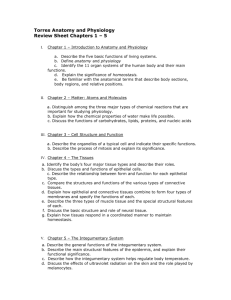
Lecture Exam One Material: Anatomy and Physiology 121
advertisement

Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System Introduction to the Human Body ¾ ¾ ¾ ¾ ¾ ¾ ¾ Anatomy and physiology are absolutely interrelated subjects in which structures at all levels are defined and also used to understand the dynamic function of a living organism. Specialized systems within the body support each others operation so that complex responses are possible to a myriad of changing environmental conditions. Anatomy Defined: Through a study of anatomy and its subdivisions, the body may be examined at different levels of structural organization. Anatomy may be defined as the study of structure and the relationships among structures. Physiology Defined: Physiology deals with how body parts operate; the structure of a part often determines its function. Physiology is the study of how body structures function. Subdivisions of Physiology: Include cell physiology, systems physiology, pathophysiology, exercise physiology, neurophysiology, endocrinology, cardiovascular physiology, immunophysiology, respiratory physiology, renal physiology, and reproductive physiology. Levels Of Structural Organization: ¾ The human body consists of several levels of structural organization. ¾ Human Body Systems: The systems of the human body are the integumentary, skeletal, muscular, nervous, endocrine, cardiovascular, lymphatic, respiratory, digestive, urinary, and reproductive. ¾ ¾ Life Processes: All living things have certain characteristics that distinguish them from nonliving things. Among the life processes in humans are metabolism, responsiveness, movement, growth, differentiation, and reproduction. ¾ ¾ Life Processes: All living things have certain characteristics that distinguish them from nonliving things. Among the life processes in humans are metabolism, responsiveness, movement, growth, differentiation, and reproduction. Homeostasis: Maintaining Physiological Limits: Basic Principles of Homeostasis : ¾ Homeostasis is a condition in which the body's internal environment remains within certain physiological limits. ¾ For the body's cells to survive, the composition of the surrounding fluids must be maintained precisely at all times. ¾ Since ECF is in constant motion throughout the body and also surrounds all body cells, it is often called the body's internal environment. ¾ ¾ ¾ ¾ ¾ Basic Principles: Homeostasis An organism is said to be in homeostasis when its internal environment: Contains the optimum concentration of0 gases, nutrients, ions, and water; Has an optimal temperature; Has an optimal volume for the health of the cells. The maintenance of homeostasis results in health; physiological imbalance may result in disease 1 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System or death. ¾ ¾ Stress and Homeostasis: Stress is any external or internal stimulus that creates an imbalance in the internal environment. If a stress acts on the body, homeostatic mechanisms attempt to counteract the effects of the stress and bring the condition back to normal. Feedback Systems (Loops): ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ ¾ A feedback system (loop) is a cycle of events in which information about the status of a condition is continually monitored and fed back (reported) to a central control region (Fig. 1.3). Any stress that changes a controlled condition is called a stimulus. Regulation of Homeostasis by Nervous and Endocrine Systems Homeostasis is regulated by the nervous system and endocrine systems, acting together or independently. The nervous system detects body changes and sends nerve impulses to counteract the stress. The endocrine system regulates homeostasis by secreting hormones. Whereas nerve impulses cause rapid changes, hormones usually work more slowly. Feedback Systems: Components A feedback system consists of three basic components. The control center determines the point at which a controlled condition should be maintained. The receptor monitors changes in the controlled condition and then sends the information, called the input, to the control center. The effector receives information, called the output, from the control center and produces a response (effect). Feedback Systems: Types If a response reverses the original stimulus, the system is a negative feedback system (loop). If a response enhances the original stimulus, the system is a positive feedback system (loop). Homeostasis of Blood Pressure (BP): Example of (-) Feedback Loop If a stimulus (stress) causes blood pressure (controlled condition) to rise, pressure sensitive nerve cells (receptors) in certain arteries send impulses (input) to the brain (control center). The brain sends impulses (output) to the heart (effector), causing the heart rate to decrease (response) and the return of blood pressure to normal (restoration of homeostasis). Homeostasis of Labor Contractions Example of (+) Feedback: When labor begins, the uterus is stretched (stimulus) and stretch-sensitive nerve cells in the cervix of the uterus (receptors) send nerve impulses (input) to the hypothalamus (control center). ¾ The hypothalamus causes the release of oxytocin (output) which stimulates the uterus (effector) to contract more forcefully (response). ¾ ¾ ¾ ¾ ¾ What is Disease? Disease is a state of homeostatic imbalance Disruptions of homeostasis can lead to disease and death. Disease is any change from a state of health, characterized by symptoms and signs. Diagnosis is the art of distinguishing one disease from another or determining the nature of a 2 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System ¾ ¾ ¾ ¾ ¾ ¾ ¾ disease; a diagnosis is generally arrived at after the taking of a medical history and the administration of a physical examination. Anatomical Terminology: Anatomical Position: The anatomical position is a standardized method of observing or imagining the body that allows precise and consistent anatomical references. When in the anatomical position, the subject stands erect facing the observer, the upper extremities are placed at the sides, the palms of the hands are turned forward, and the feet are flat on the floor. Planes and Sections: Planes are imaginary flat surfaces that are used to divide the body or organs into definite areas Principal planes include: midsagittal (median) and parasagittal, frontal (coronal), transverse (cross-sectional or horizontal), and oblique. Body Cavities: Spaces in the body that contain internal organs are called cavities; these cavities may be separated by structures such as muscles, bones, or ligaments. The two principal body cavities are the dorsal and ventral cavities . ¾ The Thoracic Cavity: The thoracic cavity contains two pleural cavities, and the mediastinum, which includes the pericardial cavity. ¾ ¾ Abdominopelvic Cavity: The abdominopelvic cavity is divided into a superior abdominal and an inferior pelvic cavity. To describe the location of organs easily, the abdominopelvic cavity may be divided into nine regions by drawing four imaginary lines ¾ Abdominopelvic Cavity: To locate the site of an abdominopelvic abnormality in clinical studies, the abdominopelvic cavity may be divided into quadrants by passing imaginary horizontal and vertical lines through the umbilicus . Medical Imaging: ¾ ¾ ¾ A very specialized branch of anatomy and physiology that is essential for the diagnosis of many disorders is medical imaging, one division of which is radiography, which includes the use of xrays. Medical imaging techniques allow physicians to peer inside the body to provide clues to abnormal anatomy and deviations from normal physiology in order to help diagnose disease. Medical Imaging: Exhibit 1.4 describes some commonly used medical imaging techniques, including conventional radiography, computed tomography (CT) scanning, dynamic spatial reconstruction (DSR), digital subtraction angiography (DSA), fluoroscopy, positron emission tomography (PET), magnetic resonance imaging (MRI and ultrasound (US). 3 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System ¾ ¾ Interpretation Of Conventional X-rays: One of the first things that can be observed on a conventional roentgenogram is that certain bodily structures and materials are radiolucent (form dark regions on exposed x-ray film) and others are radiopaque (form images that vary from sheer haziness to solid white regions on exposed x-ray film). Interpretation Of Conventional X-rays: Each body system that can be examined utilizing x-ray is evaluated using specific criteria to indicate the presence of abnormalities. Certain features commonly alert the radiologist to possible problems; variations in size, density, and shape of internal structures are often revealing. 4 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System Introduction • A tissue is a group of similar cells that usually have a similar embryological origin and are specialized for a particular function. – The nature of the extracellular material that surrounds the tissue cells and connections between the cells that compose the tissue influence the structure and properties of a specific tissue. – The science that deals with the study of tissues is called histology. Introduction • Pathologists, physicians who specialize in laboratory studies of cells and tissues, aid other physicians in making diagnoses; they also perform autopsies. Analysis of biopsies, samples of living tissue removed for microscopic examination, is a chief responsibility of a pathologist. Types Of Tissues and Their Origins • • • • • Depending on their function and structure, the various tissues of the body are classified into four principal types: epithelial, connective, muscular, and nervous. – Epithelial tissue covers body surfaces; lines hollow organs, body cavities, and ducts; and forms glands. – Connective tissue protects and supports the body and its organs, binds organs together, stores energy reserves as fat, and provides immunity. – – Muscle tissue is responsible for movement and generation of force. Nervous tissue initiates and transmits action potentials (nerve impulses) that help coordinate body activities. Types Of Tissues and Their Origins All tissues and organs of the body develop from one or more of the three primary germ layers: ectoderm, endoderm, and mesoderm. Extracellular fluid (ECF) is external to all body cells, providing a medium for dissolving and mixing solutes, transporting substances, and carrying out chemical reactions. – Interstitial (intercellular) fluid, a subdivision of the ECF, fills the microscopic spaces (interstitial spaces) between cells in tissues. – Plasma, the other subdivision of the ECE, is the liquid portion of blood, found in blood vessels. Cell Junctions Cell junctions are points of contact between adjacent plasma membranes. Three types of cell junctions serve distinct functions. – Tight junctions form fluid-tight seals between cells and are common among epithelial cells that line the stomach, intestines, and urinary bladder. – Anchoring junctions fasten cells to one another or to the extracellular material. – Communicating junctions allow the rapid spread of action potentials from one cell to the next in some parts of the nervous system and in muscle of the heart and gastrointestinal tract. Epithelial Tissues • General Features of Epithelial Tissues – Following are the general features of epithelial tissue. • Epithelium consists mostly of closely packed cells with little extracellular material. • Epithelial cells are arranged in sheets, in either single or multiple layers. • An epithelial cell has an apical surface and a basal surface attached to a basement membrane. • Many cell junctions are present, providing secure attachments among the cells. 5 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System • • • • • • • • • Epithelial Tissues Epithelia are avascular; exchange of materials between epithelium and adjacent connective tissue is by diffusion. Epithelia adhere firmly to nearby connective tissue via a thin extracellular layer, the basement membrane. Epithelia have a nerve supply. Epithelia have a high capacity for renewal (high mitotic rate) Epithelia are derived from all three primary germ layers. Covering and Lining Epithelium The arrangement of covering and lining epithelium reflects its location and function Layers are arranged as simple (one layer), stratified (several layers), and pseudostratified (one layer that appears as several). Cell shapes include squamous (flat), cuboidal (cube-like), columnar (rectangular), and transitional (variable). Covering and lining epithelia may be classified as a combination of arrangement of layers and shape of the cells. The name of the specific type of stratified epithelium depends on the shape of the surface cells. Simple Squamous Epithelium • Consists of a single layer of flat, scale like cells. • It is adapted for diffusion and filtration and is found in lungs and kidneys; in serous membranes, it functions in osmosis and secretion. Simple Cuboidal Epithelium • Consists of a single layer of cube-shaped cells. – It is adapted for secretion (the production and release by cells of a fluid that may contain a variety of substances, such as mucus, perspiration, or enzymes) and absorption (the intake of fluids or other substances by cells). Simple Columnar Nonciliated Epithelium • Consists of a single layer of nonciliated rectangular cells. – It functions in secretion of mucus and in absorption. Simple Columnar Ciliated Epithelium • Consists of a single layer of ciliated rectangular cells. – It moves fluids or particles along a passageway by ciliary action. Stratified Squamous Epithelium • • Consists of several layers of cells in which the top layer is flat and performs a protective function. – A keratinized variety forms the outer layer of skin; keratin is a protein that is waterproof, resistant to friction, and helps repel bacteria. – A nonkeratinized variety lines the mouth, esophagus, part of the epiglottis, and vagina, and covers the tongue. Stratified Cuboidal Epithelium Consists of several layers of cells in which the top layer is cube-shaped. – It functions in protection. 6 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System Stratified Columnar Epithelium • • Consists of several layers of cells in which the top layer is rectangular. – It protects and secretes. Transitional Epithelium Consists of several layers of cells whose appearance is variable. – It is capable of stretching and thus permits distention of an organ. Pseudostratified Columnar Epithelium • Has only one layer but gives the appearance of many. – It functions in secretion and movement of mucus by ciliary action. Glandular Epithelium • • A gland is a single cell or a mass of epithelial cells adapted for secretion. Exocrine glands (sweat, oil, and digestive glands) secrete their products into ducts that empty at the surface of covering and lining epithelium or directly onto a free surface. – Endocrine glands are ductless; their secretary products (hormones) enter the extracellular fluid and diffuse into the blood. Connective Tissue: General Features • Connective tissue is the most abundant tissue in the body. • Connective tissue consists of three basic elements: cells, ground substance, and fibers (the latter two of which combine to form the matrix). Matrix is abundant with relatively few cells. • Unlike epithelia, connective tissues do not occur on free surfaces. • • • Connective Tissue: General Features Except for cartilage, connective tissue, like epithelium, has a nerve supply. Unlike epithelium, connective tissue is highly vascular (except for cartilage and tendons). The matrix of a connective tissue, which may be fluid, semifluid, gelatinous, fibrous, or calcified, is usually secreted by the connective tissue cells and adjacent cells and determines the tissue’s qualities. Connective Tissue Cells • Cells in-connective tissue are derived from mesenchyme. • Immature cells have names that end in -blast (e.g., fibroblast, chondroblast) while mature cells have names that end in -cyte (e.g., osteocyte). • Most mature cells have reduced capacity for cell division and matrix formation and are mostly involved in maintaining the matrix. Connective Tissue Matrix • The ground substance and fibers, deposited in the space between the cells, comprise the matrix of connective tissue. • Substances found in the ground substance include; • Hyaluronic acid, Chondroitin sulfate, Dermatan sulfate, and Keratan sulfate. – The function of ground substance is that it supports, binds, and provides a medium for the exchange of materials between the blood and cells, and is active in influencing cell functions. 7 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System Fibers • Fibers in the matrix provide strength and support for tissues • Three types of fibers are embedded in the matrix between cells of connective tissues. – Collagen fibers, composed of the protein collagen, are very tough and resistant to stretching, yet allow some flexibility in tissue; they are found in bone, cartilage, tendons, and ligaments. – Elastic fibers, composed of the protein elastin, provide strength and stretching capacity and are found in skin, blood vessels, and lungs. – Reticular fibers, consisting of collagen and glycoprotein, provide support in the walls of blood vessels and form a strong, supporting network around fat cells, nerve fibers, and skeletal and smooth muscle fibers. Embryonic Connective Tissue • • • Connective tissue that is present primarily in the embryo or fetus is called embryonic connective tissue. Mesenchyme, found almost exclusively in the embryo, is the tissue from which all other connective tissues eventually arise. Mature Connective Tissue Mature connective tissue exists in the newborn, has cells differentiated from mesenchyme, and does not change after birth. It is subdivided into several kinds: – Connective tissue proper, cartilage, bone tissue, and blood. Subtypes include loose connective tissue, dense connective tissue, cartilage, bone, and blood. – In loose connective tissue, the fibers are loosely woven and there are many cells. Loose Connective Tissue • Areolar connective tissue consists of all three types of fibers, several types of cells, and a semifluid • • ground substance. – It functions in lending strength, elasticity, and support. Adipose tissue consists of adipocytes, specialized for storage of triglycerides. – It reduces heat loss through the skin, serves as an energy reserve, supports, protects, and generates considerable heat to help maintain proper body temperature in newborns (brown fat). Reticular connective tissue consists of fine interlacing reticular fibers and reticular cells. – It forms the stroma of organs and binds together smooth muscle tissue cells. Dense Connective Tissue • Contains more numerous and thicker fibers but considerably fewer cells than loose connective tissue. – It forms tendons, ligaments, and aponeuroses. – It provides strong attachments between various structures. • Dense irregular connective tissue consists of randomly arranged collagenous fibers and a few fibroblasts. Elastic Connective Tissue • Consists of elastic fibers and fibroblasts. – It allows stretching of various organs. 8 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System Cartilage • • • • Has jelly-like matrix (chondroitin sulfate) containing collagenous and elastic fibers and chondrocytes; it is surrounded by perichondrium. • Unlike other connective tissues, cartilage has no blood vessels or nerves (except in the perichondrium). • The strength of cartilage is due to its collagen fibers while its resilience is due to the presence of chondroitin sulfate. Types of Cartilage There are three major types of cartilage. – Hyaline cartilage is the most abundant type of cartilage and has fine collagen fibers embedded in a gel-type matrix. • It is flexible, allows movement at joints, and provides support. – Fibrocartilage contains bundles of collagen in its matrix. • It functions in support and fusion. – Elastic cartilage contains a thread-like network of elastic fibers within the matrix. • It gives support and maintains shape. The Growth of Cartilage Is accomplished by interstitial (endogenous) growth (expansion from within) and appositional (exogenous) growth (from without). Bone (Osseous Tissue) Consists of a matrix containing mineral salts and collagenous fibers and cells called osteocytes; it is surrounded by periosteum. – Calcium salts are responsible for bone’s hardness and collagen fibers for its great strength. – It supports, protects, helps provide movement, stores minerals, and houses blood-forming tissue. Blood (Vascular Tissue) • Consists of a liquid matrix called plasma and formed elements. – – Formed elements include erythrocytes, leukocytes, and thrombocytes. Blood is involved in transport, phagocytosis, allergic reactions, immunity, and clotting. Membranes • The combination of an epithelial layer and an underlying connective tissue layer constitutes an epithelial membrane. Examples are mucous, serous, and cutaneous membranes. – Synovial membranes line joint cavities, bursae, and tendon sheaths and do not contain epithelium; they also secrete a lubricating synovial fluid. Muscle Tissue • • Muscle tissue consists of fibers (cells) that are modified for contraction and thus provide motion, maintenance of posture, and heat production. Types of Muscle Tissue Three types. – Skeletal muscle tissue is attached to bones, is striated, and is voluntary. – Cardiac muscle tissue forms most of the heart wall, is striated, and is usually involuntary. It pumps blood to all parts of the body. – Smooth (visceral) muscle tissue is found in the walls of hollow internal structures (blood vessels and viscera), is nonstriated, and is usually involuntary. It provides motion (e.g., constriction of blood vessels and airways, propulsion of foods through the gastrointestinal tract, and contraction of the urinary bladder and gallbladder). 9 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System • • • • Nervous Tissue The nervous system is composed of only two principal kinds of cells: neurons (nerve cells), and neuroglia (protective and supporting cells). Most neurons consist of a cell body and two types of processes called dendrites and axons. Neurons are sensitive to stimuli, convert stimuli into nerve impulses, and conduct nerve impulses to other neurons, muscle fibers, or glands. Neuroglia protect and support neurons and are often the sites of tumors of the nervous system. 10 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System • • • • • • Introduction An organ consists of a group of tissues that performs a specific function. The tissues comprising the skin are the epithelium of the epidermis and the connective tissues of the dermis. A system is a group of organs working together toward common goals. The organs that make up the integumentary system are the skin and its derivatives, such as hair, nails, glands, and nerve endings; many interrelated factors (e.g., nutrition, hygiene, circulation, age, immunity, genetic traits, psychological state, and drugs) affect both appearance and health of skin. Skin The skin is one of the larger organs of the body; dermatology is the medical specialty that deals with diagnosing and treating skin disorders. Anatomy – Structurally, the skin consists of two principal parts. • The epidermis is the outer, thinner portion, composed of epithelium. • The inner, thicker dermis is composed of connective tissue; it overlies the subcutaneous layer (also called superficial fascia or hypodermis). Skin • • • Physiology – The skin serves several functions: • Regulation of body temperature; Protection; Sensation;Excretion; Immunity; Blood reservoir • Synthesis of vitamin D – An hour of sunlight per week is sufficient to activate the body’s own vitamin D precursor; vitamin D can also be consumed in fortified milk. – Vitamin D deficiency can arise if skin is kept completely covered outdoors, if one rarely goes outdoors, or if one doesn’t drink milk. Epidermis The epidermis is composed of stratified squamous epithelium and contains four principal types of cells: keratinocytes, melanocytes, Langerhans cells, and Merkel cells. Four or five (palm and sole) distinct layers of cells form the epidermis. – The epidermal layers, from deepest to most superficial, are the stratum basale (stratum germinativum), stratum spinosum, stratum granulosum, stratum lucidum (only in palms and soles), and stratum corneum. – The basale layer undergoes continuous cell division and produces all other layers. Epidermis – The cells in the multiple layers of the stratum corneum are continuously shed and replaced by cells from deeper strata. – Keratinization, replacement of cell contents with the protein keratin, occurs as cells move to the skin surface over 2-4 weeks. – Epidermal growth factor (EGF) is a hormone that stimulates growth of epithelial and epidermal cells during tissue development, repair, and renewal. 11 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System Dermis • The dermis is composed of connective tissue containing collagen and elastic fibers and has two regions. – The papillary layer is areolar connective tissue containing fine elastic fibers, dermal papillae, and corpuscles of touch (Meissner ‘s corpuscles). – The reticular layer is irregular connective tissue containing collagen and elastic fibers, adipose tissue, hair follicles, nerve, sebaceous (oil) glands, and ducts of sudoriferous (sweat) glands. • Lamellated, or Pacinian, corpuscles, found in the subcutaneous layer are sensitive to pressure. Skin Color • • The wide variety of colors in skin is due to three pigments--melanin, carotene, and hemoglobin (in blood in capillaries) in the dermis. The color of skin and mucous membranes can provide clues for diagnosing certain problems, such as cyanosis, jaundice, and erythema. Epidermal Ridges • Epidermal ridges increase friction for better grasping ability and provide the basis for fingerprints and footprints. The ridges typically reflect contours of the underlying dermis. Skin Grafts • When the germinal portion of the epidermis is destroyed, new skin cannot regenerate without a skin graft The most successful type of skin graft comes from the individual himself or from an identical twin. • Another type of self-donation is autologous skin transplantation, in which sheets of skin are grown in the laboratory from a small amount of the patient’s epidermis; synthetic materials may be used to simulate dermis and epidermis while this skin is being grown. • • • Epidermal Derivatives Epidermal derivatives are structures developed from the embryonic epidermis Among the epidermal derivatives are hair, skin glands (sebaceous, sudoriferous, and ceruminous), and nails. Hair or pill, are epidermal growths that function in protection and reduction in heat loss. – Hair consists of a shaft above the surface, a root that penetrates the dermis and subcutaneous layer and a hair follicle. – Associated with hairs are sebaceous (oil) glands, errectors pili muscles, and root plexuses. Epidermal Derivatives • • – New hairs develop from cell division of the matrix in the bulb; hair replacement and growth occur in a cyclic pattern. – The color of hair is primarily due to melanin. Hormones, particularly androgens, can stimulate hair growth in both males and females or somehow inhibit it in genetically predisposed males (male-pattern baldness). Drug treatment occasionally stimulates regrowth of some lost hair. Epidermal Derivatives Sebaceous Glands – Sebaceous (oil) glands are usually connected to hair follicles; they are absent in the palms and soles. • Sebaceous glands produce sebum, which moistens hairs, waterproofs and softens the skin, and inhibits bacterial growth. 12 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System • Enlarged sebaceous glands may produce blackheads, pimples, and boils. Epidermal Derivatives • Sudoriferous (sweat) glands are divided into apocrine and eccrine types. – Ecerine sweat glands have an extensive distribution; their ducts terminate at pores at the surface of the epidermis. – Apocrine sweat glands are limited in distribution to the skin of the axilla, pubis, and areolae; their ducts open into hair follicles. – Sudoriferous glands produce perspiration (sweat), which assists in maintaining body temperature and also carries small amounts of wastes to the surface. • Ceruminous glands are modified sudoriferous glands that produce a waxy substance called cerumen. They are found in the external auditory meatus. Epidermal Derivatives • Nails – Nails are hard, keratinized epidermal cells over the dorsal surfaces of the terminal portions of the fingers and toes. – The principal parts of a nail are the body, free edge, root, lunula, eponychium, and matrix. – Cell division of the matrix cells produces new nails. – Functionally, nails help in grasping and manipulating small objects in various ways and provide protection against trauma to the ends of the digits. Skin Wound Healing: Homeostasis of Skin Structure • • Epidermal Wound Healing – In an epidermal wound (e.g., an abrasion or a first-degree or second-degree burn), the central portion of the wound usually extends deep down to the dermis, whereas the wound edges usually involve only superficial damage to the epidermal cells. • Epidermal wounds are repaired by enlargement and migration of basal cells, contact inhibition, and division of migrating and stationary basal cells. Skin Wound Healing: Homeostasis of Skin Structure Deep Wound Healing – When an injury extends to tissues deep to the epidermis, the repair process is more complex than epidermal healing, and scar formation results. – During the inflammatory phase, a blood clot unites the wound edges, epithelial cells migrate across the wound, vasodilation and increased permeability of blood vessels deliver phagocytes, and fibroblasts form. Skin Wound Healing: Homeostasis of Skin Structure – During the migratory phase, epithelial cells beneath the scab bridge the wound, fibroblasts begin to synthesize scar tissue, and damaged blood vessels begin to grow. During this phase, tissue filling the wound is called granulation tissue. – During the proliferative phase, the events of the migratory phase intensify. – During the maturation phase, the scab sloughs oft the epidermis is restored to normal thickness, collagen fibers become more organized, fibroblasts begin to disappear, and blood vessels are restored to normal. Thermoregulation: Homeostasis of Body Temperature • One of the functions of the skin is the maintenance of a normal body temperature of37’C (98.6’F). • If environmental temperature is high, skin receptors sense the stimulus (heat) and generate impulses (input) that are transmitted to the brain (control center). The brain then sends impulses (output) to sweat glands (effectors) to produce perspiration. As the perspiration evaporates, the skin is cooled and body temperature returns to normal. 13 - © - Dr. Jaeson T. Fournier Lecture Exam One Material: Anatomy and Physiology 121 – Introduction to Human Body, the Tissue Level of Organization and the Integumentary System • The skin-cooling response is a negative feedback mechanism. • Temperature maintenance is also accomplished by adjusting blood flow to the skin. • • • Aging and the Integumentary System Most effects of aging of the skin do not occur until an individual reaches the late forties. Among the effects of aging on the integument are wrinkling, slower growth of hair and nails, dryness and cracking due to sebaceous gland atrophy, decrease in number of melanocytes (gray hair, blotching) and Langerhans cells (decreased immune responsiveness), and loss of subcutaneous fat (thinner skin). Chronic ultraviolet exposure accelerates skin aging and greatly increases skin cancer risk. Developmental Anatomy Of The Integumentary System • • The epidermis is derived from ectoderm. Hair, nails, and skin glands are epidermal derivatives. The dermis is derived from wandering mesenchymal cells. Disorders: Homeostatic Imbalances • Tissue damage from excessive heat, electricity, radioactivity, or corrosive chemicals that destroys (denatures) proteins in the exposed cells is called a burn. – Generally, the systemic effects of a burn are a greater threat to life than are the local effects. – Depending on the depth of damage, skin burns are classified as first-degree and second-degree (partial-thickness) and third-degree (full-thickness). – The seriousness of a burn is determined by its depth, extent, and area involved, as well as the person’s age and general health. When the burn area exceeds 70%, over half of the victims die. Disorders: Homeostatic Imbalances – – Sunburn is injury to the skin as a result of acute overexposure to the UV rays in sunlight. Skin cancer can be caused by excessive exposure to sunlight. • The three most common forms are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and malignant melanoma. • Among the risk factors for skin cancer are skin type, sun exposure, family history, age, and immunologic status. Disorders: Homeostatic Imbalances – Acne is an inflammation of sebaceous glands that usually begins at puberty under the influence of androgens. – Pressure sores, also known as decubitus ulcers, are caused by a constant deficiency of blood to tissues overlying a bony projection that has been subjected to prolonged pressure against an object such as a bed, cast, or splint; the deficiency results in tissue ulceration. 14 - © - Dr. Jaeson T. Fournier