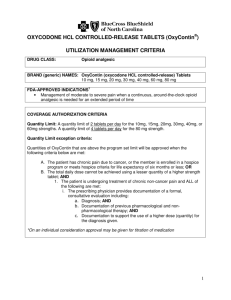
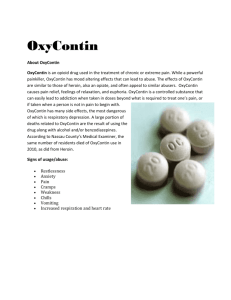
OxyContin - Priority Health
advertisement

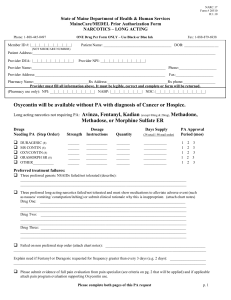
Pharmacy Prior Authorization Form For Prior Authorization, please fax to: 877 974-4411 toll free, or 616 942-8206 Commercial Urgent (life threatening) This form applies to: This request is: Medicaid MIChild Non-Urgent (standard review) Urgent means the standard review time may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. The standard review time averages between 1 and 3 business days. OxyContin® (oxycodone extended-release) Reset Form Member Last Name: ID #: Primary Care Physician: First Name: DOB: Gender: Requesting Provider: Provider Address: Provider NPI: Prov. Phone: Prov. Fax: Contact Name: Provider Signature: Date: Product Information Drug product: OxyContin 10 mg tablet OxyContin 15 mg tablet OxyContin 20 mg tablet OxyContin 30 mg tablet OxyContin 40 mg tablet OxyContin 60 mg tablet Oxycodone ER 80 mg tablet Start date (or date of next dose): Date of last dose (if applicable): Dosing frequency: Precertification Requirements Before this drug is covered, the patient must meet all of the following requirements every 90 days: 1. Must be used for treatment of moderate to severe chronic pain (pain lasting more than 90 days) 2. Must first try extended-release morphine sulfate (generic MS Contin), methadone, and fentanyl patches (methadone is not required when OxyContin is used for patients age 11 to 17). 3. Prescriber must be a participating provider or pre-approved by Priority Health to see our members 4. Oxycodone ER must be prescribed by a single provider, or single practice if Priority Health contracts with other prescribers in the same practice 5. Signed copy of pain management contract containing acceptable language to Priority Health (must be included with request) For continuation, patient must have met the following requirements every 90 days: 1. Patient must see provider for assessment of therapy every 90 days. Page 1 of 2 All fields must be complete and legible for review. Your office will receive a response via fax. Updated 09/2015 Last reviewed 09/2015 Note: Authorization for indications not approved by the Food and Drug Administration (FDA) or recognized in CMS-accepted compendia (e.g. DrugDex, AHFS, U.S. Pharmacopeia, and also Clinical Pharmacology for oncology indications only) require supporting evidence for coverage. New request Priority Health Precertification Documentation A. What is the patient’s diagnosis? moderate to severe chronic pain, for more than 90 days Other: Rationale for use: B. Which of the following medications has the patient had a documented trial with? extended-release morphine sulfate (generic MS Contin) Dates used: methadone Dates used: fentanyl patches Dates used: If any of the above were not tried, explain: C. Is a copy of a pain management contract included with this request? Yes No – rationale: D. Is a copy of the most recent medical chart notes included with this request (office visit within last 90 days)? Yes No – rationale: Continuation request Priority Health Precertification Documentation A. What day was the patient last seen by the prescriber for a pain assessment? Page 2 of 2 All fields must be complete and legible for review. Your office will receive a response via fax. Updated 09/2015 Last reviewed 09/2015