Alteplase Treatment of Acute Pulmonary Embolism
advertisement

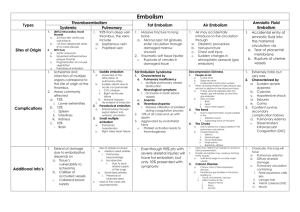
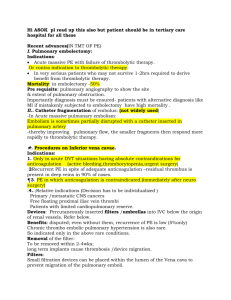
Cover Alteplase Treatment of Acute Pulmonary Embolism in the Intensive Care Unit PAMELA L. SMITHBURGER, PharmD, BCPS SHAUNA CAMPBELL, MSN SANDRA L. KANE-GILL, MS, PharmD, MSC Acute pulmonary embolism accounts for 50 000 to 100 000 deaths each year in the United States. Because of the wide spectrum of clinical manifestations, ranging from massive pulmonary embolism to small peripheral emboli, stratifying and treating patients according to their signs and symptoms is important when an acute embolism is suspected. Patients’ clinical findings can range from no signs or symptoms to unstable hemodynamic status and shock. The 3-month mortality is 10% to 15%, but can be as high as 60% in patients with hemodynamic shock. This article reviews the classifications of acute peripheral emboli, explains the treatment of acute peripheral emboli, reviews the pharmacology of alteplase, and presents an assessment of the literature evaluating alteplase for the treatment of acute peripheral emboli. Clinical pearls for the administration, monitoring, and care of a patient receiving alteplase in an intensive care unit also are discussed. (Critical Care Nurse. 2013;33[2]:17-27) A cute pulmonary embolism is a deadly event that occurs in 1 per 1000 persons and is responsible for 50 000 to 100 000 deaths each year in the United States.1-3 A pulmonary embolism is an obstruction of the pulmonary artery or one of its branches by a thrombus. The signs and symptoms range from massive pulmonary embolism that results in unstable hemodynamic status to a small peripheral embolus that can be asymptomatic. To aid in the delineation of the types of pulmonary embolism, the American Heart Association has proposed several definitions4 (Table 1). These definitions have been used in clinical trials and practice guidelines to help stratify patients and aid in treatment selection. Approximately 44% of patients who have pulmonary embolism have a confirmed deep vein thrombosis.5 The pathogenesis of venous thromboembolism can be explained on the basis of the Virchow triad6: stasis, endothelial injury, and hypercoagulability. Table 2 provides risk factors for pulmonary embolism.7-12 CNE Continuing Nursing Education This article has been designated for CNE credit. A closed-book, multiple-choice examination follows this article, which tests your knowledge of the following objectives: 1. Identify signs and symptoms when acute embolism is suspected 2. Discuss the medical management of acute peripheral emboli 3. Differentiate the classifications of acute peripheral emboli ©2013 American Association of Critical-Care Nurses doi: http://dx.doi.org/10.4037/ccn2013626 www.ccnonline.org CriticalCareNurse Vol 33, No. 2, APRIL 2013 17 Table 1 Definitions of an acute pulmonary embolisma Category Description Massive Acute pulmonary embolism with Sustained hypotension (systolic blood pressure <90 mm Hg for at least 15 min) Requirement for inotropic support, not because of other causes Persistent or pulseless, bradycardia (heart rate <40/min) with shock Submassive Acute pulmonary embolism with myocardial necrosis or right ventricular dysfunction but no systemic hypotension Low risk Acute pulmonary embolism with normal levels of biomarkers, no systemic hypotension or right ventricular dysfunction a Based on information from Jaff et al.4 Table 2 Selected risk factors for thromboembolisma Component of the Virchow triad Risk factor Stasis Immobilization Paralysis Atrial fibrillation Long-distance travel Venous insufficiency Endothelial injury Recent central venous instrumentation Hypertension Atherosclerosis Trauma or surgery Indwelling catheter Hypercoagulability Malignant neoplasms History of heavy smoking Pregnancy Obesity Estrogen therapy Sepsis Trauma or surgery of a lower extremity a Based on information from Stein et al,7 PIOPED Investigators,8 Darze et al,9 Heit et al,10 Green et al,11 and Goldhaber et al.12 Thrombi from the iliofemoral vein are the most commonly involved source of pulmonary embolism.13,14 After traveling to the lungs, large thrombi often lodge in the bifurcation of the main pulmonary artery or the lobar branches, obstructing perfusion in the artery or its branches. The thrombus causes a blockage in the lung, resulting in an increase in pulmonary pressure, which increases the resistance to blood flow in the right ventricle. The result is increased right ventricular workload and decreased perfusion to the lung. If the right ventricle cannot pump against the increased pressure, right-sided heart failure can occur, which is manifested as hypoxemia, hypotension, and shortness of breath.15 Impaired gas exchange is also commonly associated with pulmonary embolism. The impairment is not solely due to the mechanical obstruction of the vasculature. Numbers of neutrophils and levels of platelet-activating factor are increased, and functional intrapulmonary shunting (area in the lung where perfusion exceeds ventilation), atelectasis, and surfactant dysfunction may occur, which can contribute to impaired gas exchange.16 In the United States, acute pulmonary embolism is the third leading cause of death in hospitalized patients.17 Unfortunately, the manifestations of an acute pulmonary embolism can be highly variable and nonspecific, ranging from no signs or symptoms to unstable hemodynamic status and shock. Patients with acute pulmonary embolism can have a wide range of signs and symptoms, including dyspnea at rest or with exertion (73%), sharp chest pain that may radiate to the shoulder (44%), calf or thigh pain (44%), calf or thigh swelling (41%), cough (34%), 2+ pillow orthopnea (28%), and wheezing (21%). Clinical manifestations of a deep vein thrombosis are apparent in 44% of patients.15,18 Approximately 8% of patients experience circulatory collapse, and among these patients, dyspnea Authors Pamela L. Smithburger is an assistant professor of pharmacy and therapeutics, University of Pittsburgh, School of Pharmacy, and a critical care clinical specialist in the medical ICU, University of Pittsburgh Medical Center Presbyterian Hospital, Pittsburgh, Pennsylvania. Shauna Campbell is the director of the medical ICU, University of Pittsburgh Medical Center. Sandra L. Kane-Gill is an associate professor of pharmacy and therapeutics, Center for Pharmacoinformatics and Outcomes Research, University of Pittsburgh, School of Pharmacy, and a critical care patient safety officer, Department of Pharmacy, University of Pittsburgh Medical Center. Corresponding author: Pamela Smithburger, PharmD, BCPS, University of Pittsburgh School of Pharmacy, University of Pittsburgh Medical Center, 200 Lothrop St, Pittsburgh PA 15213 (e-mail: smithburgerpl@upmc.edu). To purchase electronic or print reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail, reprints@aacn.org. 18 CriticalCareNurse Vol 33, No. 2, APRIL 2013 www.ccnonline.org has been reported in 82% and dyspnea or tachypnea in 92%.18 In adults, the rate of asymptomatic acute pulmonary embolisms ranges from 28% to 58%.11 In addition to signs and symptoms, the gold standard for diagnosis of a pulmonary embolism is pulmonary angiography.19 This study is performed by injecting contrast material into a branch of the pulmonary artery. Normal findings on pulmonary angiograms exclude a diagnosis of pulmonary embolism. Pulmonary angiography and computed tomography of the lungs can reveal pulmonary abnormalities that may explain a patient’s signs and symptoms. According to Wolf et al,19 66% to 93% of pulmonary embolisms can be detected by using computed tomography or pulmonary angiography. A D-dimer test can aid in the diagnosis of pulmonary embolism. D-dimers are specific degradation products of cross-linked fibrin. In patients with an acute clot, the serum level of D-dimer is elevated because of the simultaneous increase in coagulation and fibrinolysis.20 The D-dimer level has a high negative predictive value for venous thromboembolism and pulmonary embolism and therefore can be used to rule out these conditions.2 However, the test has poor specificity and a low positive predictive value. Therefore, other means of diagnosing pulmonary embolism are necessary.20 Clinical outcomes of pulmonary embolism vary greatly depending on patients’ characteristics and the type of pulmonary embolism. The estimated 3-month mortality rate after diagnosis is 10% to 15%.21 However, 5% to 10% of patients with pulmonary embolism have an unstable hemodynamic status and shock and compared with patients without these characteristics have a higher mortality rate of almost 60%.9,12 Therefore, stratifying patients on the basis of their clinical signs and symptoms when pulmonary embolism is suspected is important. Acute Pulmonary Embolism Initial Treatment Treatment of pulmonary embolism includes both initial stabilization and anticoagulation, with consideration given to the use of a thrombolytic agent. In patients with suspected pulmonary embolism, stabilization of hemodynamic status should be the primary focus.3,4 Patients with hypoxemia should be given supplemental oxygen. For patients with hypotension, fluid boluses are used initially to replace fluids; vasopressors are given if fluid replacement is inadequate. Anticoagulation is the www.ccnonline.org mainstay of treatment for patients with a high probability of pulmonary embolism. Patients with objectively confirmed pulmonary embolism or strongly suspected pulmonary embolism and no contraindications should receive anticoagulation therapy with low-molecularweight heparin, subcutaneous fondaparinux, or intravenous unfractionated heparin.3,4 Anticoagulants, such as heparin, prevent the thrombus that is already formed from increasing in size. These medications cannot decrease the size of a thrombus that has already formed, but they can be used to stop clot growth and the development of new clots.21 Although anticoagulants prevent both growth of established thrombus and formation of new thrombus, thrombolytics actually decrease the size of the already formed thrombus by dissolving fibrin. The 2011 guidelines of the American Heart Association4 and the guidelines of the American In addition to signs and symptoms, the College of gold standard for diagnosis of a pulmonary Chest Physi- embolism is pulmonary angiography. cians3 recommend that patients with massive pulmonary embolism, evidence of hemodynamic compromise, and acceptable bleeding risk receive a thrombolytic. Use of a thrombolytic not only accelerates the lysis of the thrombus in acute pulmonary embolisms but also improves physiological parameters such as pulmonary perfusion and right ventricular function via dissolution of the thrombus. Alteplase Alteplase initiates local fibrinolysis by binding to the fibrin in a clot and converting the trapped plasminogen to plasmin.22 The result is dissolution of the thrombus.22,23 When alteplase is administered, more than 50% of the drug concentration in the plasma is cleared within 5 minutes after the infusion is stopped. Alteplase is primarily cleared hepatically.23 The Food and Drug Administration (FDA) has approved this thrombolytic agent for management of ST-elevation myocardial infarction (lysis of thrombi in coronary arteries), acute stroke, and acute pulmonary embolism.23 Alteplase was approved for management of acute pulmonary embolism in 2002, and it can be used for management of acute, massive pulmonary embolism in adults for the lysis of acute pulmonary emboli accompanied by unstable hemodynamic status, such as hypotension.23 CriticalCareNurse Vol 33, No. 2, APRIL 2013 19 Contraindications and Interactions. Patients treated with alteplase should be evaluated; bleeding, especially at the catheter puncture site; and hemorrhages, including gastrointestinal, intracranial, and retroperitoneal hemorrhages should be considered.4 Most of the absolute and relative contraindications for use of alteplase (Table 3) are characteristics that would predispose a patient to a bleeding event.23 Clinicians should also be mindful of possible drug interactions. Concurrent administration of alteplase with an anticoagulant, such as heparin and vitamin K antagonists, or other medications that alter platelet function, such as aspirin and clopidogrel, may increase the risk of bleeding if administered before, during, or after alteplase therapy. The length of time the bleeding risk is increased depends on the agent used in addition to alteplase and can range from 1 hour for heparin to up to 5 days for clopidogrel.3,4 Therefore, patients given these combinations of drugs should be carefully monitored if the drugs are administered together.3,4,23 Use With Heparin. The FDA-approved regimen of alteplase for an acute, massive pulmonary embolism is 100 mg administered by intravenous infusion over 2 hours.22 Heparin therapy should be stopped during the alteplase infusion and reinstituted after the infusion when the activated partial thromboplastin time (aPTT) or thrombin time returns to twice normal or less.23-27 With thrombolysis, patients may have an increased risk for bleeding. However, in a comparison of the bleeding rates after the administration of alteplase in patients who received heparin only and patients who received alteplase plus heparin, the rates of bleeding in the 2 groups did not differ significantly.24-30 Overall, compared with heparin alone, alteplase decreased total peripheral resistance and ventricular dilatation and increased cardiac output, ejection fraction, and oxygen saturation.24,26,28 Table 4 reviews the grading criteria for clinical trials. Table 5—available online only at www.ccnonline.org— summarizes clinical trials on the use of alteplase in patients with massive pulmonary embolism. Treatment of Submassive Pulmonary Embolism Thrombolysis should be considered for patients with submassive pulmonary embolism if they have a poor prognosis and a low risk for bleeding.4 The guidelines3 of the American College of Chest Physicians recommend 20 CriticalCareNurse Vol 33, No. 2, APRIL 2013 Table 3 Contraindications to use of alteplasea Absolute contraindications Relative contraindications Internal bleeding Previous intracranial hemorrhage History of a cerebral vascular accident within the past 3 months Recent intracranial or intraspinal surgery or trauma Intracranial neoplasm Arteriovenous malformation or aneurysm Known bleeding diathesis a Based Age >75 y Current use of anticoagulation Pregnancy Noncompressible vascular punctures Traumatic or prolonged cardiopulmonary resuscitation (<10 min) Recent internal bleeding (within 2-4 wk) History of chronic, severe, and poorly controlled hypertension Severe uncontrolled hypertension on initial examination (systolic blood pressure >180 mm Hg or diastolic blood pressure >110 mm Hg) Dementia Remote ischemic stroke (>3 mo) Major surgery within preceding 3 weeks on information from Jaff et al4 and Ouellette and Patocka.22 the use of thrombolytic agents in these patients. Administration of a thrombolytic agent in addition to heparin requires assessment of a patient’s characteristics and of the risks and benefits of thrombolytic use, such as right ventricular strain and predisposition for bleeding. Of note, use of alteplase for treatment of submassive pulmonary embolism has not been approved by the FDA and is a widely debated topic. In patients with acute right ventricular dysfunction, use of alteplase can result in a 2- to 3-fold increase in death due to the embolism.33 Among patients with submassive pulmonary embolism, those who received heparin plus alteplase had less deterioration in clinical status, shorter hospital stays, an increase in pulmonary perfusion, shorter time to improved right ventricular function, and lower hospital mortality than Table 4 Grading criteria for clinical trialsa Assessment Grade Grade description Risk vs benefit 1 2 Benefit > risk Risk > benefit Quality of the data available A B C Good Fair Poor a Based on information from Ansani et al.31 www.ccnonline.org did those who received heparin alone.34-36 In addition, primary PE is diagnosed thrombolysis with alteplase and treatment is necessary decreased the need for treatment escalation, such as emergently administering a thrombolytic after Massive PE Submassive PE Low-risk PE heparin therapy alone was unsuccessful.35 Differences in bleeding between patients who received RV strain or a possibility Hemodynamic compromise No RV strain heparin alone and patients who of poor prognosis (SBP <90 mm Hg received heparin plus alteplase were for >15 minutes or need inotropic support) not significant.34-36 Table 6—available online only at www.ccnonline.org— summarizes the use of alteplase in patients with submassive pulAnticoagulation Anticoagulation Anticoagulation monary embolism. The Figure is a proposed treatment algorithm based on a patient’s risk of bleeding Consider thrombolytic agents if: and severity of the pulmonary 1. Patient has shock or respiratory distress 2. RV dysfunction embolism as reflected by hemody3. Elevated levels of biomarkers (troponin, BNP) 3,4 namic compromise. In systemic thrombolytic therapy, the drug is given through a peripheral intravenous catheter. When sysLow or acceptable bleeding risk and no contraindications to thrombolytic therapy temic thrombolytic therapy is contraindicated because of increased risk for bleeding or insufficient time for systemic thrombolysis, other 1. Discontinue heparin infusion 2. Administer alteplase 100 mg IV for 2 hours therapies, such as catheter-directed 3. Check aPTT thrombolysis (CDT), may be neces4. Restart heparin infusion when aPTT ≤2 times normal sary.3,39,40 In CDT, the thrombolytic agent is administered directly into the pulmonary artery via a pulFigure Treatment algorithm for acute pulmonary embolism. Based on information from Kearon et al3 and Jaff et al.4 monary artery catheter23; the usual Abbreviations: aPTT, activated partial thromboplastin time; BNP, brain natriuretic peptide; IV, intravenous; thrombolytic agent is full-dose PE, pulmonary embolism; RV, right ventricle; SBP, systolic blood pressure. heparin. Table 7 is a summary of the clinical trials and assessments of the mechanical thrombectomy, which can involve either efficacy of CDT with alteplase.31,39,41-46 Overall, CDT spinning wires or jets of physiological saline aimed at the appears safe and effective. With CDT, medications can thrombus, to increase the rate of dissolution.47 Currently, be delivered directly to the thrombus at a high concenCDT with alteplase is an “off-label” use of the drug. When tration. Lower doses of a thrombolytic and shorter duraused in CDT, alteplase has been infused at 0.5 to 1 mg/h tions of infusions are used to achieve complete for up to 48 hours.39 No clinical trials have been done to thrombolysis. In theory, compared with systemic thromcompare systemic thrombolysis with CDT. In a review of bolysis, the use of lower doses and shorter infusions several methods of catheter-directed approaches with or times with alteplase reduces the risk of bleeding compli3,40,41 without local or systemic thrombolytic therapy in patients cations. Thrombolytic methods have also been comwith acute massive pulmonary embolism, Kuo et al39 bined with mechanical methods such as percutaneous www.ccnonline.org CriticalCareNurse Vol 33, No. 2, APRIL 2013 21 Table 7 Summary of clinical trials and assessments of the efficacy of catheter-directed thrombolysis (CDT) in patients with pulmonary embolism (PE) Study Study design n Type of PE Treatment Chamsuddin et al, 2008 RE 10 Acute massive Catheter-directed infusion of urokinase 60 000 IU in 12 hours, then 90 000 IU/h (n = 1); alteplase mean dose 0.88 mg/h (n = 8); reteplase 0.5 mg/h then 0.25 mg/hr (n = 1) Mean infusion time was 24.76 hours Kuo et al,39 2009 RE 594 Acute massive, treated with modern CDT Modern CDT included low-profile devices; mechanical fragmentation and/or aspiration of emboli, including rheolytic thrombectomy, and intraclot thrombolytic injection if a local drug was infused Griffith et al,43 2009 CR 1 Massive Catheter-directed infusion of alteplase 1 mg/h + VA-ECMO + inhaled nitric oxide 20 ppm + mechanical thrombolysis Bechtel et al,44 2005 CR 1 Massive bilateral Catheter-directed alteplase initial infusion of 12 mg followed by an infusion of 0.7 mg/h Lin et al,45 2009 RE 25 Massive Catheter-directed alteplase at dose 0.93 mg/h for a mean total dose of 25.43 mg (range 16-45 mg) Mean duration of the infusion was 26.7 hours (range 14-46 hours) vs catheter-directed therapy + EkoSonic Endovascular System Kuo et al,46 2008 RE 12 Massive Among the 12 patients, 7 received CDT thombolysis: 5 received alteplase (mean dose 20 mg) and 2 received tenecteplase (mean dose 12 mg) with catheter-directed fragmentation and suction embolectomy 41 Abbreviations: CR, case report; RE, retrospective; VA-ECMO, venoarterial extracorporeal membrane oxygenation. a Grading is based on criteria of the Agency for Healthcare Research and Quality.31 Table 8 Guideline recommendations for the use of thrombolytic agents to treat massive and submassive pulmonary embolism (PE) and in catheter-directed thrombolysis (CDT) Guideline Massive PE Gradea IIA,B Gradea Submassive PE American Heart Association4 The use of thrombolytic agents is reasonable for patients with massive acute PE and an acceptable risk for bleeding complications The use of thrombolytics may be considered for patients with submassive PE judged to have clinical evidence of adverse prognosis (new unstable hemodynamic status, worsening respiratory insufficiency, severe right ventricular dysfunction, or major myocardial necrosis) and low risk for bleeding complications American College of Chest Physicians3 For patients with evidence of hemodynamic compromise, use of thrombolytic therapy is recommended unless patient has major contraindications because of risk for bleeding 1B In selected high-risk patients without hypotension who are judged to have a low risk for bleeding, administration of thrombolytic therapy is suggested 2B European Society of Cardiology48 Thrombolytic therapy is the first-line treatment in patients with high-risk PE presenting with cardiogenic shock and/or persistent arterial hypotension, with very few absolute contraindications. NA Routine use of thrombolysis in patients not at high risk for bleeding is not recommended, but may be considered in selected patients with intermediate-risk PE and after thorough consideration of conditions increasing the risk for bleeding NA Abbreviations: NA, not applicable; VA-ECMO, venoarterial extracorporeal membrane oxygenation. a Grading is based on criteria of the Agency for Healthcare Research and Quality.31 22 CriticalCareNurse Vol 33, No. 2, APRIL 2013 www.ccnonline.org IIB,C Results Gradea Lysis of thrombus was 69%, with a mean lysis time of 23.4 hours The treatment group had no major hemorrhagic events 1B In 60% to 67% of patients, a local thrombolytic agent was infused during the mechanical maneuvers The pooled success rate was 86.5% (95% CI, 82.2%-90.2%; q = 60.3, P = .004 for heterogeneity; I 2 = 40.3%) 1C VA-ECMO was stopped and patient was extubated 1C Patient recovered completely and was discharged taking enoxaparin 1 mg/kg twice a day 1C EkoSonic Endovascular System treatment was a success compared with the CDT group (P < .02) The alteplase dosage and infusion time were lower in the EkoSonic group than in the CDT group (P < .001). 1B Mean systolic pulmonary pressure improved from 57.6 to 44 mm Hg (P < .05); shock index improved (<0.9) in 83% of patients Clinical success was achieved in 83% of patients 1C reported that clinical success was achieved in 71% to 100% of patients who underwent a catheter-directed embolectomy with either systemic or local thrombolysis. In patients who underwent catheter-directed embolectomy alone, the success rate was 67% to 88%. Therefore, local experience with CDT and the expertise of the physician performing the procedure should be taken into account when CDT is being considered for a patient. Use of Alteplase in Patients With Acute Pulmonary Embolism CDT Gradea Direct intra-arterial delivery of thrombolytics, such as alteplase 0.6 mg/kg (up to 50 mg), over 15 minutes, may be helpful when mechanical thrombectomy strategies are ineffective NA Infusion of alteplase directly into a pulmonary artery rather than via a peripheral vein does not accelerate thrombolysis but does cause more frequent bleeding at the catheter insertion site When a lytic agent is appropriate for PE, thrombolytic agents should be infused into a peripheral vein over 2 hours or less NA Direct local infusion of tissue plasminogen activator via a catheter in the pulmonary artery (at a reduced dosage) did not have any advantages over systemic intravenous thrombolysis This approach should generally be avoided, because it is associated with an increased risk for bleeding at the puncture site NA Table 8 provides a summary of the recommendations of the American Heart Association,4 the American College of Chest Physicians,3 and the European Society of Cardiology48 for use of a thrombolytic agent in patients with massive pulmonary embolism or submassive pulmonary embolism and in CDT. For patients with massive pulmonary embolism, all 3 guidelines recommend use of a thrombolytic agent when the patients have no risk for bleeding. In patients with submassive pulmonary embolism, the 3 guidelines recommend use of thrombolytic agents in patients at high risk for death who have a low risk for bleeding. Neither the American College of Chest Physicians nor the European Society of Cardiology recommends the use of CDT. The American Heart Association suggests that CDT may be helpful when other mechanical thrombectomy strategies are unsuccessful. Currently, 3 meta-analyses49-51 (Table 9) have been conducted to evaluate thrombolysis for the treatment of pulmonary embolism. Agnelli et al49 found a lower composite end point of death and recurrence of embolism with thrombolysis than with heparin therapy alone. Wan et al50 reported a possible benefit for the use of thrombolysis in patients with unstable hemodynamic status and the highest risk for death or recurrence of embolism. Therefore, these authors50 recommend use of a thrombolytic agent in patients with a major pulmonary embolism and hemodynamic compromise. Dong et al51 did not find any benefit of thrombolysis or any difference in hemorrhagic events between control and interventional groups. They concluded that evidence of any benefit from the use of thrombolytic agents rather than heparin in the treatment of acute pulmonary embolism is insufficient. Bedside Nursing Management Patients receiving alteplase for the treatment of acute pulmonary embolism require specific nursing monitoring www.ccnonline.org CriticalCareNurse Vol 33, No. 2, APRIL 2013 23 Table 9 Summary of 3 meta-analyses on the use of thrombolysis for the treatment of pulmonary embolism (PE) Study No. Type of PE Treatments Results Any A total of 241 patients (52.3%) received thrombolytic therapy with streptokinase (n = 31), urokinase (n = 102 ), or alteplase (n = 108) A total of 220 patients received heparin A total of 11 deaths (4.6%) occurred in the thrombolysis group and 17 deaths (7.7%) occurred in the heparin group (RR, 0.59; 95% CI, 0.27-1.25) Five fatal bleeding episodes (2.1%) occurred in the thrombolysis group; none occurred in the heparin group Agnelli et al,49 2002 461 patients, 9 clinical trials Wan et al,50 2004 748 patients, 11 trials Acute Dong et al,51 2006 679 patients, 8 trials Confirmed Patients in the included trials Thrombolytic therapy resulted in a nonsignificant were randomized to receive a reduction in recurrent PE or death (6.7% vs 9.6%; systemic thrombolytic agent, OR, 0.67, 95% CI, 0.40-1.12, P for heterogeneincluding urokinase, streptokiity = .48), a nonsignificant increase in major nase, alteplase, or heparin bleeding (9.1% vs 6.1%; OR, 1.42; 95% CI, 0.81-2.46), and a significant increase in nonmajor bleeding (22.7% vs 10.0%; OR, 2.63; 95% CI, 1.53-4.54) When a thrombolytic agent was used in patients with unstable hemodynamic status, a reduction in recurrent PE or death occurred (9.4% vs 19.0%; OR, 0.45; 95% CI, 0.22-0.92) Patients were included in trials Results were similar between the heparin and that used a thrombolytic, includthrombolytic groups for the following: death ing streptokinase, urokinase, (OR, 0.89; 95% CI, 0.45-1.78), PE recurrence recombinant tissue plasmino(OR, 0.63; 95% CI, 0.33-1.20), major hemorgen activator, and alteplase rhagic events (OR, 1.61; 95% CI, 0.91-2.86), Results were compared with minor hemorrhagic events (OR, 1.98; 95% CI, those of patients who had 0.68-5.75) heparin alone or placebo or surgical intervention Abbreviations: OR, odds ratio; RR, relative risk. and care. Because of the high risk for bleeding, these patients should be cared for in a critical care setting for at least 24 hours, depending on their clinical status.50 Close monitoring for bleeding and hypertension are required during this time. Alteplase should be diluted with sterile water to a final concentration of 1 mg/mL for injection.22 The manufacturer provides a transfer device that should be used to add the sterile water to the alteplase powder. Foaming may occur when the sterile water is added but will dissipate if the mixture is allowed to stand undisturbed for Patients should be monitored closely several minutes. Of note, for bleeding and hypertension in a critical care setting for at least 24 alteplase hours after administration of alteplase should not be because of the high risk for bleeding. shaken during dilution and mixing. In order to thoroughly mix the medication, the vial should be gently swirled or inverted. Alteplase is stable at room temperature for 8 hours after it is 24 CriticalCareNurse Vol 33, No. 2, APRIL 2013 reconstituted and contains no antibacterial preservatives. For these reasons, the drug should be reconstituted immediately before use and should be administered within 8 hours of dilution.26 In most patients, a continuous heparin infusion will already have been started while the decision to use alteplase is being made or while the alteplase is being dispensed by the pharmacy. In these patients, in order to decrease the risk for bleeding, the heparin infusion should be stopped when the alteplase infusion is started. Alteplase should be administered as a continuous infusion over a 2-hour period. During the infusion, patients’ neurological status should be monitored frequently because of the increased risk for cerebral hemorrhage. Neurological checks should be completed every 15 minutes during administration of the drug, then every 30 minutes for 6 hours, and then hourly for 24 hours after initiation of treatment.3,4,52 Alert patients should be instructed to report any changes in headache, vision, and sensorium. Any change in neurological status is reason to discontinue the infusion to investigate the www.ccnonline.org possibility of intracranial bleeding,22 and computed tomography of the head should be conducted immediately. Bleeding remains a risk for up to 36 hours after completion of the alteplase infusion.4 Heart rate and blood pressure should be monitored continually, because these physiological indicators could alert bedside nurses to the occurrence of bleeding.22,52 Monitoring of heart rate and blood pressure is recommended for 24 hours after the administration of alteplase. Upon completion of the alteplase infusion, continuous infusion of heparin should be reinitiated. Before the infusion is restarted, blood should be obtained for determination of aPTT. In order to reduce the risk for bleeding, the heparin should not be started until the aPTT is twice the normal level or less.23 As the heparin infusion is restarted, monitoring for signs and symptoms of bleeding should continue. The aPTT should be monitored per institutional protocol to ensure the attainment of therapeutic anticoagulation and to prevent overanticoagulation. Other important nursing considerations include refraining from venous or arterial punctures and placement of invasive tubes during the first 24 hours after administration of alteplase.50 Existing insertion sites of invasive catheters should be assessed hourly for bleeding. At times, alteplase may be administered via a CDT method. In these situations, a smaller dose of alteplase (0.5-1 mg/h) is infused into the pulmonary artery via a pulmonary artery catheter for an extended time (14-46 hours).39,41-46 As with systemic administration of alteplase, bedside nurses should monitor patients for any signs or symptoms of bleeding. Specific attention should be paid to the insertion site of the pulmonary catheter.43 The efficacy of alteplase can be monitored by noting the resolution of signs and symptoms related to the pulmonary embolism. For example, a patient should begin to have improvement in hemodynamic parameters, including blood pressure, heart rate, and right end-diastolic function. Improvement in the patient’s subjective symptoms should also occur, such as less chest pain, shortness of breath, and wheezing or cough.23 Summary Acute pulmonary embolisms are life-threatening abnormalities with a wide range of signs and symptoms. Because of the wide spectrum, from no signs or symptoms to hypotension and shock, diagnosis can be difficult. Early diagnosis and treatment are necessary to provide www.ccnonline.org the best care and improve patients’ outcomes.53 Alteplase is efficacious in the treatment of acute massive and submassive pulmonary embolisms, although it has not been approved by the FDA for treatment of submassive pulmonary embolism. The risk for and development of bleeding should always be taken into account when therapy is started. CCN Financial Disclosures None reported. Now that you’ve read the article, create or contribute to an online discussion about this topic using eLetters. Just visit www.ccnonline.org and click “Submit a response” in either the full-text or PDF view of the article. To learn more about caring for patients with pulmonary embolism, read “Massive Pulmonary Embolism” by Shaughnessy in Critical Care Nurse, February 2007;27(1):39-50. Available at www.ccnonline.org. References 1. Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States, 1979-1998: an analysis using multiple-cause mortality data. Arch Intern Med. 2003;163(14):1711-1717. 2. Burge AJ, Freeman KD, Klapper PJ, Haramati LB. Increased diagnosis of pulmonary embolism without a corresponding decline in mortality during the CT era. Clin Radiol. 2008;63(4):381-386. 3. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ; American College of Chest Physicians. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133(6 suppl):454S-545S. 4. Jaff MR, McMurtry S, Archer SL, et al; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; American Heart Association Council on Peripheral Vascular Disease; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association [published correction appears in Circulation. 2012;125(11):e495]. Circulation. 2011;123(16):1788-1830. 5. Meignan M, Rosso J, Gauthier H, et al. Systematic lung scans reveal a high frequency of silent pulmonary embolism in patients with proximal deep venous thrombosis. Arch Intern Med. 2000;160(2):159-165. 6. Dickson BC. Venous thrombosis: on the history of Virchow’s triad. Univ Toronto Med J. 2004;81:166-171. 7. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007; 120(10):871-879. 8. PIOPED Investigators. Value of the ventilation/perfusion scan in acute pulmonary embolism: results of the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED). JAMA. 1990;263(20):2753-2759. 9. Darze ES, Latado AL, Guimarães AG, et al. Incidence and clinical predictors of pulmonary embolism in severe heart failure patients admitted to a coronary care unit. Chest. 2005;128(4):2576-2580. 10. Heit JA, O’Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med. 2002;162(11):1245-1248. 11. Green RM, Meyer TJ, Dunn M, Glassroth J. Pulmonary embolism in younger adults. Chest. 1992;101(6):1507-1511. 12. Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999;353(9162):1386-1389. 13. Galanaud JP, Sevestre-Pietri MA, Bosson JL, et al; OPTIMEV-SFMV Investigators. Comparative study on risk factors and early outcome of CriticalCareNurse Vol 33, No. 2, APRIL 2013 25 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 26 symptomatic distal versus proximal deep vein thrombosis: results from the OPTIMEV study. Thromb Haemost. 2009;102(3):493-500. Girard P, Decousus M, Laporte S, et al; PREPIC Study Group. Diagnosis of pulmonary embolism in patients with proximal deep vein thrombosis: specificity of symptoms and perfusion defects at baseline and during anticoagulant therapy. Am J Respir Crit Care Med. 2001;164(6): 1033-1037. Moheimani F, Jackson DE. Venous thromboembolism: classification, risk factors, diagnosis, and management . ISRN Hematol. 2011;2011:124610. doi:10.5402/2011/124610. Jorens PG, Van Marck E, Snoeckx A, Parizel PM. Nonthrombotic pulmonary embolism. Eur Respir J. 2009;34(2):452-474. Goldhaber SZ, Elliott CG. Acute pulmonary embolism, I: epidemiology, pathophysiology, and diagnosis. Circulation. 2003;108(22):2726-2729. Stein PD, Beemath A, Matta F. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879. Wolf SJ, McCubbin TR, Nordenholz KE, Naviaux NW, Haukoos JS. Assessment of the pulmonary embolism rule-out criteria rule for evaluation of suspected pulmonary embolism in the emergency department. Am J Emerg Med. 2008;26(2)181-185. Wang Y, Liu ZH, Zhang HL, Luo Q, Zhao ZH, Zhao Q. Predicative value of D-dimer test for recurrent venous thromboembolism at hospital discharge in patients with acute pulmonary embolism. J Thromb Thrombolysis. 2011;32(4):410-416. Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States, 1979-1998: an analysis using multiple-cause data. Arch Intern Med. 2003;163:1711-1717. Ouellette DW, Patocka C. Pulmonary embolism. Emerg Med Clin North Am. 2012;30(2):329-375. Activase [package insert]. South San Francisco, CA: Genentech Inc;2011. Meneveau N, Schiele F, Vuillemenot A, et al. Streptokinase vs alteplase in massive pulmonary embolism: a randomized trial assessing right heart haemodynamics and pulmonary vascular obstruction. Eur Heart J. 1997; 18(7):1141-1148. Meneveau N, Schiele F, Metz D, et al. Comparative efficacy of a two-hour regimen of streptokinase versus alteplase in acute massive pulmonary embolism: immediate clinical and hemodynamic outcome and one-year follow-up. J Am Coll Cardiol. 1998;31(5):1057-1063. Konstantinides S, Tiede N, Geibel A, et al. Comparison of alteplase versus heparin for resolution of major pulmonary embolism. Am J Cardiol. 1998; 82:966-970. Wang C, Zhai Z, Yang Y, et al; China Venous Thromboembolism (VTE) study group. Efficacy and safety of low dose recombinant tissue-type plasminogen activator for the treatment of acute pulmonary embolism: a randomized, multicenter, controlled trial. Chest. 2010;137(2):254-262. Sors H, Pacouret G, Azarian R, Meyer G, Charbonnier B, Simonneau G. Hemodynamic effects of bolus vs 2-h infusion of alteplase in acute massive pulmonary embolism: a randomized controlled multicenter trial. Chest. 1994;106(3):712-717. Dalla-Volta S, Palla A, Santolicandro A, et al. PAIMS 2: alteplase combined with heparin versus heparin in the treatment of acute pulmonary, embolism. Plasminogen Activator Italian Multicenter Study 2. J Am Coll Cardiol. 1992;20(3):520-526. PIOPED Investigators. Tissue plasminogen activator for the treatment of acute pulmonary embolism. Chest. 1990;97:528-533. Ansani NT, Fedutes-Henderson BA, Skledar SJ, et al. Practical approach to grading evidence for formulary recommendations. Am J Health Syst Pharm. 2005;62:1498-1501. Le Conte P, Huchet L, Trewick D, et al. Efficacy of alteplase thrombolysis for ED treatment of pulmonary embolism with shock. Am J Emerg Med. 2003;21(5):438-440. Kucher N, Rossi E, De Rosa M, et al. Prognostic role of echocardiography among patients with acute pulmonary embolism and a systolic arterial pressure of 90 mm Hg or higher. Arch Intern Med. 2005;165:1777-1781. Berghaus TM, Thilo C, Bluethgen A, et al. Effectiveness of thrombolysis in patients with intermediate-risk pulmonary embolism: influence in length of hospital stay. Adv Ther. 2010;27(9):648-654. Konstantinides S, Geibel A, Heusel G, Heinrich F, Kasper W; Management Strategies and Prognosis of Pulmonary Embolism-3 Trial investigators. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med. 2002;347(15):1143-1150. Fasullo S, Scalzo S, Maringhini G, et al. Six-month echocardiographic study in patients with submassive pulmonary embolism and right ventricle dysfunction: comparison of thrombolysis with heparin. Am J Med Sci. 2011;341(1):33-39. CriticalCareNurse Vol 33, No. 2, APRIL 2013 37. Goldhaber SZ, Agnelli G, Levine MN. Reduced dose bolus alteplase vs conventional alteplase infusion for pulmonary embolism thrombolysis: an international multicenter randomized trial. The Bolus Alteplase Pulmonary Embolism Group. Chest. 1994;106(3):718-724. 38. Goldhaber SZ, Haire WD, Feldstein ML, et al. Alteplase versus heparin in acute pulmonary embolism: randomized trial assessing right-ventricular function and pulmonary perfusion. Lancet. 1993;341(8844):507-511. 39. Kuo WT, Gould MK, Louie JD, Rosenberg JK, Sze DY, Hofmann LV. Catheter-directed therapy for the treatment of massive pulmonary embolism: systemic review and meta-analysis of modern techniques. J Vasc Interv Radiol. 2009;20(11):1431-1440. 40. Krichavsky MZ, Rybicki FJ, Resnic FS. Catheter directed lysis and thrombectomy of submassive pulmonary embolism. Catheter Cardiovasc Interv. 2011;77(1):144-147. 41. Chamsuddin A, Nazzal L, Kanf B, et al. Catheter-directed thrombolysis with the endowave system in the treatment of acute massive pulmonary embolism: a retrospective multicenter case series. J Vasc Interv Radiol. 2008;19:372-376. 42. Skaf E, Beemath A, Siddiqui T, et al. Catherter-tip embolectomy in the management of acute massive pulmonary embolism. Am J Cardiol. 2007; 99:415-420. 43. Griffith KE, Jenkins E, Haft J. Treatment of massive pulmonary embolism utilizing a multidisciplinary approach. Perfusion. 2009;24:169-172. 44. Bechtel JJ, Mountford MC, Ellinwood WE. Massive pulmonary embolism in pregnancy treated with catheter fragmentation and local thrombolysis. Obstet Gynecol. 2005;106:1158-1160. 45. Lin PH, Annambhotla S, Bechara CF, et al. Comparison of percutaneous ultrasound-accelerated thrombolysis versus catheter-directed thrombolysis in patients with acute massive pulmonary embolism [published correction appears in Vascular. 2010;18(1):62]. Vascular. 2009;17(suppl 3):S137-S147. 46. Kuo WT, van den Bosch MAAJ, Hofmann LV, et al. Catheter-directed embolectomy, fragmentation, and thrombolysis for the treatment of massive pulmonary embolism after failure of systemic thrombolysis. Chest. 2008;134:250-254. 47. Hubbard J, Saad WEA, Sabri SS, et al. Rheolytic thrombectomy with or without adjunctive indwelling pharmacolysis in patients presenting with acute pulmonary embolism presenting with right heart strain and/or pulseless electrical activity. Thrombosis. 2011;2011:246410. 48. Torbicki A, Perrier A, Konstantinides S, et al; ESC Committee for Practice Guidelines (CPG). Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008;29(18):2276-2315. 49. Agnelli G, Becattini C, Kirschstein T. Thrombolysis vs heparin in the treatment of pulmonary embolism. Arch Intern Med. 2002;162:2537-2541. 50. Wan S, Quinlan DJ, Agnelli G, Eikelboom JW. Thrombolysis compared with heparin for the initial treatment of pulmonary embolism. Circulation. 2004;110:744-749. 51. Dong BR, Hao Q, Yue J, Wu T, Liu GJ. Thrombolytic therapy for pulmonary embolism. Cochrane Database Syst Rev. 2009;(3):CD004437. doi:10.1002/14651858. CD004437.pub3. 52. Vance D L. Treating acute ischemic stroke with intravenous alteplase. Crit Care Nurse. 2001;21(4):25-32. 53. Piazza G, Goldhaber SZ. Acute pulmonary embolism, I: epidemiology and diagnosis. Circulation. 2006;114:e28-e32. www.ccnonline.org