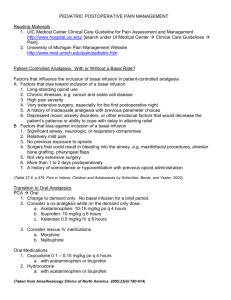
Pharmacy Newsletter – Pain Management Tables (6/02)1
advertisement

1
Brigham and Women’s / Dana Farber Guidelines for Opiate Administration / Pain Management Tables (2002)]
[references available from Faulkner Hospital Pharmacy ext. 7247]
Pain Management Tables (7/02)1
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Available Dosing Forms and Selected Comments
↓ - decreased incidence vs. other NSAIDs
↑ - increased incidence vs. other NSAIDs
Drug
Dosing Interval /
Maximum Daily Dose
Common Dosage
Forms (mg) #
Comments:
Acetaminophen
(Tylenol)
4-6 hours / 4000 mg
Less than 2 grams/day appears to be tolerated in patients with cirrhosis, monitor closely; essentially no anti-inflammatory
activity; low risk of GI side effects; no effect on platelets
(Included for comparison; no anti-inflammatory activity)
Aspirin
4-6 hours / 4000 mg
Tabs: 325, 500
Soln: 160 mg/5 mL
Supp: 120, 325, 650
Drops: 80 mg/ 0.8 mL
Tab: 81, 325
EC Tab: 81, 325
Supp: 300, 600
Celecoxib
(Celebrex)
Choline Magnesium
Trisalicylate
(Trilisate)
Ibuprofen
(Advil, Motrin)
12 hours / 400 mg
Tab: 100
↓ incidence of GI ulcerations; minimal to no inhibition of platelet function; cross allergy with sulfonamides
8-12 hours / 3000 mg
Tab: 750
(salicylate content)
↓ GI bleeding* vs. aspirin and perhaps vs. NSAIDs as a class, possibly due to minimal anti-platelet activity; use caution in
preexisting liver disease and avoid in severe liver disease
4-8 hours / 3200 mg
Tab: 200, 400, 600
Susp: 100 mg/5 mL
Indomethacin
(Indocin)
Ketorolac
(Toradol)
8-12 hours / 200 mg
Cap: 25, 50
Supp: 50 mg
Injectable:
- 15 mg/mL
- 30 mg/mL
Tab: 500, 750
Repeated studies have shown doses of 1500 mg/day or less to have the lowest risk of inducing serious GI complications among
non-salicylate NSAIDs; these studies did not include etodolac (Lodine—non-formulary) or nabumetone (Relafen); low risk of
inducing hepatotoxicity, but should be avoided in severe hepatic impairment; possible ↑ nephrotoxicity
High risk of nephrotoxicity vs. other NSAIDs; ↑ headache, tinnitus, dizziness, GI side effects; may aggravate depression or other
psychological disturbances secondary to CNS penetration
High incidence of headache; ↑ nephrotoxicity and GI complications; use no longer than 5 days; use 15 mg in patients greater than
65 years of age, less than 50 kg, or with renal impairment
6 hours / 120 mg
12-24 hours / 2000 mg
Nabumetone
(Relafen)
8-12 hours / 1500 mg
Tab: 250, 375
Naproxen
(Naprosyn)
4-6 hours / 400 mg
Cap: 50
Meclofenamate
(Meclomen)
24 hours / 25 mg chronic
Tab: 12.5
Rofecoxib
50 mg acute (5 days)
(Vioxx)
8-12 hours / 3000 mg
Tab: 500
Salsalate
(Disalcid)
# Supp = suppository; Susp = suspension; EC = enteric coated; Soln = oral solution
High risk of GI bleeding; use caution in preexisting liver disease and avoid in severe liver disease; least potent inhibitor of renal
prostaglandins
↓ GI bleeding* and side effects; reduce dose in hepatic dysfunction. Daily to twice daily dosing.
↑ hepatotoxicity (↓ dose 50% in hepatic disease) and possible nephrotoxicity; high tissue penetration; potent inhibitor of
leukocyte function; pregnancy category B (1st and 2nd trimester only)
High incidence of diarrhea, ↑ GI side effects; do not use for more than 1 continuous week
↓ incidence of GI ulcerations; minimal to no inhibition of platelet function
See choline magnesium trisalicylate
* Limited data versus COX 2 inhibitors
NSAID Selection*
Situation or Patient Population
Consider
Generally Avoid
GI Bleed, history of
Hepatic dysfunction, current
Hepatic dysfunction, high risk
Lactation
Peptic Ulcer
Renal dysfunction, current
Renal dysfunction, pts at risk for
Thrombocytopenia
Warfarin, concurrent use
Acetaminophen, celecoxib, ibuprofen, nabumetone, rofecoxib, non-acetylated salicylates**
Acetaminophen (reduced doses)
Ibuprofen
Acetaminophen, ibuprofen, ketorolac, naproxen
Acetaminophen, celecoxib, rofecoxib, non-acetylated salicylates**
Acetaminophen (reduced doses)
Aspirin, non-acetylated salicylates**
Acetaminophen, rofecoxib, celecoxib, non-acetylated salicylates**
Acetaminophen, rofecoxib, celecoxib, non-acetylated salicylates**
Aspirin, indomethacin, ketorolac, meclofenamate
Aspirin, ibuprofen
Naproxen
Aspirin, non-acetylated salicylates**
Aspirin, indomethacin, ketorolac, meclofenamate
Aspirin, choline magnesium trisalicylate, indomethacin
Ibuprofen, indomethacin, naproxen
All other agents inhibit platelet function and prolong bleeding time to some degree
All other agents inhibit platelet function and prolong bleeding time to some degree
* Only formulary items are listed
** non-acetylated salicylates include salicylate salts (choline magnesium trisalicylate) and salsalate
Equianalgesic Opioid Dose Chart and Available Formulations***
Drug
Morphine
(MSIR, MS Contin*)
IV / IM
10
Equianalgesic Doses (mg)
Oral
30 (chronic)
Available Strengths
and Dosage Forms
Tab: 15 mg
CR* Tabs: 15, 30, 60 mg
Soln: 10 mg/5 mL
Suppository: 10 mg
Injectable
Tab: 2 mg
Injectable
Tab: 5 mg
CR* Tab: 10, 20 mg
Soln: 5 mg/5 mL
Hydromorphone
(Dilaudid)
Oxycodone
(Roxicodone, OxyContin*)
1.5
7.5
N/A
20
Hydrocodone
Codeine
N/A
130
30
200
Fentanyl
(Sublimaze,
Duragesic patch)
Meperidine
(Demerol)
0.1
(100 mcg)
N/A
Tab: 15, 30 mg
Injectable
Transdermal Patch:
25, 50, 75, 100 mcg/hour
Injectable
75
300
Tab: 50 mg
Injectable
10 to 20 acute
2 to 4 chronic
Tab: 5, 10 mg
Soln: 5 mg/5 mL
Methadone
5 to 10 acute
(Dolophine)
1 to 2 chronic
Tramadol **
(Ultram)
* CR = Controlled release; Soln = oral solution
Tab: 50 mg
Comments
Caution: Do NOT confuse with Morphine.
Caution: Each Percocet 5 mg/325 mg contains 5 mg Oxycodone and 325 mg Acetaminophen.
Percocet should be ordered as 5 mg/325 mg tablets (only strength on formulary).
Caution: Each Vicodin tablet contains 5 mg Hydrocodone and 500 mg Acetaminophen.
Doses greater than 60 mg not recommended. Increased nausea and constipation.
Transdermal patch 25 mcg/hour is equianalgesic to approximately 50 mg of oral morphine per day.
Not recommended for pain management.
CNS excitation from metabolite accumulation.
Dose MAX = 600 mg/day; limit to 48 hours.
Long half life; accumulates with repeated dosing; may require dose decrease on days 2 to 5
Ceiling dose 400 mg/day (300 mg/day for elderly).
50 mg of tramadol is equianalgesic to approximately 60 mg of oral codeine.
**Not an opioid; binds to opiate receptors
***These are NOT suggested starting doses; these are doses of opioids that produce approximately the same
Equianalgesic Conversion Example:
amount of analgesia. Published trials vary in the suggested doses that are equianalgesic to morphine. By using
the Equianalgesic Opioid Dose Chart, you can determine a dose of a new (“NEW”) opioid and/or route of
administration that is approximately equal in analgesic effect to the dose of the former (“OLD”). Titration to
clinical response is necessary. Recommended doses do not apply to patients with renal or hepatic insufficiency
or other conditions affecting drug metabolism and kinetics. Elderly patients generally require lower doses,
titrated slowly to the desired effect or intolerable side effects. (reference: www.med.umich.edu/PAIN/APAINMGT)
Patient takes OxyContin 20 mg po Q 12 hours and Percocet (5 mg/325 mg) 1 tablet po Q 3 to 4 hours PRN.
Only 1 Percocet (5 mg/325 mg) has been required for breakthrough pain every day. Convert to continuous IV infusion of morphine.
[{OxyContin 20 mg = oxycodone 20 mg CR} and {Percocet (5 mg/325 mg) = oxycodone 5 mg and acetaminophen 325 mg}]
****Incomplete cross-tolerance: Some studies and written clinical impressions suggest that during high-dose
chronic treatment with one strong opioid, patients become somewhat tolerant to that drug but remain relatively
sensitive to different opioids. This is one reason to consider reducing the dose of the NEW drug by 25% to 50%.
(reference: Principles of Analgesic Use in the Treatment of Acute Pain and Cancer Pain; 4th Edition; 1999)
STEP I → DAILY OPIOID REQUIREMENT: Calculate patient’s total daily opioid requirement
(NOTE – if taking different opioids, need to convert each to one common opioid)
-- Total daily dose of oxycodone from OxyContin 20 mg → 20 mg x 2 doses → 40 mg
-- Total daily dose of oxycodone from 1 Percocet (5 mg/325 mg) → 5 mg
→ 40 mg oxycodone + 5 mg oxycodone → 45 mg oxycodone/day
STEP II → OLD to NEW: Convert the daily requirement of the old opioid to that of the new opioid.
EQUIANALGESIC DOSE CONVERSION FORMULA: ***
EXAMPLE:
Opiate Allergy: True allergic reactions to opioids are rare (i.e., IgE involvement). Symptoms are usually
secondary to mast cell activation and subsequent histamine release. Selection of another opioid class is usually
necessary only if patient has had a true allergic reaction and not simply a sensitivity to histamine release.
class (chemical structure)
diphenylheptanes
phenanthrenes
phenylpiperidines
opiates
methadone, propoxyphene
codeine, hydrocodone, hydromorphone, morphine,
oxycodone, levorphanol (non-formulary)
fentanyl, meperidine, sufentanil (non-formulary)
Equianalgesic Dose for OLD (Chart) = 24-hour dose of OLD (total)
Equianalgesic Dose for NEW (Chart)
(x) 24-hour dose of NEW
20 mg po oxycodone
10 mg IV morphine
=
45 mg po oxycodone
(x) mg IV morphine
→ (x) = 22.5 mg IV morphine/day (i.e., 22.5 mg IV morphine/day is equianalgesic to 45 mg po oxycodone/day)
STEP III → INCOMPLETE CROSS TOLERANCE: ****
Consider incomplete cross tolerance and decrease total daily opiate dose by 25% to 50% → 11.25 mg to 16.9 mg
STEP IV → NEW DRUG DOSE:
→ 11.25 mg to 16.9 mg/day divided by 24 hours/day → 0.45 mg to 0.7 mg of morphine per hour.