Pain Management Detailing Handout
advertisement

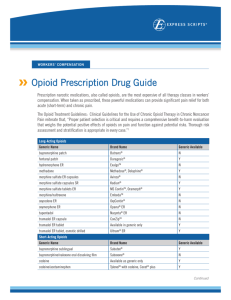
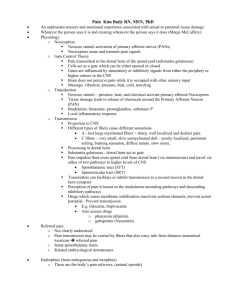
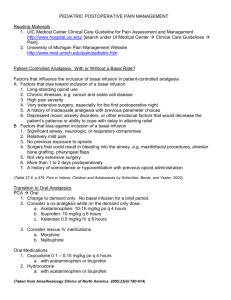
Aging Q3 Pain Management ACOVE Pain-related problems are present in 25% - 50% of community-dwelling elderly people. Pharmacological treatment with analgesics for pain is the most common in the elderly, however, the use of alternative medications and non-pharmacological interventions should also be considered. Treatment decisions require continuous weighing of risks and benefits. (Etzioni, et al. JAGS 2007 55:S403-S408) Mechanisms of Chronic Pain Nociceptive Neuropathic Peripheral sensitization (hyperalgesia, allodynia) Central sensitization (NMDA) Desensitization (tolerance) Disinhibition (GABA) WHO Ladder Level 3 (severe pain): strong opioids – morphine, hydromorphone, fentanyl, oxycodone +/- adjuvants Level 2 (moderate to severe pain): acetaminophen plus opioid (hydrocodone, codeine, oxycodone); tramadol +/adjuvants Level 1 (mild to moderate pain): acetaminophen, aspirin, NSAIDS (cox-2) +/adjuvants Opioid Side Effects Nausea and vomiting (central) Delayed gastric emptying Constipation Hypotension Myoclonus Respiratory depression CNS GU Pruritus Non-opioid Treatment Options (Adjuvants) for Pain in the Elderly Drug Acetaminophen Anticonvulsants Antidepressants Local Anesthetics NSAIDS Tramadol Muscle Relaxants Description Comments/Side Effects First-line agent for patients with OA and patients with mild to moderate pain. Primarily in neuropathic pain (carbamazepine divalproex, gabapentin, pregabalin, topiramate, duloxetine) Limit dose in elderly. Avoid combining with opioids. TCAs, SNRIs Start low dose,increase slowly: Anticholinergic side effects of TCAs BP effects of SNRIs Lidocaine: may apply up to 3 patches q 12 hours Capsaicin: burning pain intolerable by some patients. Cox-2 probably OK. Avoid combining with opioids Lidocaine patches Capsaicin Avoid in elderly if possible (AGS) Start low dose, increase slowly Cyclobenzaprine, carisoprodol Avoid in elderly if possible (AGS) Carbamazepine: blood dyscrasias,Gabapentin/Pregabalin: Ataxia, dizziness, somnolence Drowsiness, nausea, constipation May not be best option for patients on antidepressants Anticholinergic side effects, arrhythmias EQUIANALGESIC DOSES OF OPIOID ANALGESICS USED FOR THE CONTROL OF PAINa Oral (PO) Dose (mg) Analgesicb Intravenous (IV Dose (mg) 50 150 Meperidine (Demerol)c – (do not use in elderly) 100 Codeine (Tylenol with Codeine)c,d 15 Hydrocodone (Vicodin, Lortab, Zydone, Norco, Vicoprofen) c,e - 15 MORPHINE (MSIR, Roxanol, MS Contin, Kadian, Avinza)f 5 Oxycodone (Percodan, Percocet, Endocet, Roxicodone, OxyIR, OxyContin, OxyFAST, OxyDose)g - 10 10 Methadone (Dolophine)h - (very difficult to use in elderly) 5 4 Hydromorphone (Dilaudid)f 2 - Levorphanol (Levo-Dromoran) Fentanyl (Duragesic/Actiq)i 60 1.5 h 1 - i Duragesic fentanyl transdermal system: mcg/h patch q 3 days=mg morphine PO q12th. Actiq: 1 unit buccally over 15 minutes pm breakthrough pain. Opioid treatment of chronic pain should be initiated in opioid-naïve patients with a short acting opioid (e.g. oxycodone) and converted to a long-acting opioid (e.g. fentanyl patches) when the desired analgesic effect is achieved. a Equianalgesic doses listed were obtained from a variety of studies and experiences and are meant only as guidelines b Dose interval: q4h, except for: meperidine=q2-3h, levorphanol=q4=6h, methadone=q6-12h. MS Contin=q8-12h, Kadian=q12-24h, Avinza=q24h, OxyContin=q12h, Duragesic=q48-72h. c Not recommended for severe pain – neurotoxic with repeated dosing. d Tylenol #2=15mg codeine, Tylenol #3=30 mg codeine, Tylenol #4=60mg codeine. All contain 325 mg acetaminophen. e Combination tablets contain 2.5-10 mg hydrocodone plus 325-750 mg acetaminophen or 200 mg ibuprofen. f Rectal suppositories available. Per rectum (P.R.) dose is equal to PO dose. g Combination tablets contain 2.5-10 mg oxycodone+325-650 mg acetaminophen or 325 mg aspirin. h Caution: Risk of toxicity from delayed accumulation. In opioid rotation, start methadone at 25-50% of equianalgesic dose calculated from table FCCC PMC 3/23/0 Funding provided by D.W. Reynolds Foundation UIM chronic opioid management policy (complies with Board of Medicine recommendations) Patients on chronic opioid therapy pain must be assessed every three months and complete a “Patient Agreement” annually and the patient agrees: That opioids are part of an overall pain management plan and patients must adhere to other recommendations such as physical therapy, use of pharmacologic adjuncts etc. Opioids will be written by UIM only and acquired from one pharmacy Prescriptions will NOT be re-written or written early under any circumstances Not use illegal substances and agree to random urine drug screens Patient will not sell or give opioids to others Violation of agreement for chronic pain management will result in dismissal from the UIM practice