Improved intradialytic stability during haemodialysis with blood volume
advertisement
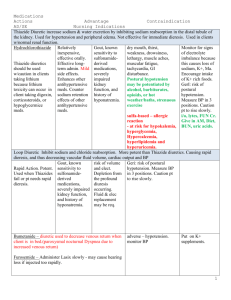
JNEPHROL 2009; 22: 232-240 ORIGINAL ARTICLE www.sin-italy.org/jnonline – www.jnephrol.com Improved intradialytic stability during haemodialysis with blood volume - controlled ultrafiltration Danila Gabrielli1, Batya Kristal2, Krassimir Katzarski3, Maan Youssef4, Toufic Hachache5, František Lopot6, Catherine Lasseur7, Thomas Gunne8, Branimir Draganov9, Ralf Wojke10, Adelheid Gauly10 Abstract Background: Intradialytic morbid events (IMEs) during haemodialysis (HD), including symptomatic hypotension, are related to ultrafiltration (UF)-induced hypovolaemia. Blood volume monitoring and automatic feedback control of the UF rate were developed to limit the extent of hypovolaemia during dialysis. The present study investigated the effect of blood volume (BV)–controlled UF on the incidence of HD treatments with IMEs. Methods: This prospective randomised crossover study included hypotension-prone patients, characterised by occurrence of IMEs in at least 33% of HD treatments during a 6-week screening phase. These patients underwent 2 treatment phases, each lasting 6 weeks, in randomised order. Each patient served as their own control, treated with standard HD in one phase and with BV-controlled UF in the other phase. Hospital of Valle d’Aosta, Aosta - Italy Western Galilee Hospital, Nahariya - Israel 3 Karolinska University Hospital, Stockholm - Sweden 4 Hospital René Dubos, Pontoise - France 5 AGDUC, La Tronche - France 6 General University Hospital, Prague-Strahov - Czech Republic 7 Hospital Saint André, Bordeaux - France 8 General Hospital, Mora - Sweden 9 Ulleval University Hospital, Oslo - Norway 10 Fresenius Medical Care, Bad Homburg - Germany 1 2 Results: Thirty-four patients from 9 HD centres were enrolled; 26 could be included in the analysis population. In comparison with standard HD, BV-controlled UF reduced the percentage of HD sessions complicated by IME significantly from 40% ± 27% to 32% ± 25% (p=0.02). A lower frequency of HD sessions with IME could be observed in 46% of the patients. The frequency of treatments with symptomatic hypotension was reduced from 32% ± 23% in standard HD to 24% ± 21% with BV-controlled UF (p=0.04). Changes in blood pressure and heart rate from start to end of the HD session were not different between the 2 treatment modes. Conclusions: This crossover study showed improved intradialytic stability with BV-controlled UF, compared with standard HD. Key words: Blood volume control, Blood volume moni- tor, Haemodialysis, Intradialytic morbid events, Symptomatic hypotension 232 JN_D_00009_Gauly_GABRIELLI.indd 232 15-04-2009 13:11:42 JNEPHROL 2009; 22: 232-240 introduction Symptomatic hypotension occurs in about 20% of haemodialysis (HD) treatments (1). Factors predisposing patients to develop recurrent hypotensive episodes during HD treatment are various comorbid conditions (2) and the HD procedure itself, which can affect many physiological parameters relevant for cardiovascular stability. The most important factor is certainly the ultrafiltration volume necessary to remove excess body water during HD. If the vascular refilling rate does not keep pace with the ultrafiltration rate, hypovolaemia develops (3, 4). Compensatory mechanisms to hypovolaemia might become ineffective, leading to hypotension. However, the cardiovascular response to hypovolaemia is patient dependent. Interindividually, a wide range of relative blood volumes (RBVs) at which symptomatic hypotension develops has been observed (4-8). These findings indicate that the occurrence of hypotension might be associated with a critical relative blood volume that is specific to an individual patient due to various comorbidities and medications such as antihypertensives. On the other hand, others have found that patients experienced a similar reduction of RBV at the same point in time during HD sessions whether or not intradialytic morbid events (IMEs) occurred (7). A study preceding the present one demonstrated that intrapatient variability in the RBV at which an IME occurred was less than 4% in about 60% of patients investigated (8). The latter data support using a defined critical RBV (RBVcrit) for control of blood volume via adjusting the ultrafiltration (UF) rate to avoid the RBV reaching this critical value during the treatment. This concept is realised in the blood volume monitor (BVM), which enables automatic feedback control of the UF rate thus preventing RBV from falling below the predefined RBVcrit. RBVcrit can be assessed by measuring RBV at the time when IMEs occur during several treatments (9) or in an iterative approach where a mean RBV at occurrence of IMEs in a comparable population (8) is selected and then adjusted from treatment to treatment according to the patient’s needs. The practicability of the latter approach was addressed in the present study, which had the objective of investigating differences in haemodynamic stability in hypotension-prone patients when comparing standard HD with blood volume (BV)–controlled UF. Subjects and methods Patients and study design Patients on thrice-weekly HD with a treatment time of at least 180 minutes and prone to hypotension were enrolled in the study. These were patients in whom at least one third of HD sessions were complicated by IMEs during a 6-week screening phase. IMEs were defined as any symptom occurring during the HD treatment, including symptomatic hypotension, cramps, nausea, dizziness, headache, vomiting, unconsciousness or other adverse symptoms requiring a medical intervention such as transient reduction or premature stop of ultrafiltration, infusion of isotonic or hypertonic saline or glucose solution, Trendelenburg position, blood pressure–stabilising medication or other appropriate measures. Symptomatic hypotension as one form of IME was defined as a drop of blood pressure with symptoms but without predefined level of absolute or relative decrease of blood pressure. The main exclusion criteria were therapeutic approaches potentially confounding the effect of blood volume control on intradialytic stability such as HD performed with sodium or ultrafiltration profiles, application of active blood temperature control, planned changes in dialysate composition or recombinant human erythropoietin dose during the period of the study, current intake of antihypotensive medication, frequent changes of dry body weight (>±1% during screening phase) and various severe medical conditions. The study was designed as an open randomised crossover study to allow intrapatient comparison. Two treatment phases each of 6-week duration were defined. Phase A involved standard HD treatment with a constant UF rate, while phase B involved HD treatment with BV–controlled UF. After the screening phase, patients were centrally randomised to the order A-B (group I) or B-A (group II). Each patient received 18 treatments per study phase. The dialysis prescription in terms of dialyser type, dialysate composition, dialysate temperature, dialysis frequency, planned treatment time, recombinant human erythropoietin dose and antihypertensive medication had to be maintained constant throughout both study phases. The study was performed in adherence with the Declaration of Helsinki. The study protocol was submitted to ethics committees according to national regulations, and written consent was received from all patients recruited for the study. Blood volume monitoring and automated ultrafiltration control UF control via continuous monitoring and feedback control was performed with the blood volume monitor (BVM) in the 4008 HD machine (Fresenius Medical Care, Bad Homburg, Germany). The BVM monitors the RBV from measure233 JN_D_00009_Gauly_GABRIELLI.indd 233 15-04-2009 13:11:43 Gabrielli et al: Haemodialysis and blood volume control ments of blood density which varies with changes in the volume of the vascular space. Blood density is determined by measuring the velocity of ultrasound pulses travelling through a cuvette of precise dimensions which is located in the arterial blood line, as described elsewhere (10). The UF control algorithm in the BVM implements the critical RBV concept, in which an automatic feedback loop controls the ultrafiltration rate (UFR) without changing dialysate sodium. By this means the RBV is always maintained above a predefined value for the respective treatment (RBVcrit). At start of dialysis, double the mean UFR is applied. This rate is reduced as the session progresses and further reduced when the RBV approaches the RBVcrit initially set by the user. If RBV rises above RBVcrit due to vascular refilling, the UFR increases again. The set UF goal for the treatment is always maintained and reached by adjusting the UFR according to the remaining fluid volume to be removed, the remaining treatment time and the RBVcrit set for the respective treatment. The definition of the RBVcrit for an individual patient was established following a practical approach likely to be applied in clinical practice. On the basis of the mean RBV at the time of occurrence of IMEs, which was 88.7% ± 6.2% in a previous study, the initial RBVcrit was set to 89% at the start of phase B in the current study. Adjustments to this value were made in individual patients in subsequent treatments according to the following procedure: If the UF target was not achieved in the planned treatment time, the RBVcrit in a TABLE I BASELINE PATIENT CHARACTERISTICS OF ANALYSIS POPULATION Age, years Sex, % male Dry body weight, kg Time on RRT, years Sessions with IME, % Primary nephropathy, number (%) Primary glomerulonephritis Pyelonephritis Interstitial nephritis Vascular diseases Secondary glomerular/systemic disease Congenital diseases Familiar/hereditary disease Others/unknown Comorbidities, number (%) Diabetes mellitus Coronary heart disease Myocardial insufficiency Previous myocardial infarction Heart failure (NYHA class I, II, III) Peripheral arteriopathy Previous stroke Hypertension Autonomous neuropathy Cardiac arrhythmia requiring treatment Others Group I (n=11) Group II (n=15) All patients (n=26) 70.4 ± 15.0 45.5 65.1 ± 12.6 6.0 ± 4.1 46.7 ± 10.2 69.2 ± 14.0 60.0 66.1 ± 11.2 3.3 ± 2.4 48.0 ± 20.6 69.7 ± 14.0 53.8 65.7 ± 11.6 4.5 ± 3.4 47.5 ± 16.8 2 (18.2) 1 (9.1) 1 (9.1) 1 (9.1) 3 (27.3) - 1 (9.1) 2 (18.2) 2 (13.3) 2 (13.3) - 3 (20.0) 1 (6.7) 1 (6.7) 3 (20.0) 3 (20.0) 4 (15.4) 3 (11.5) 1 (3.8) 4 (15.4) 4 (15.4) 1 (3.8) 4 (15.4) 5 (19.2) 1 (9.1) 6 (54.5) 2 (18.2) 2 (18.2) 4 (36.4) 5 (45.5) 2 (18.2) 8 (72.7) 1 (9.1) 2 (18.2) 5 (45.5) 3 (20.0) 4 (26.7) 2 (13.3) 2 (13.3) 5 (33.3) 4 (26.7) 2 (13.3) 10 (66.7) 2 (13.3) 5 (33.3) 3 (20.0) 4 (15.4) 10 (38.5) 4 (15.4) 4 (15.4) 9 (34.6) 9 (34.6) 4 (15.4) 18 (69.2) 3 (11.5) 7 (26.9) 8 (30.8) Values are means ± SD of the data, or numbers (percentage). IME = intradialytic morbid event; RRT = renal replacement therapy. 234 JN_D_00009_Gauly_GABRIELLI.indd 234 15-04-2009 13:11:43 JNEPHROL 2009; 22: 232-240 given patient was decreased by 1%-2% in the next treatment. Conversely, if the initial RBVcrit was not tolerated by the patient, RBVcrit was then increased by 1%-2% in the subsequent session. The target UF volume had to be defined in both phases as the difference between predialysis body weight and the dry weight. vention was applied to test for statistical significance. For the assessment of group homogeneity, 95% confidence intervals were considered. If not stated otherwise, results are given as means ± standard deviation (SD). Statistical significance is assumed for a p value <0.05. Statistical analysis was performed with the SAS programme package, version 9.1. Study parameters Results The primary outcome variable was the percentage of sessions disturbed by IMEs during each 6-week study phase. The IMEs documented were defined as described for the screening phase (see “Patients and study design”). Blood pressure and heart rate were also measured predialysis and postdialysis. For each session the planned and real treatment time, planned and achieved ultrafiltration volume, dry weight and dry weight changes were recorded. RBV was continuously monitored in both study phases. At baseline and in the last week of each study phase, blood samples were taken predialysis in the mid-week session to determine haematocrit, electrolytes and albumin. Equilibrated Kt/V (eKt/V) was calculated by the Daugirdas second-generation formula (11) using equilibrated postdialysis urea values, which were assessed according to the formula by Smye et al (12). Statistical analysis A linear model for crossover design (ANOVA), which takes into account the effect of study group, time and study inter- Patient characteristics Thirty-four hypotension-prone HD patients from 9 centres were enrolled in the study and randomised to group I (n=16) and group II (n=18). Five patients in group I and 3 patients in group II could not be included in the analysis population. Of these, 6 patients terminated the study prematurely: due to dry weight changes (n=2), change of dialysis centre (n=1), change of renal replacement therapy (n=2) or death not related to the study treatment (n=1). Further, 2 patients had to be excluded from the analysis population due to protocol violations (dry weight change exceeding ±2%). Baseline patient characteristics of the 26 patients of the analysis population are given in Table I. They were comparable between groups I and II, except for time on renal replacement therapy, which was longer in group I, but without statistical significance. Seventy-seven percent of patients had been prescribed at least one type of antihypertensive agent, and 85% received recombinant human erythropoietin during the study. TABLE II TREATMENT AND PATIENT PARAMETERS BY STUDY PHASE Standard HD BV-controlled UF p Value Real treatment time (minutes) 252.4 ± 26.4 254.3 ± 28.4 0.041 Fluid removal (L) 2.30 ± 0.64 2.30 ± 0.55 0.647 Dry body weight (kg) 65.7 ± 11.6 65.7 ± 11.5 0.406 Body weight predialysis (kg) 68.2 ± 11.9 68.2 ± 11.8 0.748 Body weight post-dialysis (kg) 65.9 ± 11.7 65.9 ± 11.7 0.946 RBV end of session (%) 88.3 ± 5.8 89.7 ± 5.1 0.011 Values are means ± SD of the data, calculated from the means of all treatments of each patient in the respective study phase. BV = blood volume; HD = haemodialysis; RBV = relative blood volume; UF = ultrafiltration. 235 JN_D_00009_Gauly_GABRIELLI.indd 235 15-04-2009 13:11:44 Gabrielli et al: Haemodialysis and blood volume control Fig. 1A, B - Haemodynamic effects of blood volume–controlled ultrafiltration by percentage of treatments (A) and number of intradialytic morbid events or symptomatic hypotension (B). BV = blood volume; HD = haemodialysis; IME = intradialytic morbid event; SH = symptomatic hypotension; UF = ultrafiltration. Treatments The fluid removal achieved was unchanged between the two treatment phases in both groups. The planned treatment time was 254 ± 29 minutes and 255 ± 29 minutes, whereas the real treatment time amounted to 252 ± 26 minutes and 254 ± 28 minutes (p=0.041) in standard HD and in BV-controlled UF, respectively. According to the protocol and due to exclusion of protocol violators from the analysis population, the dry weight was not different between both study phases (Tab. II). In phase A, patients were eating or drinking in 49% of the sessions, in phase B during 53%. Treatment parameters had to be maintained constant throughout the study; mean dialysate temperature was 36.5°C ± 0.4°C, and mean dialysate sodium 140 ± 1 mmol/L. Mean RBVcrit set at start of the study phase B was 88.6% ± 1.2%. Few patients started phase B with a RBVcrit lower than 89% despite protocol instructions. Throughout the study phase, RBVcrit was increased in 2 patients, and decreased in 14 patients resulting in a mean of 86.5% ± 3.4% at the end of the 6-week period. At the start of the individual treatment, the RBV was by definition 100%; during the session, the RBV decreased, and at the end of the session, a lower mean RBV was found in standard HD than in HD with BV-controlled UF (p=0.011; Tab. II). Haemodynamic effect of blood volume–controlled UF During HD with BV-controlled UF, the percentage of sessions disturbed by IMEs was lower with BV-controlled UF (32.0% ± 25.5%) than in standard HD (40.1% ± 27.3%; p=0.02), equivalent to a reduction of 20% (Fig. 1A). BV- TABLE III FREQUENCY OF TREATMENTS REQUIRING APPLICATION OF SOLUTIONS TO TREAT AN INTRADIALYTIC MORBID EVENT Percentage of treatments with application of: Hypertonic solutions Isotonic solutions Standard HD BV-controlled UF p Value 16.0 ± 24.4 14.3 ± 16.6 12.0 ± 22.9 11.8 ± 13.8 0.199 0.292 Values are means ± SD of the data. BV = blood volume; HD = haemodialysis; UF = ultrafiltration. 236 JN_D_00009_Gauly_GABRIELLI.indd 236 15-04-2009 13:11:47 JNEPHROL 2009; 22: 232-240 controlled UF reduced the frequency of treatments with IMEs in 46% of the patients. Comparable effects could be demonstrated for the mean number of IMEs per HD treatment, reduced from 0.53 ± 0.41 to 0.42 ± 0.41 (p=0.04; Fig. 1B). Accordingly, the frequency of HD sessions with symptomatic hypotension (SH) and the mean number of SH episodes per treatment were significantly reduced with BV-controlled UF (Fig. 1A, B). A similar effect is seen including all recruited patients in the analysis, therefore the introduction of a systematic bias by excluding dropouts and protocol violators from the analysis population is unlikely. In accordance with a lower percentage of sessions with IMEs, the frequency of treatments with a need for hyper- tonic and isotonic solutions was lower in phase B than in phase A, but the difference did not reach statistical significance (Tab. III). Decreases in blood pressure and increases in heart rate from start to end of the HD session were not different between the two treatment modes (Tab. IV). Effects on other parameters There was no significant difference between the achieved dialysis dose (eKt/V) between phase A and B (see Tab. V). Laboratory data also showed no significant differences between the two study phases. TABLE IV PREDIALYSIS TO POSTDIALYSIS CHANGE OF BLOOD PRESSURE (BP) AND HEART RATE Systolic BP (mm Hg) Predialysis Postdialysis Δ Post-Pre Diastolic BP (mm Hg) Predialysis Postdialysis Δ Post-Pre Heart rate (per minute) Predialysis Postdialysis Δ Post-Pre Standard HD BV-controlled UF p Value 132.3 ± 21.0 121.2 ± 21.2 -11.2 ± 16.9 134.7 ± 21.7 124.5 ± 23.9 -10.1 ± 18.9 0.165 0.104 0.254 69.7 ± 12.3 65.4 ± 12.0 -4.6 ± 8.6 70.2 ± 13.3 65.5 ± 12.5 -4.9 ± 8.8 0.631 0.894 0.939 74.3 ± 8.8 79.0 ± 9.6 4.7 ± 8.6 74.0 ± 8.3 77.7 ± 9.9 3.5 ± 7.7 0.550 0.220 0.231 Values are means ± SD of the data, calculated from the means of all treatments of each patient in the respective study phase. Δ = change; BV = blood volume; HD = haemodialysis; UF = ultrafiltration. TABLE V DELIVERED DIALYSIS DOSE AND SERUM PREDIALYSIS LABORATORY PARAMETERS AT THE END OF EACH 6-WEEK STUDY PHASE eKt/V Sodium (mmol/L) Total calcium (mg/dL) Haematocrit (%) Albumin (g/L) Standard HD BV-controlled UF p Value 1.12 ± 0.30 138.9 ± 3.0 9.8 ± 0.7 35.3 ± 5.0 34.9 ± 3.0 1.17 ± 0.28 139.6 ± 2.9 10.1 ± 0.8 35.3 ± 5.5 35.0 ± 3.1 0.156 0.510 0.060 0.723 0.678 Values are means ± SD of the data. BV = blood volume; eKt/V = equilibrated Kt/V; HD = haemodialysis; UF = ultrafiltration. 237 JN_D_00009_Gauly_GABRIELLI.indd 237 15-04-2009 13:11:47 Gabrielli et al: Haemodialysis and blood volume control Discussion The present study demonstrated that feedback control of UF via continuous monitoring of the relative blood volume was able to reduce the frequency of sessions with intradialytic morbid events in a hypotension-prone HD population from 40% during standard HD to 32%. This reduction rate (equivalent to 20%) is somewhat lower than in previous studies (13-20). However, in contrast to the methods applied in those studies, our results were achieved without modification of dialysate sodium during the treatment. In our study population, 46% of the patients responded to the study intervention, which is consistent with findings of other studies that have identified responders and nonresponders or high/low responders to BV-controlled UF (14, 21). The frequency of sessions disturbed by IMEs could be reduced maintaining the UF volume achieved, in both study phases. Although the planned treatment time was nearly identical between both treatment modes, the real treatment time was on average about 2 minutes longer during BV-controlled UF. Although statistically significant, we do not believe that this small difference of less than 1% of the treatment time could explain the 20% reduction of HD sessions with IMEs. During standard HD, the mean RBV at the end of the session was slightly lower than during BVcontrolled UF, and was thus likely to fall more often below the individually tolerable RBVcrit of the respective patient, which in turn was reflected by the higher IME rate. However, as the difference of RBV at the end of the session was small, it is possible that not only hypovolaemia but also shape and behaviour of the RBV signal in response to the different UF patterns throughout the treatment might be predictors for the occurrence of symptomatic hypotension (7, 22). The effectiveness of mechanisms to compensate for hypovolaemia might depend on factors such as age and the presence of cardiovascular comorbidities (1). This may explain an individual threshold of tolerable RBV (8), albeit with an intrapatient variability due to fluctuations of the degree of overhydration, a potentially incorrect assessment of dry body weight and other factors affecting acute responses to UF. There are also patients with no association between hypovolaemia and hypotension, in whom the control of blood volume is without effect (21). Takeda et al was able to identify predictors of volume-dependent hypotension such as diabetes and interdialytic body weight increase (23). However, in our study we could not consider such predictors as the sample size was too small, and such analyses had not been predefined in the study protocol. Although unchanged dry weight (<±1%) was prescribed by the protocol, and protocol violators were excluded from the analysis population, a change of body composition – e.g., of total body water within these dry weight limits, with potential influence on the vascular refilling rate – cannot be excluded. The patient-specific threshold of RBVcrit and the relationship between the RBV and the occurrence of IMEs are still matters of debate. Zucchelli and Santoro showed that in hypotension-prone patients, the RBV reduction at the end of dialysis was more pronounced than in hypotension-resistant patients, likely due to an individual defect in the refilling capacity (24). Also Cai et al were able to relate the occurrence of hypotension due to hypovolaemia to a reduction of central blood volume as measured by thoracic electrical impedance (25). Barth et al (8) identified an individual RBV limit at which haemodynamic instability occurs with a limited intrapatient variability in most patients. However, other authors could not confirm in their studies any relationship between a predefined RBV limit and the onset of symptomatic hypotension (7, 26). In one study, symptomatic hypotension occurred in only 2 patients, which limits the general applicability of these results (26). Nette et al found a wide interpatient variability of RBV preceding the moment at which hypotension occurred. This might be attributable to a different degree to which patients are affected by cardiovascular comorbidities and the difficulty of precisely determining dry weight. Therefore, the development of hypotension was related to impairments of cardiovascular compensatory mechanisms rather than hypovolaemia (6). Nevertheless, the present study used the concept of a RBVcrit which had to be set at the start of the treatment. Starting from the mean value of RBVcrit of 89% as determined in an earlier study with 60 hypotension-prone patients (8), RBVcrit was then adjusted in the subsequent treatments according to the patient outcome of the initial treatment. The need for adjustments in RBVcrit from time to time probably reflects changes in the prevailing circumstances, especially changes in fluid status. Therefore, a flexible approach allowing RBVcrit adjustments even during the treatment would be desirable. Considering actual changes in such circumstances, such as the degree of overhydration, and adjusting the RBVcrit accordingly, may improve fluid management (Tovbin et al. Abstract ERA-EDTA 2005; http://www.abstracts2view.com/era/view.php?nu=ERA5L_462) In a study conducted by Reddan et al, intradialytic blood volume was monitored and a manual intervention protocol was applied including interruption of UF and changing the UF goal. No effect on the occurrence of intradialytic hypotension and other complications related to the treatment procedure was found (27). Thus, an automatic feed- 238 JN_D_00009_Gauly_GABRIELLI.indd 238 15-04-2009 13:11:48 JNEPHROL 2009; 22: 232-240 back loop inherent in the blood volume monitor to instantaneously react to changes in patient parameters seems a more promising approach to improving haemodynamic stability during HD. The decrease in blood pressure and increase in heart rate were only marginally less pronounced in BV-controlled UF than in standard HD, similar to observations in other studies (13, 14, 16). Despite promising results in this study, we acknowledge some limitations. It was an open study, in which patient and user bias can never be excluded. The patient number was still small and did not allow adjusting for various treatment- and patient-related pathologies, or for the possibility that current fluid status was potentially responsible for the development of hypotension. However, the intrapatient comparisons and unchanged treatment parameters between the two phases should have minimised these effects. Further, the improvements in cardiovascular stability during the treatment with BV-controlled UF could possibly have been more pronounced if we had also applied active body temperature control (28). In summary, the present crossover study demonstrated that the frequency of HD treatments complicated by intradialytic morbid events including symptomatic hypotension was reduced with BV-controlled UF as compared with References 1. standard HD. This was achieved without modification of dialysate sodium, while maintaining UF volume and comparable treatment time. Acknowledgements We thank the staff of all of the participating centres for their dedicated contribution to this study. The review of the manuscript by Paul Chamney is gratefully acknowledged. Statistical analysis was performed by M. Hohn, c-m-h GmbH, Waldems, Germany. Financial support: The study has been funded by Fresenius Medical Care. Conflict of interest statement: R. Wojke and A. Gauly are employees of Fresenius Medical Care. Address for correspondence: Adelheid Gauly, PhD Fresenius Medical Care Deutschland GmbH Else-Kroener-Strasse 1 D-61352 Bad Homburg, Germany adelheid.gauly@fmc-ag.com 5. Changes in blood volume during dialysis are dependent upon the rate and amount of ultrafiltrate. ASAIO Trans. Daugirdas JT. Pathophysiology of dialysis hypotension: an 1989;35:250-252. update. Am J Kidney Dis. 2001;38:S11-S17. 2. Schreiber MJ Jr. Clinical case-based approach to understanding 6. 4. and left ventricular function. Clin Nephrol. 2005;63:276-283. Sherman RA. The pathophysiologic basis for hemodialysisrelated hypotension. Semin Dial. 1988;1:136-142. Nette RW, van den Dorpel MA, Krepel HP, et al. Hypotension during hemodialysis results from an impairment of arteriolar tone intradialytic hypotension. Am J Kidney Dis. 2001;38:S37-S47. 3. Mann H, Ernst E, Gladziwa U, Schallenberg U, Stiller S. 7. Andrulli S, Colzani S, Mascia F, et al. The role of blood volume Leunissen KM, Kooman JP, van der Sande FM, van Kuijk WH. reduction in the genesis of intradialytic hypotension. Am J Hypotension and ultrafiltration physiology in dialysis. Blood Kidney Dis. 2002;40:1244-1254. Purif. 2000;18:251-254. 8. Barth C, Boer W, Garzoni D, et al. van der SF, Wojke R, Schil- 239 JN_D_00009_Gauly_GABRIELLI.indd 239 15-04-2009 13:11:48 Gabrielli et al: Haemodialysis and blood volume control 9. ling H, Passlick-Deetjen J: Characteristics of hypotension- response to hypovolemia. Kidney Int. 2004;65:1499-1510. prone haemodialysis patients: is there a critical relative blood 20. Dasselaar JJ, Huisman RM, de Jong PE, Burgerhof JG, Frans- volume? Nephrol Dial Transplant. 2003;18:1353-1360. sen CF. Effects of relative blood volume-controlled hemodi- Garzoni D, Keusch G, Kleinoeder T, et al. Reduced complica- alysis on blood pressure and volume status in hypertensive tions during hemodialysis by automatic blood volume controlled ultrafiltration. Int J Artif Organs. 2007;30:16-24. patients. ASAIO J. 2007;53:357-364. 21. Donauer J, Kolblin D, Bek M, Krause A, Bohler J. Ultrafiltra- 10. Johner C, Chamney PW, Schneditz D, Kramer M. Evaluation tion profiling and measurement of relative blood volume as of an ultrasonic blood volume monitor. Nephrol Dial Trans- strategies to reduce hemodialysis-related side effects. Am J plant. 1998;13:2098-2103. Kidney Dis. 2000;36:115-123. 11. Daugirdas JT. Second generation logarithmic estimates of 22. Mitra S, Chamney P, Greenwood R, Farrington K. Linear de- single-pool variable volume Kt/V: an analysis of error. J Am cay of relative blood volume during ultrafiltration predicts he- Soc Nephrol. 1993;4:1205-1213. modynamic instability. Am J Kidney Dis. 2002;40:556-565. 12. Smye SW, Dunderdale E, Brownridge G, Will E. Estimation 23. Takeda A, Toda T, Fujii T, Sasaki S, Matsui N. Can predialysis of treatment dose in high-efficiency haemodialysis. Nephron. hypertension prevent intradialytic hypotension in hemodialy- 1994;67:24-29. 13. Basile C, Giordano R, Vernaglione L, et al. Efficacy and safety of haemodialysis treatment with the Hemocontrol biofeedback system: a prospective medium-term study. Nephrol Dial Transplant. 2001;16:328-334. 14. Santoro A, Mancini E, Basile C, et al. Blood volume controlled hemodialysis in hypotension-prone patients: a randomized, multicenter controlled trial. Kidney Int. 2002;62:1034-1045. 15. Wolkotte C, Hassell DR, Moret K, et al. Blood volume control by biofeedback and dialysis-induced symptomatology: a short-term clinical study. Nephron. 2002;92:605-609. 16. McIntyre CW, Lambie SH, Fluck RJ. Biofeedback controlled he- sis patients? Nephron Clin Pract. 2006;103:c137-c143. 24. Zucchelli P, Santoro A. Dialysis-induced hypotension: a fresh look at pathophysiology. Blood Purif. 1993;11:85-98. 25. Cai Y, Zimmerman A, Ladefoged S, Secher NH. Can haemodialysis-induced hypotension be predicted? Nephron. 2002;92:582-588. 26. Krepel HP, Nette RW, Akcahuseyin E, Weimar W, Zietse R. Variability of relative blood volume during haemodialysis. Nephrol Dial Transplant. 2000;15:673-679. 27. Reddan DN, Szczech LA, Hasselblad V, et al. Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol. 2005;16:2162-2169. modialysis (BF-HD) reduces symptoms and increases both he- 28. Maggiore Q, Pizzarelli F, Santoro A, et al. The effects of con- modynamic tolerability and dialysis adequacy in non-hypoten- trol of thermal balance on vascular stability in hemodialysis sion prone stable patients. Clin Nephrol. 2003;60:105-112. patients: results of the European randomized clinical trial. Am 17. Franssen CF, Dasselaar JJ, Sytsma P, Burgerhof JG, de Jong J Kidney Dis. 2002;40:280-290. PE, Huisman RM. Automatic feedback control of relative blood volume changes during hemodialysis improves blood pressure stability during and after dialysis. Hemodial Int. 2005;9:383-392. 18. Begin V, Deziel C, Madore F. Biofeedback regulation of ultra- Received: January 03, 2008 Revised: May 09, 2008 Accepted: June 28, 2008 filtration and dialysate conductivity for the prevention of hypotension during hemodialysis. ASAIO J. 2002;48:312-315. 19. Cavalcanti S, Ciandrini A, Severi S, et al. Model-based study of the effects of the hemodialysis technique on the compensatory © Società Italiana di Nefrologia 240 JN_D_00009_Gauly_GABRIELLI.indd 240 15-04-2009 13:11:49