate loss and grief only with a dying patient; this module focuses on loss and grief related to loss of control, loss of body image, loss of self-esteem, loss of body part(s) or function(s), loss of sexuality, loss of role performance, loss of social role, poor prognosis, cancer, and loss of life. Competency: Implements appropriate nursing care when caring for a patient/family experiencing a loss. Objectives: Upon completion of the study module the orientee will: A. Discuss the three stages of illness. B. Discuss the four grief stages C. Discuss a person’s common feelings/reactions in each of the grief stages. Content: A. B. Stages of Illness Death and Dying Required Activities: A. Study and complete activities in this module. B. Read about the following located in the facility Policy and Procedure Guide. • Care of the dying patient • Advance Directives/Do Not Resuscitate C. Complete final exam with minimum accuracy of 90%. Approved By: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction In this module, loss and grief as experienced by patients and families are reviewed. Most people relate loss and grief only with a dying patient; this module focuses on loss and grief related to: • • • • • • • • • Loss of control Loss of body image Loss of self-esteem Loss of body part(s) or function(s) Loss of sexuality Loss of role performance Loss of social role Poor prognosis/cancer Loss of life The experience of illness precipitates many stressful feelings and reactions. These include frustration, anxiety, Anger, denial, shame, grief, loss, and uncertainty. Patients and their families need to adapt to the demands of the different stages of illness. Painful and disturbing symptoms lead to diagnostic tests and medical treatment. There are often dreaded questions about prognosis, body changes, and the reactions of other. Hospitalization is a major stressor. Although necessary and often life saving, it plunges people into an unfamiliar and often frightening environment where they feel vulnerable and out of control. Serious illness or injury is always more than just physical pain and inconvenience. A person’s life goals, family, work, income, mobility, body image, and life style may be drastically altered. Whether the changes are temporary or permanent, the situation may develop into a crisis for the person—a crisis that affects family, friends, and professional caregivers. To be of optimal help to patients, families, staff, and themselves, the nurse needs to know the following: 1. 2. 3. 4. 5. The usual stages of illness and various emotional responses The major tasks of adapting to significant illness or injury The typical coping strategies used by patients and families The psychological and social factors that help or hinder coping His/her own reactions to the various stresses and how to deal with them The transition from health to illness is a complex and highly individualized experience. In addition to restoring physiologic balance, the two main tasks of the patient are: 1. To modify the body image, concept of self, and relations to other people and work 2. To readjust realistically to the limitations imposed by the condition Each patient has a mental and social picture of himself/herself that is based on multiple experiences in the past, present, and anticipated future. Serious illness and injury abruptly interfere with that self-concept. Adapting to the changes imposed by illness can affect the patient’s sense of identity. An important aspect of the total self-image that is often affected by physical changes is the perception of one’s physical self as separate and distinct from all others. Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ This perception is based on inner sensations and functioning as well as on information derived from the external environment. Society prescribes norms of physical appearance and behavior. The perception body image operates on both conscious and unconscious levels. Threats to the body image and self-esteem are recognizable in many nursing situations. Feelings of shame, inadequacy, and guilt may be precipitated, depending on the patient’s definition of the situation. Violation of modesty and invasion of privacy causes anxiety and embarrassment. Exposure of the body during physical examinations and treatments may be upsetting, even though expected as part of the regime. Disturbances in the usual elimination process and need for using a bedpan or talking about bowel and bladder habits threatens self-esteem. This is a major problem for patients requiring surgery that produces such drastic changes as a colostomy or ileostomy. Major changes in body image are brought about by amputation of a limb or a breast (mastectomy), by surgery on the reproductive organs, hair shaved for brain surgery, or even the surgical scar itself. The reaction of the body to radiation treatment may threaten body image, as may change skin color, such as occurs in jaundice. A. STAGES OF ILLNESS • Initial Stage The development of symptoms is usually accompanied by unpleasant sensations, loss of vigor and stamina, and a decrease in the ability to function. To ward off the prospect of sickness, a person may plunge into activity, keeping late hours with extra work and social activities. Another individual may become passive and withdrawn, hoping vague symptoms will go away. A person may put off seeking medical care for fear of the diagnosis, especially if something serious is suspected, such as cancer Anxiety, guilt, shame, and denial is prominent during this initial phase. • Second Stage The patient recognizes and admits that he/she is sick and in need of help from others, especially from the medical and nursing staff. In this stage, the patient becomes preoccupied with himself/herself, symptoms, and treatment. The patient’s behavior is often regressive. During the stage of accepted illness, the patient may express anger, guilt, and resentment. He/She may be very critical of care and medical management, attacking the very people he/she depends on. The most helpful nursing approach at this time is to view this reaction as the person’s attempt to deal with the situation. Do not take it personally! The nurse should encourage the expression of feelings without passing judgment, moralizing, or arguing. Labeling the feelings (i.e. “This must be difficult to believe” or “You must be feeling a loss of control”) will encourage the patient to verbalize fears. During this stage, the patient may be experiencing an acute sense of loss. The clinical picture is depression with sadness, hopelessness, and anger. He/She may be mourning the loss of health and vigor, the loss of a body part or function, or a change in job and family. He/She may be moving into the emotional reactions to dying. Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • Third Stage The third stage is the convalescent or restitution period. The return of health and physical strength often precedes the patient’s feeling and acting “well.” Just as lag usually occurs in the initial stage between the appearance of physical symptoms and the emotional acceptance of illness, a reverse lag occurs in recovery. Getting well implies giving up a dependent, regressive position and resuming adult responsibilities and normal relations with others. Although some people are reluctant to give up the patient role, more are motivated toward health but are afraid or hesitant to try out new skills. This is particularly true if the illness and treatment require major changes in work and family relations. The nurse helps patients in this stage by assuming a role analogous to that of a parent of a teenager. He/She gradually relaxes protection and offers guidance, advice, and encouragement to progress. He/She quietly retires to the sidelines, ready to reassure but encourages experimentation with new skills. He/She steps in only when gross errors in judgment occur. The patient senses the confidence of the nurse and is reassured. During the convalescent stage, the nurse can stimulate the patient to renew an interest in the world, communicate better with family, and make plans for the future. For example, there are support groups for people who have had strokes, heart attacks, open-heart surgery, mastectomies, ostomies, cancer, and other conditions. A member of one of these groups may be called upon to talk to the patient both before and after surgery to convey hope and to give realistic, first-hand information on coping with his/her common disability. Grief is a complex emotional response to the anticipated or actual loss of someone or something valued. The loss may be that of a relative or friend, a part of the body, a job health, or life. Feelings of anxiety, helplessness, hopelessness, guilt, anger, depression, remorse, sadness, and loneliness are part of grief. Mourning refers to the process that follows the loss and ultimately results in overcoming the grief. Grief and mourning involve social responses that are best dealt with by the inclusion of others. There are many cultural factors involved in the specific way in which grief and mourning take place, from the extremes of a stoic appearance to elaborate and ritualistic weeping, and public display. The intensity of grief and mourning depends on the significance and extent of the loss to the person. The stages of mourning are similar to the stages of adaptation to illness: shock and disbelief, awareness, and restitution. Nursing interventions to help patients and families who experience grief and mourning include: 1. 2. 3. Anticipate reactions to loss Support their usual coping mechanisms Allow expression of feelings The nurse should provide privacy and availability of self and others who can provide support. When a body part or function is lost, the nurse should design a specific plan of care to prevent additional loss of self-esteem. The presence and willingness of the nurse to participate in the painful experiences that Accompany grief help to prevent feelings of total abandonment. By being aware of the usual patterns of grief and the need for other types of therapeutic intervention, such as Reach to Recovery for a mastectomy patient, Patients and their families’ can be supported. Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ B. Death and Dying Most patients have hoped for and expected a long and healthy life. A serious illness raises questions of vulnerability and uncertainty about the future. The purpose of hope is to ward off despair, which is characterized by mental anguish, disorganization, helplessness, and hopelessness. Loss of hope leads to giving up those behaviors that lead to physical and emotional equilibrium. Death may result from the loss of the will to live. Hope activates the motivational system. It is reinforced by other people (doctors, nurses, family members) who give support and encouragement to continue the struggle. When patients see “the light at the end of the tunnel,” they can persist in moving toward future goals of improved functioning. Even with patients who have a poor prognosis of who are dying, hope for meaningful living in the present or for relief of suffering are important aspects that can be reinforced with nursing care. For most people, just the thought of death is frightening and even impossible. Regardless of religious beliefs, it is difficult to imagine oneself not existing in the world. Nurses are deeply committed to life and health. The dying patient is a direct contraindication to that commitment. Sometimes the medical and nursing staff react to dying patients as if they represent a failure of their skill and care. Although nothing can be done to reverse the ultimate process, dying patients and their families can be helped during the final days. People face death in many ways. According to Kubler-Ross (1969), the emotional responses of a person facing death can be traced through five phases: 1. 2. 3. 4. 5. Denial and isolation Anger Bargaining Depression Acceptance • DENIAL-Denial permits hope to exist. Often, patients are ready to accept the fact that they are dying, but the family continues to express denial. This delays communication of concerns. Denial and isolation are interrupted when the patient begins to think about unfinished business: personal affairs, finances, and arrangements for spouse, children, and others. • ANGER-The next emotion expressed is anger. The question, “Why me?” does not require an answer, but the patient is helped if the nurse is present to listen and to offer support. The behavior of patients in this stage is difficult because nothing can be done that seems to please. Nurses can expect this expression of anger and should not take it personally. Patients often want to express their sense of outrage and helplessness. When feelings have been vented, they are able to move on. • BARGAINING-Bargaining is a phase of coping during which the dying person attempts to negotiate a trade. Usually, it involves a deal with their God, the physician, or the nurse: “If I can live long enough to attend my son’s wedding, I’ll be ready to die.” If at all possible, patients should be granted their requests. • DEPRESSION- The full impact of the inevitable is apparent to patients in the depression stage. Defense mechanisms are no longer effective; sadness and anguish are felt and expressed by crying. They also elicit the support of loved ones and nurses. /CBO/NURSE ASSIST/HCMH/8/13/2004/ • ACCEPTANCE-Acceptance is a time of relative peace. The patient seems to want to review the past and contemplate the unknown future. Often, patients do not talk a great deal but want others nearby. If pain is relieved, the person who has accepted death often wants to be comforted by having contact with those who are meaningful. Emotional demands on the nurse are often continuous and draining. Without proper understanding and coping skills, the cumulative effects may be overwhelming and may lead to professional and personal problems. Although caring for a dying patient is an emotional strain, nurses can become the most important link with life for a dying patient by promoting comfort and providing emotional support. REFERENCES Smeltzer, S.C. & Bare, B.G. (2000). Textbook of Medical-Surgical Nursing. Philadelphia: Lippincott. Page 5 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Name: _____________________ Score: _____________________ Regional Hospitals: Loss and Grief Final Exam for the Certified Nursing Assistant 1. T F Hospitalization is a major stress for patients, 2. T F A patient experiences loss of body image following a mastectomy. 3. T F A patient experiences an acute sense of loss in the “accepted illness” phase. 4. T F In the convalescent period, the nurse should offer guidance, advice and encouragement. 5. T F The intensity of grief and mourning depends on the significance and extent of the loss to the person. 6. T F When a seriously ill patient verbally attacks the nurse and complains of the the poor nursing care, it should be send as probably a manifestation of the patient’s loss if there is no data to support poor care. 7. T F Patients who have had a mastectomy, ostomy, or head injury should be encouraged to participate in support groups. 8. T F Long-term hospitalization can cause loss of role performance and/or of social role. 9. T F The emotional responses of a person facing death can be raced through ten stages. 10. T F Acceptance of death is a time of relative peace. /CBO/NURSE ASSIST/HCMH/8/13/2004/ Loss and Grief Final Exam Answer Key 1. True 2. True 3. True 4. True 5. True 6. True 7. True 8. True 9. False 10. True /CBO/NURSE ASSIST/HCMH/8/13/2004/ Regional Hospital: Conflict Management Study Module for the Certified Nursing Assistant Purpose: Conflict and conflict resolution measures are delineated. Competency: Uses conflict management skills appropriately. Objectives: Upon completion of this module, the orientee: A. Practice the five basic communication techniques to increase confidence, verbal effectiveness, and personal power B. Discuss how to manage unexpected confrontations. C. Identify various personality styles and ways to work effectively with people. D. Demonstrate effective listening skills. Content: A. B. C. D. E. F. Unexpected Confrontations Personalities Tact Listening Skills Conclusion Bibliography Required Activities: A. B. Read and study activities in this module. There is no final exam for this module. Approved by: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction: Stressful situations arise in our everyday lives, whether it is at home or at work. How an individual handles oneself in difficult situations depends on his/her level of confidence. Studies have shown five basic communication techniques that can help increase confidence, verbal effectiveness, and personal power: 1. Relaxing 2. Visualizing 3. Affirming 4. Scripting 5. Practicing A. 1. Relaxing: The more physically relaxed one is, the better his/her concentration and mental focus. Being Relaxed can help in a difficult conversation by reducing stress, tension, and anxiety. 2. Visualizing: This ancient process is using one’s minds eye to create mental pictures of something he/she would like to achieve, such as, resolving an issue between self and a friend. Visualizing helps one feel more confident about creating a successful outcome. It helps to dissolve fear and doubts about what can be achieved. 3. Affirmation: Confidence building statements are called affirmations. This is self-talk that one says aloud or silently. Many times “self talk” raises doubts, worries, and other counterproductive thoughts that hinder achievement. Affirmations are a way of replacing old self-talk patterns of disapproval and skepticism with more optimistic suggestions that promote success. For example, a strong affirmation would state, “I will success in this orientation.” A weak affirmation would state, “I hope I do good in this orientation. Strong affirmations help build confidence. 4. Scripting: Scripting is nothing more than writing down what you want to say. This technique provides a game plan to follow to help so that one stays calm in a difficult conversation. It is difficult to say what one means with confidence if he/she is just “winging it.” Knowing what one wants to say keeps one focused on the big picture. It does not let one get sidetracked into counterproductive arguments over irrelevant details. 5. Practicing: Practicing what to say before entering a difficult conversation helps one to be calm; it allows a person to internalize and adopt a conversation game plan. As an effective communicator, how one speaks is more important than what a person says. Studies show that as little as 10 percent of a message is based on words; 90 percent is based on body language and tone of voice. Unexpected Confrontations Keeping calm is the most effective way to handle unexpected confrontations. Research has defined a four point alternative strategy for coping with unexpected verbal confrontations that allows a person to regain composure, remain calm, and defuse an emotionally challenging situation. Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • Don’t’ fight back; verbal attacks result in an adrenaline rush that causes the body to react. Ears get hot, eyes narrow, and the heart beats more rapidly. Meanwhile, the mind searches frantically for ammunition to sling back at the attacker. Research indicates few confrontations stop at this point. The result is more volatile, insults and accusations and usually the disagreement ends with someone saying something he/she will regret. No one wins in this situation. The best response is to do nothing—except listen. Make it your goal to understand the nature of the attack so that eventually a reasonable compromise can be reached. • Exercise self control-this will help regain composure after the initial shock of the unexpected attack. Relax and focus on the reasons for the assault. Then set the ground rules for communication such as, “Why don’t you take a moment to calm down, then we’ll talk”, rather than reacting to the other person’s hostility. • Listen, sympathize, and acknowledge feelings-concede to the person’s right to feel the way he/she does even if you disagree. Using acknowledgment strategy allows a person to stay calm and objective without having to defend. Use reflective listening skills to show empathy; understand the attackers’ feeling. This action tends to defuse the conflict. It also gives more time to get the facts and assess the situation so one can decide how to respond. Perhaps one will discover that the attacker has blown the incident way out of proportion, misunderstood information, misinterpreted a statement or action, is trying to cover up a larger issue, or has just made you aware of a genuine complaint that needs attention. • Guide the other person to an acceptable compromise-once the problem has been seen from the other person’s perspective, it can be discussed and outcomes discovered. Each person needs to look at the issue from the other perspective. Once this is done, solutions for compromise will surface. Conflicts arise, but can be dealt with in a controlled and reasonable manner. Relaxing the mind and body, visualizing positive results, using affirmation, scripting the game plan, and rehearsing sets the stage for success in challenging conversations. In addition, speaking assertively allows a person to make a positive statement or request and then allows him/her to be ready to respond to a possible objection, refusal or the disapproval of the listener. It is assertiveness and persistence-not how aggressively one speaks or acts-that reflects confidence. By using both assertiveness and tact in stressful conversations a person can get his/her point across to others without resorting to shouting or insensitive comments. Keep in mind, however, that it is vital to get to the root of the issue before the other person pleads innocence, counterattacks, or changes the subject. Assertive communication allows people with different viewpoints and goals to minimize friction by reaching mutually acceptable compromises. By using both assertiveness and tact in stressful conversations, views can be shared without resorting to shouting or insensitive comments. When speaking assertively, others are more likely to listen and respect feelings, opinions, judgments, and viewpoints. Speaking calmly improves one’s ability to communicate and encourages receptivity in others. Aggressive statements often contain criticisms and accusations while assertive statements reveal a speaker’s feelings and wishes. Assertive statements are effective as long as they are fait and said clearly and calmly. Flexibility and compromise are as important as assertiveness in any conversation. Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ B. Personalities People’s personalities play a large role in how they present themselves, and in the way one needs to deal with them. Personality examples follow: • A STEAMROLLER is the person who shouts, bangs his/her hands on the table, and is hostile and abusive. This person hopes the other will cave in; the goal is to squash any opposition. The steamroller sounds like: “How could you be so stupid!” or “This is what we’re going to do, and I don’t want to hear another word about it! Steamrollers want to dominate others and they know they can get away with their aggressive behaviors, as many people would rather give in than fight. Research suggests that if one is dealing with a steamroller, unfold the arms, look him/her square in the eyes, say his/her name, and tell him/her you don’t agree. Some suggestions include, “Mr. X, I disagree with you.” Or, “Mrs. Y, I don’t see it that way. In my opinion…”Steamrollers love to fight and they usually win. By not feeding into they’re bullying, staying calm, and avoiding provocative statements you can keep the steamroller from getting all worked up. • Another prickly personality is the “KNOW-IT-ALL”. These people feel compelled to impress and dominate with what they believe to be their vast experience and superior knowledge. They see themselves as experts and have the right answer to any problem. They try to overwhelm with facts to prove they are right and to minimize the listener’s level of understanding. It is possible to question the know-it-all’s advice without getting into an argument or making him/her snubbed by using this three point strategy:) Restate the main points; 2) Ask detailed follow-up questions; 3) ask for a solution to a worst-case scenario. Restating shows that one is listening and understands what has been said. Asking follow-up questions shows consideration for what the know-it-all has suggested, but also indicates fuzziness on the finer points. Asking for a worst-case scenario solution allows the know-it-all to problem solve a possible solution. Know-it-alls are very impressed with their logic, but this allows them to come up with other possibilities and often they will back off—for the moment. • The BUSHWHACKER is the person who ambushes with deadly innuendoes, sarcastic remarks and humor—at the listener’s expense. These people do not use head-on confrontation but are devious and use indirect attacks to chip away at one’s credibility. They play to an audience so they can boost their own status while putting others on the spot. A bushwhacker sounds like this, “Oh, a new dress! Did your husband finally break down, or do you have a “secret friend” that buys you clothes on sale at K-Mart? (Ha, ha, ha,).” If you say nothing, expect the behavior to continue. Most bushwhackers hate confrontation; so force them out into the open. Co-workers and friends are noticing how you deal with, (or don’t deal with), these quietly aggressive individuals. Sometimes simply drawing attention to the bushwhacker will stop the behavior, “I’m sorry Mike, but I didn’t quite hear what you just said—would you mind repeating that?” Or “You made a comment I didn’t hear. Why don’t you share it with everyone? ---Go ahead, you have the floor!” Be prepared for more sarcastic, snide remarks. It’s good to show a sense of humor, but now the pressure can be put on the bushwhacker by asking for negative feedback. “What is it about…that you don’t like?” Page 4 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • The WET BLANKET is a person who is gloomy and deflates other people’s goals and dreams. They have innumerable reasons not to do things or take risks. They have a negative attitude that spreads like a dark cloud. They say demoralizing comments such as: “You want to do what?” or “Why bother? No one will notice anyway.” Use this four-step approach to encounter the Wet Blanket’s cynical attitudes: 1. Do not argue, rather listen and rephrase: 2. Acknowledge the Wet Blanket’s viewpoint: 3. Say you are going to take the risk anyway: 4. Ask the Wet Blanket to help These people have unlimited reasons for not doing things. Arguing only stimulates more negativity. Instead of arguing, rephrase what he or she has said and zero in on the key points. Do and Don’ts when dealing with difficult personalities: • • • • • • • • • Do remain persistent even though you may feel like giving in. Don’t respond immediately. Take a deep breath and count to ten. Do listen for areas of agreement. Don’t fight or get caught u in arguing over details. Do think about what you want to say and then say it. Don’t be overwhelmed by an aggressive person’s behavior. Do exercise your right to reject a pushy person’s advice. Don’t let negative people squelch your enthusiasm or rob you of your dreams. Do stick up for yourself; verbally aggressive people will respect you and be less inclined to pressure you in the future. Don’t give up on yourself if an aggressive person overwhelms you. Practice your assertive skills and be ready for that person the next time. • C. Tact Tact is defined as the ability to recognize the delicacy of a situation and then to say the most considerate or more appropriate thing. Tact requires sensitivity to others, combined with the skill to speak assertively at any given time without giving offense. Tact requires ingenuity and the ability to know what will make a person feel better after talking. There is an easy way to learn the basic elements of tact. Each letter of the word T-A-C-T-F-U-L stands for one of seven strategies that will help one say the right thing in any sticky conversation. T Think before you speak Avoid tactless comments by thinking about what you want to say and how you want to say it before talking. A Apologize quickly when you blunder The trick is to recognize the mistake. Turning into the other person’s verbal and nonverbal reactions will help determine if an apology is in order. Acknowledge the mistake; do no make elaborate excuses. Apologize with a touch of humility and change the subject to something upbeat. C Converse, don’t compete Do you approach conversations, as a competition in which there is a winner and a loser? Do not make it your aim to fascinate people with your knowledge and verbal skill by punching holes in their opinions, arguing over details, or correcting their mistakes. You’ll certainly make an impression, but probably not the one you desired. Page 5 /CBO/NURSE ASSIST/HCMH/8/13/2004/ T F D. Time your comments Before beginning a conversation, be sure the other person wants to listen. Conversational timing improves when the speaker and the listener: • Agree upon a time to talk • Get right to the point • Do no insist upon an immediate response or agreement • Show a willingness to listen Focus on behavior—not on personality The tactful approach is to identify the annoying behavior rather than focus on his/her personality. remember it is easier for a person to change specific, identifiable actions than it is to alter his or her entire character. Point out that the behavioral upsets you, even if you know he/she is trying to help. Be sure to do this in private, so as not to embarrass anyone. U Uncover hidden feelings Saying things tactfully is more likely if an attempt is made to uncover and understand the other person’s feelings. L Listen for feedback Poor listening skills frequently lead to tactless comments. Criticism or indiscreet remarks often stem from a desire to dominate the conversation without considering what the other person has to say. However, when one listens carefully for feedback and reactions, he/she will know if the conversational partner is listening and understands. Listening Skills The literature identifies ten ways to improve listening skills: • Eliminate internal and external distractions External and internal distractions are the major factors that interfere with listening. Therefore to truly be effective, eliminate as many distractions as possible. It is crucial to give people complete attention so that the focus can be body language, what is said, what is not said, and what feelings and meanings the words imply. External distractions include a blaring television, a radio, screaming children, telephones, and playing with a pencil, doodling, or performing some other task while the other person is speaking. Internal distractions, while less obvious are equally detrimental to listening. These include daydreaming, worrying, tuning out, excessive note taking, focusing only on facts, or mentally debating with the speaker. • Encourage the other person to speak first Ask the other person to speak first. There are three reasons to encourage another person to present his/her views first: listening shows good etiquette and a desire to consider another person’s viewpoint objectively, encourages the other person to talk and reduces competition in the conversation, and it helps identify areas of agreement. • Use and observe body language Body language speaks loudly. It sends a message of interest or boredom. A listener’s closed or disinterested body language makes a speaker feel self conscious and less willing to share. When trying to communicate with someone, show interest in him/her. Smile casually, uncross the arms, keep hands away from the face, lean forward slightly, make frequent eye contact, and nod the head. Focus your attention on how something is said as well as on what is said. Zero in on the speaker’s sensitive areas, concerns, and hidden feelings. This listening between the lines helps prevent tactless comments, which can offend or lead to an argument. Page 6 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • Avoid unnecessary interruptions Good listeners do not interrupt a speaker; make trivial points, or petty corrections, or abrupt changes of topic; or complete an unfinished sentence. Interrupt with relevant questions or comments that advance a discussion toward a conclusion. Also, interrupt if an important fact was missed or a concept is not understood. • Listen for key words These words convey information and show interest and emotions. • Use reflective listening Rephrasing comments is one of the best ways to use reflective listening. It demonstrated listening and understanding. • Clarify implied statements Implied statements confuse communication because the poor listener often misinterprets the speaker’s meaning or purpose, which leads to verbal blunders or arguments. The first step in overcoming this communication problem is to listen carefully for a speaker’s Adloaded ≅ statements or questions, which imply much more than he/she is saying. A speaker’s tone of voice and the words he or she emphasizes reveal a great deal. • Identify and focus on main points While it may be tempting to debate the finer details of an issue, identifying and focusing on a speaker’s main points helps a person to see the “big picture.” Avoiding a focus on trivial facts eliminates wasted time and false assumptions. A good listener traces the development of the speaker’s main ideas and then makes an effort to predict where these important points are leading. This listening skill helps a person to stay actively involved in the conversation and determines how effective the communication is. • Silently review and order main points: then draw conclusions. There comes a time in most conversations where you can steal a few moments to mentally review and order the main points made by the other person, starting with what the listener believes the speaker considers the most important. This eliminates irrelevant details and allows the listener to focus on, and remember the speaker’s main points and ideas. This also provides an opportunity to ask follow-up questions. • Acknowledge the speakers’ viewpoint Acknowledging the speaker’s viewpoint sets the tone for open communication. Whether one agrees or disagrees with a particular view, everyone is entitled to his/her viewpoint. E. Conclusion Conflict occurs in everyone’s life, at home, at school, at work, and at social events. Yet there is much one can do to understand conflict and to defuse conflict. Basic communication techniques, a knowledge of personality styles, using tact, and using effective listening skills are helpful. Page 7 /CBO/NURSE ASSIST/HCMH/8/13/2004/ BIBLIOGRAPHY Badger, J.M. (1995). 14 tips for managing stress on the job. American Journal of Nursing, 95 (9), 31-33. Collins, M.A., (1996). The relation of work stress, hardiness, and burnout among full-time hospital staff Nurse. Journal of Nursing Staff Development. 12(2), 81-85. Costantino, C.A., & Merchant, S.P., (1989). Designing conflict management systems. (pp. 12-33). Droppleman, P.G. & Thomas, S.P., (1996). Anger in nurses: Don’t lose it. American Journal of Nursing. 96(4), 26-31. Fowler, A.R. Jr., Buschardt, S.C., Jones, M.A., (1993). Retaining nurses through conflict resolution. Health Progress. 74(5), 25-29. Frohling, H., (1996). Patient acuity and unit acuity. Nursing Management. 27(1). 10-11. Gabor, D., (1994). In speaking your mind in 101 difficult situations≅?…!=(pp.12-33). Huber, D.G., (1995). Hospital extra: Understanding the sources of stress for nurses. American Journal of Nursing. 95(12), 16J, 16N, 16P. Litwack, L., (1995). Practical points: Taking control: An approach to problem solving. Journal of Post Anesthesia Nursing. 10(3), 163-165. Lacono, B.J., & jacono, J.J., (1997). Worklife. Quick and easy stress relief techniques. Canadian-Nurse. 93(2), 49-50. Jalowiec, A., & Schaefer, K.M., (1993). The effectiveness of coping strategies in critical care nurses. Dimensions of Critical Care Nursing. 12(4), 204-205. Kenny, M.f., Gapas, J., & Hilton, G. (1995). Cross utilization in critical care. Nursing Management. 26(5), 48D, 48F-1. Laschinger, H.K., & Havens, D.S., (1996). Staff nurse work empowerment and a perceived control over Nursing practice: Conditions for work effectiveness. Journal of Nursing Administration. 26(9), 27-35. McDaniel, C., (1995). Organizational culture and ethics work satisfaction. Journal of Nursing Administration. 25 (11), 15-21. Moore, S., Kuhrik, M., Kuhrik, N., & Katz, B., (1996). Coping with downsizing: Stress, self-esteem, and social Intimacy. Nursing Management. 27(3), 28, 30. Page 8 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Peterman, B.A., Springer, P., Farnsworth, J., (1995). Analyzing job demands and coping techniques. Nursing Management. 26(2), 51-53. Salladay, S.A., (1998). Ethical problems. Dysfunctional workplace: Like a soap opera. Nursing. 28(5), 30. Seago, J.A., (1996). Work group culture, stress, and hostility: Correlations with organizational outcomes. Journal of Nursing Administration. 26(6), 39-47. Seago., J.A., & Faucett, J., (1997). Job strain among registered Nurses and other hospital workers. Journal of Nursing Administration. 27(5), 19-25. Page 9 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Title: Regional Hospital: Restraint/Seclusion Study Module for the Certified Nursing Assistant Purpose: This module delineates the use of restraints and seclusion including the philosophy, goals, and policy/procedure of the organization. Competency: Discusses elements of restraint and seclusion use. Objectives: Discuss organizational goals regarding restraint use. A. Discuss the myths vs. realities regarding restraints. B. Define restraint and seclusion. C. Review safety measures. D. Differentiate restraint from non-restraint, such as standard positioning, immobilization and adaptive devices. E. Discuss the effect of restraint use on the patient’s rights, dignity and well being. F. Identify preventive strategies and alternatives to restraint use. G. Discuss legitimate use of restraint. Content: A. B. C. D. E. F. G. H. I. Myth vs. Reality Restraint Policy and Procedure Definitions Side Effects and Restraint Use Preventive Strategy Alternatives to Restraint Acceptable Use of Restraint Conclusion References Required Activities: 1. Read and review the contents of this module to include the objectives required for your job description. (There is no final exam) 2. Read restraint Policy and Procedure. Approved by: Becky Finch RN Jodi Asche CNA Mary Vold RN BSN Beverly Nelson CNA Diane Vrieze RN Page 1 /CBO/NURSE ASSIST/HCMH/8/13/2004/ Introduction: Health care providers throughout the ages have routinely used physical restraints. Their use was usually not questioned, because restraints were viewed as protection for patients. The effectiveness of restraints began to be questioned in the late 1970’s (Reigle, 1997). Mandates from regulatory agencies, accreditation agencies and patient advocacy groups have compelled health care facilities to drastically reduce the use of restraints. Patients have the right to be free of restraint. The Restraint Task Force has led the effort to reduce restraint. This study module refers to the policy/procedure and standards for medical-surgical patients. Standards regarding use of restraint in behavioral health units are distinctly different from the ones discussed in this module. Content: A. Myth VS. Reality Nurses have historically used restraints for a variety of reasons such as to protect the patient from injury, to prevent the removal of medical equipment, or to prevent wandering behavior. By exploring and understanding some of the misconceptions regarding restraints, health care providers will seek alternative to their use. Myth: Reality: Restraints reduce the incidence of falls. There is evidence that restraints do not reduce the incidence of falls and that patients have less severe injuries if left unrestrained. A restraint will not prevent a patient form falling out of bed. In fact, the injury received if a patient falls when restrained may be more severe than if left unrestrained. There is no evidence that physical restraints safeguard patients from injury (Gilbert & Counsell, 1999). Myth: Reality: Restraints save money because the restrained patient requires less nursing time and attention. Patients in restraints require more attention to meet basic care needs and to assure their safety. The notion that restraints reduce the number of staff needed to care for patients is false. In fact, the opposite is true (Reigle, 1997). Restrained patients require more frequent visual observations. Because of the risks and safety issues associated with restraint use, you need to pay vigilant attention to ensure patient safety. A patient is unable to reach for a drink of water if his/her wrists are tied down. Consequently, you need to monitor more frequently to see that basic needs of fluid, elimination, and activity are met. Myth: Reality: Restraints control aggressive and combative behavior. Restraints can increase agitation, combativeness, and aggression. If you are angry, upset, and/or confused, would being tied down help calm you down? Applying restraints may remove the immediate threat, but does not solve problems in the long term (Reigle, 1997). Instead of immediately thinking of applying restraints, you should be asking yourself: “Why is this patient agitated?” “Was he started on a new medication that is having an adverse affect?” “Is he uncomfortable or in pain?” Page 2 /CBO/NURSE ASSIST/HCMH/8/13/2004/ B. Restraint Policy and Procedure: Refer to the facility’s policy and procedure regarding restraints. C. Definitions: • Restraint: • Any method of physically restricting a person’s freedom of movement, physical activity to his/her body. Seclusion: The involuntary confinement of person alone in a room where a person is physically prevented from leaving. What makes a device a restraint is the purpose or reason for its application. If a device is applied to restrict a person’s freedom of movement, activity, or normal access to his/her body, the device is a restraint. The following are not considered restraints: • Standard practices: 1. IV arm boards 2. Surgical positioning 3. Temporary immobilization related to procedures 4. Protection of surgical and treatment sites in neonatal or pediatric patients • Therapeutic holding/comforting of children • Adaptive support 1. Casts 2. Splints 3. Postural support If you place a cloth vest on a frail, elderly woman because she does not have enough upper body to hold herself upright in a wheel chair, the vest is not a restraint, but considered postural support as long as the vest does not restrict movement and can be easily removed by the patient. On the other hand, if the cloth vest is applied to prevent the patient from getting out of the wheelchair and wandering down the hallway, the vest is considered a restraint (Kobs, 1997). In this case, the standards apply of the use of the vest and a physician order has to be obtained and all the required documentation and patient monitoring must be done. The device used is not the issue, but the reason for its use is what defines whether or not the device is a restraint. The following are not considered restraints: • • Helmets to protect the head from injury Forensic and corrective restrictions used for security purposes The restraint policy does not apply to restraints used by police. If the police bring a patient to the Emergency Department in handcuffs, the police have applied the handcuffs for law enforcement purposes. On the other hand, if that same patient becomes confused and uncooperative and limb holders are applied to prevent him/her from pulling out the chest tube, the limb holders are considered restraints. Page 3 /CBO/NURSE ASSIST/HCMH/8/13/2004/ D. Side Effects of Restraint Use Restraint use can have adverse consequences on a patient’s physical and emotional well being. By understanding and thinking about these effects, you may taken them into account and reconsider restraint use. Physical consequences include all the adverse effects of immobility, including decubitis ulcers, skin tears, nerve injuries, and contractures. Restraints have been shown to cause injury resulting in higher mortality, longer hospital stays, and increased nosocomial infections (Ebersole & Hess, 1998). Negative outcomes arise from the safety issues related to restraint use and the fact that they are considered a high-risk procedure. Possible serious injuries associated with restraint use are broken bones, asphyxiation, strangulation, and death. Psychological consequences are the emotional effects of restraint use on the patient. Patient advocacy groups have interview patients who have been placed in restraints to find out what it felt like. Patients report how humiliated they felt when in restraints, the feeling of abandonment, and how embarrassed they were to have family walk in and be unable to cover themselves (Tideiksaar, 1998). Patients have also talked about fear for their safety while in restraints. Imagine the frightening feeling or worrying about what you would do if there was a fire and you are tied down and unable to move. This is why attention to protecting a patient’s rights, maintaining their dignity, and looking out for their physical well-being and safety, is essential when using restraints. E. F. Preventive Strategy The 3 keys to limiting the use of restraint are: 1. Do a thorough patient assessment. By assessing your patient’s physical health status and emotional/mental functioning, you can identify problems and initiate therapies, which could head off the use of restraints. Look at cultural/language barriers, which may lead to confusion or disruptive behavior. 2. Intervene with alternatives whenever possible. 3. Evaluate your treatment plans so the need for restraint doesn’t occur. Plan early to prevent the use of restraints. Has everything been tried to prevent the use of restraints? Alternative to Restraint The key to reducing restraint usage is the use of alternatives whenever possible. When thinking about alternatives, you need to be creative. The following are standard, effective alternatives. • • • • • • Consider adverse drug interactions/metabolic imbalance Reality orientation Decreased stimuli Use of PRN medication Room close to nurse’s station Repeated reassurances Page 4 /CBO/NURSE ASSIST/HCMH/8/13/2004/ • • • • • • Music therapy Ambulation/diversional activities Mattress on the floor (to prevent a fall) Constant observation (family/sitter/staff) Fall precautions (Fall Risk Assessment and Prevention Program) Cover or remove exposed lines or tubes The patient and family can play a significant role in limiting the use of restraints by offering suggestions alternatives. The patient and family’s preferences and suggestions should be considered in the patient’s plan of care. Some alternatives to restraints that the patient/family can offer are: • • • • Hobbies/interests of the patient Music preferences Aid in overcoming language/cultural barriers which could precipitate restraint use Bringing family photos/videos to calm and redirect the patient Family members may be willing to stay for longer periods of time to keep the patient safe and calm. They can offer you insight into music preferences, activities, and hobbies that interest the patient. G. Acceptable Use of Restraints Restraint use is justified when the safety of the patient or the safety of others is threatened. It is never acceptable or appropriate to use restraints as punishment, for staff convenience, discipline, or because the patient has a prior history of needing to be restrained. There are situations where restraint use is justified. The use has to be based on your assessment of the patient at that particular time. Restraint should only be used when all possible, viable alternatives have been evaluated, attempted, and failed. Close attention has to be paid to maintain a patient’s rights, dignity, and the meeting of their basic needs if you use a restraint. The least restrictive method of restraint should always be used. For example: Restraining one wrist is less restrictive than restraining both wrists. Soft limb holders are less restrictive than leather restraints. H. Conclusion By using alternative and basing restraint use on assessed patient needs, reducing the use of restraints is an attainable goal. It is essential to respect patient rights and meet their basic care needs if the use of restraint and seclusion is unavoidable. Increased knowledge of issues regarding restraint use by all disciplines will enhance our quality patient care and help achieve this goal. Page 5 /CBO/NURSE ASSIST/HCMH/8/13/2004/ I. References Ebersole, P., & Hess, P. (1998). Toward healthy aging. (5th ed.). St. Louis: Mosby. Gilbert, m., & Counsell, C. (1999). Planned s\change to implement a restraint reduction program. Journal of nursing care quality, 13 (5), 57-65\64. Kobs, A. (1998). Questions and answers from the JCAHO. Nursing management, 28 (1), 14-15. Reigle, J. (1997). Limiting the use of physical restrain. New guidelines present challenges. Critical Care nurse 17 (4) 80-85. Tideiksaar, R. (1998). Falls in older persons: Prevention and management. (pp. 125-137). Baltimore: Health Professions Press. Page 5 /CBO/NURSE ASSIST/HCMH/8/13/2004/