Lecture 4
Pawel Doloto
pawel@creighton.edu
August 28, 2003 Psychological Dimensions
I heard the word on the street is that some of the M1 girls are pretty good looking, I don’t know cause I’ve been studying for the ID quiz so I haven’t had a chance to look. Then I heard a lot of them were single.
THEN I got a suggestion from a female M2 girl (whose name rhymes with ary hussy) that I should divulge some of my sweet-talking secrets to the rest of the single guys in our class, so that they can have a potent arsenal of pick up lines to approach the single M1 ladies.
All of the pick up lines are in italics throughout the note service, if you are easily offended don’t read them.
Also, try them at your own risk. Good luck!
#1(With hands on shoulders) Oh, those are shoulder blades, I thought they were wings.
Physician as Change Agent
Behavioral Change in a patient can sometimes take a long time; other times, all it takes for a successful intervention is one comment/observation to make the patient realize that they want to change.
Main Points today:
•
Review our MD patient/physician relationship skills and behaviors
•
•
Present the four principles guiding communication with patients
Go over skills required to bring about change in an ambivalent or resistant patient
•
Go over cases, which will show incorporation of the above skills in a time-limited patient setting
Most of the cases, we’ll face will be very straightforward, e.g. “doctor, fix my broken finger.” But in some cases the diagnosis may not be as clear, we will need the our communication skills to solve the case, or when the patient is resisting treatment or change the good relationship we have with him/her will help us treat them.
There are four general principles to guide Physician communication w/ the patient:
I. Building relationship
1.
Early MD behaviors: greet by name, make eye contact, shake hands, smile, eye level, small talk, use humor, avoid “why” questions, do not ask multiple questions (give a patient a chance to answer), be careful of misleading or biased questions.
Try to avoid medical jargon, statement of false reassurance, or defensive statements. It is also very important to have actions and words be consistent with each other. Check
Cole/Bird Book (whatever that is) chapters 25/26 for more examples of things to do and avoid.
#2 If you need a love doctor, I have like a medicated degree…
2.
Enhancing Social Power (things that make others look up to you):
•
Credibility- credentials, reputation (like graduating from Creighton, YEY!),
Diplomas, attire, organized, attentive
•
Trustworthiness (probably the most important aspect)- warm, understanding, some self-disclosure, good follow through, nonverbal communication is more important than verbal to build trust, without trust you won’t get very far
•
Attractiveness, similar attitudes, physical attractiveness, again nonverbal communication- nodding, smiling, eye contact
Read over Slide 3.1 to know what kind of traps you can fall into during 1 st
session, but we don’t need to know.
3.
Early Stage Strategies-
•
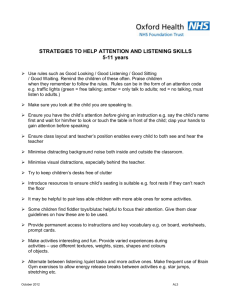
Open-Ended Questions- whenever starting a new subject area w/ a patient, ask open ended questions, remember to listen to the patient, they should be doing most of the talking even 10-15mins of mostly listening will make you look caring.
•
Active Listening- be able to acknowledge what the patient is saying, sometimes paraphrase it or clarify what patient is talking about. Don’t just sit in a room with a patient. Be able to transition from one area to another (e.g. from weather smalltalk to severe strep A infection), or use reflective listening.
#3 Sure, I’ll help you study Anatomy…
Don’t say, “Sure, I’ll help you study infectious disease…”
•
Page 4, Slide 1, Roadblocks to Active listening, look it over, e.g. if you’re ordering directing, or commanding, warning or threatening then you are not really actively listening.
•
Active (reflective) listening- essentially it is guessing what the patient is saying.
There are 3 steps in communication: coding, hearing, decoding, and breakdown could happen anywhere. MD makes a guess at the meaning of what the patient said and reflects (tells the patient) what that guess was in a form of a statement.
Reflective listening is an active process of checking that patient & MD are talking about the same thing. It is important in following open-ended questions.
•
Affirmation or Validation- essentially MD communicates to the patient that patient’s behavior is understandable within the context of patient’s life (e.g. MD says ”I understand how you can see drinking as a way out of stress in your life”).
Don’t have to agree w/ the behavior, just acknowledge that they’re trying to deal with things in their life (even if their efforts are misguided). Acknowledge the feeling of the patient. Try to point out whether patient’s response to dealing w/ issues is appropriate/reasonable or not (e.g. drinking not the best way to deal w/ stress). Make sure that your verbal and non-verbal expression match (so don’t roll your eyes at your patients Brewer).
Amount of validation needed will change from case to case; some, more private issues or withdrawn patients may require more time & validation, others less. If the MD is overanxious to make patient feel better may lead to invalidation patient’s feeling (e.g. wouldn’t spend 30min of feeling validation for a hangnail). The MD should convey to the patient that their feelings are understandable but furthermore that the patient can live with them (it sucks that you’re sick, but you can deal with it; here’s what you can do)
#4 You may not be really hot, but I bet you like to do it…
•
Summarization- good way to link material, reinforce what has been said, show you’ve been listening, clarify things, transition, end or begin conversation, fill silence when you’re lost & can help the patient hear their own ambivalence to things.
Slide on 5.3 gives examples of summarizing.
•
You must be able to deal w/ Different levels of patient motivation: 1) straightforward-real easy 2) Ambivalent 3) Complete Resistance
•
MD must understand ambivalence as something normal & understandable, not as a sign of poor motivation. Forcing the issue w/ the patient may lead to resistance, while pointing out the pros and cons of the situation may lead to cooperation by patient.
•
Slide 6.3, some examples of why people would be ambivalent about change (two good options, two crappy options, view of change varies from day to day, torn
between 2 options). Sometimes, people won’t want to change until their circumstances change, like they have a child so just keep on reminding the pt.
#5 I'm not trying anything, I always put my hands there.
II. Orchestrate Discrepancy-
1.
Make the patient aware of consequences of not changing (overweight= heart problems,
Diabetes). You can also point out the differences between the patient’s goals & their behavior. The arguments for change should come from the patient; the MD is the one who makes the patient put these arguments forth.
2.
Slide 7.3 shows a figure of phases of change (client= patient, counselor=MD).
It is MD’s job to go into patient’s world, understand them, and then drag them out into the healthy lifestyle through introduction of incongruence b/n patient’s goals and their being, which can be used as motivation by the patient.
3.
It is important to build a relationship with the patient, but MDs need other strategies to get them to change, to resolve their ambivalence. MDs need to get patient to come up with arguments for change, see what part of change the patient’s willing to do. Remember confrontation may lead to resistance, but getting patient to cooperate may lead to success.
(Dr. Guck says if you act like Colombo (sp?) then you will evoke your patients’ proper response?”
#6 If you were a tear in my eye I would not cry for fear of losing you.
4.
Slides 8.1 & 8.2 are examples of questions to ask patient:
•
Problem Recognition: e.g. what things make you think this is a problem? (if they do not recognize the problem, you can’t help them)
•
Concern: e.g. How much/ In what way does this concern you? (if it doesn’t concern them, they probably won’t change)
•
Intention to Change: e.g. what makes you think you need to change? (find out their motivation so you don’t have to wrestle with them to change, but assist them with it)
•
Optimism: e.g. what encourages you that you can make a change if you want to?
(How can I the MD help you?)
III. Roll with Resistance- 4 categories of resistance (If the patient exhibits these behaviors you know that the patient is resisting.):
1.
Arguing: The patient contests the accuracy, expertise or integrity of the MD (by challenging, discounting, or being hostile).
2.
Interrupting: Patient breaks in and interrupts MD in a defensive manner (e.g. talking over or cutting off).
3.
Denying: Patient expresses an unwillingness to recognize problems, cooperate, accept responsibility or take action (e.g. they try to blame, disagree, excuse, claim impunity, minimize, they show pessimism or reluctance).
4.
Ignoring: Patient does not follow MD recommendations (e.g. inattention, non-answer, no response, sidetracking). This is common in teenagers, so be ready during your first interview with a teen.
#7 If I could rearrange the alphabet, I'd put U and I together.
5.
In order to deal with resistance, you want to avoid arguing for change, it won’t help, change strategy! Do not directly oppose resistance. You can invite new perspectives (that
can lead to change), but you can’t impose them. So, don’t get down on yourself if your patient, for example, doesn’t want to stop smoking. It doesn’t mean you’re a bad doctor.
It’s up to the patient to want to make a change, you’re just there to support them. Get your answers and solutions from the patient (e.g. are they willing to cut down smoking, or do they even feel the need to stop?). If someone is resisting, it means you have to try a different strategy.
8. Stand still so I can pick you up!
IV. Support Self-Efficacy
1.
defined as the belief in one’s ability to perform a specific behavior; it includes beliefs in one’s capabilities and optimism about being successful in behavior change efforts. So a patient may be ready to stop a behavior, but they may not feel up to it. Here’s where you can make the difference, (e.g. “you can do it!”)
2.
All efforts to express empathy, develop discrepancy, avoid argumentation, and roll with resistance may be ineffective if patient does not believe that he/she can change. So, all the skills discussed up to now are useless unless you can get your patient to believe in him/her self. You got to be a positive influence.
So, what do you do when someone comes in and says “I failed, I got drunk with my buddies last weekend”
Answer from the 2 people in lecture: “You’re stupid!”
Answer from Dr. Guck: Reaffirm the patient, tell them it was a good effort, focus on the good, re-establish their belief that they can do it.
3.
It is important that the MD makes statements and asks questions that promote the patient’s
HOPE that change is possible. Remember, you are the agent of change that has to implement this.
Systems that you can use to put into your 5-10minutes of interview with the patient:
I. National Cancer Institute’s 5 A’s (can be found in chptr #9 in our 20 Problems Book):
1.
Ask about motivation for change
2.
Assess for motivation for change
3.
Advise the patient
4.
Assist the patient
5.
Arrange Follow-up
6.
Judith Ockene’s Model
II. Judith Ockene’s Model
1.
Assess Desire and Motivation to Change
2.
Examine Past Experiences with Behavior Change (what worked and what didn’t work for the patient in the past)
3.
Ask about Barriers to Change (what makes change hard)
4.
Ask about resources for change (who/what can help you)
5.
Plan for Change and Follow up (what can we do this week, what about next week)
FRAMES- Active in gradients in effective brief interventions: F eedback, R esponsibility, A dvice, M enu,
E mpathy, and S elf-Efficacy
Summery: Dance with Patients, don’t wrestle with them.
#9 this one’s for you MCS: “Hey...somebody farted. Let's get out of here.”
For those of you that have not yet found a behavioral change project I recommend watching Troy
McClure’s Self-Improvement Video Series:
“Paint chips, Delicious but deadly,”
“Smoke yourself thin,” and “Get confidence, stupid!”