Increased Arterial Carboxyhemoglobin Concentrations in Chronic
advertisement

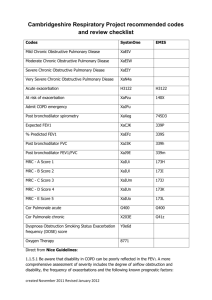
Increased Arterial Carboxyhemoglobin Concentrations in Chronic Obstructive Pulmonary Disease Hiroyasu Yasuda, Mutsuo Yamaya, Katsutoshi Nakayama, Satoru Ebihara, Takahiko Sasaki, Shoji Okinaga, Daisuke Inoue, Masanori Asada, Miyako Nemoto, and Hidetada Sasaki Department of Geriatric and Respiratory Medicine, Tohoku University School of Medicine, Sendai, Japan Rationale: Exhaled carbon monoxide (CO) and arterial blood carboxyhemoglobin concentrations (Hb-CO) increase in inflammatory pulmonary diseases. Objectives: To study whether arterial Hb-CO is useful to monitor disease activity in patients with chronic obstructive pulmonary disease (COPD) who had stopped smoking. Methods: We measured arterial Hb-CO, arteriovenous Hb-CO differences, and FEV1 in 58 patients with COPD and 61 ex-smoking control subjects. Results: Arterial Hb-CO concentrations in patients at stable conditions were higher than those in control subjects (p ⬍ 0.0001). Furthermore, the Hb-CO concentrations in patients at the exacerbations (p ⬍ 0.0001) were higher than those at the stable conditions. Arterial Hb-CO concentrations in patients at stage III were higher than those in patients at stage II, and the Hb-CO concentrations in patients at stage IV were higher than those in patients at stage III at the stable conditions and exacerbations. Arterial Hb-CO correlated with exhaled CO in patients with COPD at stage II and stage III at the exacerbations. Arterial Hb-CO inversely correlated with the arterial blood partial oxygen pressure and FEV1. Arteriovenous Hb-CO differences in patients at the exacerbations did not differ from those in patients at stable conditions and from those in control subjects. Moreover, arterial Hb-CO correlated with serum C-reactive protein values and serum lipid peroxide concentrations. Conclusions: These findings suggest that increased arterial Hb-CO may relate to severity in patients with COPD because of lung and systemic inflammation and production of reactive oxygen species. Keywords: carbon monoxide; carboxyhemoglobin; chronic obstructive pulmonary disease; heme oxygenase; systemic inflammation Chronic obstructive pulmonary disease (COPD) is a major global health problem that has an increasing disease burden and effect on health care spending and is characterized by airflow limitation that is not fully reversible (1). Various factors are associated with the pathogenesis of COPD, including oxidative stress (2), inflammatory cells (3, 4), such as activated neutrophils and mononuclear leukocytes (5), and mediators, including tumor necrosis factor ␣ (6, 7). Furthermore, these factors are associated with the exacerbations of COPD (7–9) caused by airway infection of viruses and bacteria (10, 11). Many reports have suggested that airflow limitation presented by FEV1 inversely correlates with several inflammatory indicators, such as nitric oxide (NO) levels in exhaled air (12, 13), 4-hydroxy-2-nonenal levels in the lung (14), and sputum interleukin-8 levels and soluble tumor necrosis factor receptor (4) in patients with COPD. NO, hydrogen peroxide, ethane, and 4-hydroxy-2-nonenal in exhaled air have been suggested to be (Received in original form July 15, 2004; accepted in final form March 4, 2005) Correspondence and requests for reprints should be addressed to Hiroyasu Yasuda, M.D., Ph.D., Department of Geriatric and Respiratory Medicine, Tohoku University School of Medicine, 1-1 Seiryo-machi, Aoba-ku, Sendai, 980-8574, Japan. E-mail: yasuda@geriat.med.tohoku.ac.jp Am J Respir Crit Care Med Vol 171. pp 1246–1251, 2005 Originally Published in Press as DOI: 10.1164/rccm.200407-914OC on March 11, 2005 Internet address: www.atsjournals.org noninvasive markers in monitoring the production of reactive oxygen species in the lung, and inflammation in the airway and lung in patients with COPD (12–17). On the other hand, the inducible form of heme oxygenase (HO), HO-1, is reported to be expressed in airway epithelial cells (18), endothelial cells (19), and alveolar macrophages (20). Carbon monoxide (CO) is produced endogenously by HO, and is known to be present in measurable quantities in the exhaled air of normal subjects (21, 22). Upregulation of HO-1 by oxidant stress and proinflammatory cytokines (23) in airway and lung inflammation is suggested to cause the increased levels of exhaled CO in patients with inflammatory pulmonary diseases such as bronchial asthma, acute pneumonia, silicosis, bronchiectasis, upper respiratory tract infections (URTIs), and seasonal allergic rhinitis (20, 22, 24–29). Arterial blood carboxyhemoglobin (Hb-CO) concentrations correlate to exhaled CO concentrations (21), and have also been suggested to be an inflammatory marker in inflammatory pulmonary disease, including bronchial asthma, acute pneumonia, and silicosis (27–29). Blood gas analysis is performed in patients with COPD not only at the first visit to the hospital to estimate respiratory failure but also at visits to the hospital because of exacerbations. The arterial Hb-CO concentrations can be measured at the measurement of blood gas. However, Hb-CO concentrations at stable conditions and exacerbations have not been studied in patients with COPD. In the present study, we studied the relationship between Hb-CO concentrations and disease severity in patients with COPD. We also measured the arteriovenous (a-v) Hb-CO concentration differences in patients with COPD to study the systemic and lung inflammation (28) in these patients (30, 31). Some of the results of these studies have been previously reported in the form of an abstract (32). METHODS Subjects We studied 61 control subjects and 58 patients with COPD (Table 1). Of patients with COPD, 28 were classified into stage II, 10 into stage III, and 20 patients into stage IV according to the criteria by the Global Initiative for Chronic Obstructive Lung Disease (33). To avoid the influence of ambient CO on the Hb-CO, we enrolled subjects living uptown in Sendai City in the Miyagi prefecture with the same environment as previously described (28). Furthermore, passive smokers in patients with COPD and control subjects were excluded. Exacerbations of COPD were defined with the criteria previously described (11, 34). At the exacerbations, 18 of 58 patients had symptoms of URTIs defined with the methods previously described (34). Type A influenza virus was isolated from sputum from 7 of the 18 patients with URTIs, and type B influenza was isolated from three patients. In another 30 patients with COPD, 13 patients had acute bronchitis with purulent sputum, and six patients had pneumonia. The patients with exacerbated COPD had been receiving treatment as previously described (35). None of the control subjects were receiving long-term medication. All control subjects and all patients with COPD were ex-smokers. To Yasuda, Yamaya, Nakayama, et al.: Carboxyhemoglobin in COPD 1247 TABLE 1. SUBJECT CHARACTERISTICS Subject Category Age (yr) Male/female (no.) CRP (mg/dl) FEV1 (%pred) PaCO2 (mm Hg) PaO2 (mm Hg) Smoking History (pack-yr) Control (n ⫽ 61) COPD (n ⫽ 58) 69.7 ⫾ 1.2 70.9 ⫾ 1.1 55/6 53/5 0.06 ⫾ 0.01 4.90 ⫾ 0.62* 95.5 ⫾ 0.8 48.9 ⫾ 2.2* 40.5 ⫾ 0.2 53.5 ⫾ 2.1* 90.2 ⫾ 0.8 64.4 ⫾ 1.7* 27 ⫾ 2 58 ⫾ 2* Definition of abbreviations: COPD ⫽ chronic obstructive pulmonary disease; CRP ⫽ C-reactive protein. Values are mean ⫾ SE. * p ⬍ 0.0001. exclude current smokers, we measured urinary cotinine concentrations with high-performance liquid chromatography (36). This study was approved by the Tohoku University Ethics Committee, and informed consent was obtained from each subject. Measurement of Arterial and Venous Blood Hb-CO and Exhaled CO We took blood from the radial artery and the median cubital vein in patients with COPD and in control subjects. We measured the Hb-CO concentrations with a spectrophotometer (18, 27, 37), and calculated the a-v Hb-CO concentration differences (28). We also measured exhaled CO concentrations in the control subjects and patients, as previously described (21, 22, 25, 26, 38). To avoid the influence of ambient CO on Hb-CO, Hb-CO and exhaled CO levels were measured at least 3 hours after arrival in a room in the hospital with low ambient CO. Measurement of Serum Lipid Peroxide Concentrations of lipid peroxide (LPO) in arterial blood serum were measured with methods as previously described (39, 40). Study Protocol We examined the relationships between arterial Hb-CO and either exhaled CO, PaO2 and PaCO2, serum C-reactive protein (CRP), and LPO, or FEV1. Statistical Analysis The age, sex, Hb-CO concentrations, a-v Hb-CO difference, exhaled CO concentrations, arterial blood PaO2 and PaCO2 values, serum CRP values, serum LPO concentrations, and FEV1 in each group are reported as mean ⫾ SE. Statistical analysis of these values was performed by one-way analysis of variance and followed by the Newman-Keuls test. Linear regression analysis was performed using the method of least squares, to compare the relationship between arterial blood Hb-CO and either exhaled CO, PaCO2, PaO2, CRP value, LPO concentrations, or FEV1 in patients with COPD at the exacerbations. Significance was accepted at p ⬍ 0.05. stable conditions. The Hb-CO concentrations were stable and reproducible between two measurements (0.81 ⫾ 0.02 vs. 0.82 ⫾ 0.02%, n ⫽ 58, p ⬎ 0.50). Hb-CO concentrations in patients with COPD at stable conditions (0.81 ⫾ 0.02%, n ⫽ 58) were significantly higher than those in control subjects (0.55 ⫾ 0.02%, n ⫽ 61, p ⬍ 0.0001; Figure 1). Among the patients with COPD at stable conditions, Hb-CO increased in the severe stage of COPD. Hb-CO concentrations in patients at stage III (0.83 ⫾ 0.03%, n ⫽ 10, p ⬍ 0.05) were higher than those in patients at stage II (0.70 ⫾ 0.03%, n ⫽ 24). Hb-CO concentrations in patients at stage IV (0.95 ⫾ 0.03, n ⫽ 20, p ⬍ 0.05) were also higher than those in patients at stage III. The arterial blood Hb-CO concentrations in all patients with COPD at the exacerbations (1.09 ⫾ 0.04%, n ⫽ 58) were significantly higher than those at a stable condition before the exacerbations (0.81 ⫾ 0.02%, p ⬍ 0.0001; Figure 1). Furthermore, among the patients at the exacerbations, Hb-CO increased in the severe stage of COPD. At the exacerbations, Hb-CO concentrations in patients at stage III (1.12 ⫾ 0.05%, n ⫽ 10, p ⫽ 0.0001) were higher than those in patients at stage II (0.85 ⫾ 0.03%, n ⫽ 28). Hb-CO concentrations in patients at stage IV (1.41 ⫾ 0.07%, n ⫽ 20, p ⫽ 0.01) were also higher than those in patients at stage III. Furthermore, in patients at stage IV, the Hb-CO changes between stable conditions and exacerbations (0.47 ⫾ 0.05%) were higher than those in patients at stage III (0.29 ⫾ 0.05%, p ⬍ 0.01), and the Hb-CO changes in patients at stage III were higher than those in patients at stage II (0.14 ⫾ 0.02%, p ⬍ 0.05). RESULTS Subject Characteristics The subject characteristics of patients with COPD and control subjects are shown in Table 1. There was no statistically significant difference in age and sex between normal control subjects and patients. All control subjects and patients were ex-smokers. Furthermore, urinary cotinine concentrations of all subjects were less than 30 ng of the cotinine/mg creatinine ratio, showing that all subjects in this study were not current smokers (22). The patients were treated with sustained-release theophylline and inhaled anticholinergic agents (oxitropium bromide). Furthermore, 10 of 58 patients were treated with inhaled corticosteroids (beclometasone dipropionate or fluticasone propionate). Arterial Blood Hb-CO Concentrations To examine the reproducibility of the arterial blood Hb-CO measurement in stable COPD, we measured the Hb-CO concentrations twice with a 4-week interval in patients with COPD at Figure 1. Arterial blood carboxyhemoglobin (Hb-CO) concentration in healthy ex-smoker control subjects (n ⫽ 61) and in patients with chronic obstructive pulmonary disease (COPD; n ⫽ 58) at the exacerbations and in patients with COPD at a stable condition before the exacerbations. The error bars indicate mean ⫾ SEM. 1248 AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE VOL 171 2005 Hb-CO concentrations in patients with the symptoms of URTIs (1.10 ⫾ 0.08%, n ⫽ 18) were higher than those in control subjects (p ⬍ 0.0001) and those in patients at the stable conditions (0.82 ⫾ 0.04%, p ⬍ 0.0001), but did not differ from those in patients without URTIs at the exacerbations (1.09 ⫾ 0.06%, n ⫽ 40, p ⬎ 0.8). Hb-CO concentrations in patients treated with inhaled corticosteroids did not differ from those in patients without inhaled corticosteroids at the stable conditions (0.87 ⫾ 0.03 vs. 0.80 ⫾ 0.03%, n ⫽ 10, p ⬎ 0.2) and at the exacerbations (1.24 ⫾ 0.08 vs. 1.06 ⫾ 0.05%, p ⬎ 0.1). In the present study, the Hb-CO concentrations in ex-smoking control subjects (n ⫽ 54) with a smoking history of more than 60 pack-years, which was the average smoking history of patients in this study (Table 1), did not differ from the Hb-CO concentrations in the control subjects (n ⫽ 7) with a smoking history of less than 60 pack-years (data not shown). Venous Blood Hb-CO Concentrations The venous blood Hb-CO concentrations were measured in 14 patients with COPD and 16 control subjects. The venous blood Hb-CO concentrations in patients with COPD at a stable condition (0.71 ⫾ 0.04%, n ⫽ 14) were significantly higher than that in control subjects (0.45 ⫾ 0.03%, n ⫽ 16, p ⬍ 0.0001). Furthermore, among the patients at the stable condition, the venous blood Hb-CO increased at the severe stage of COPD. The venous blood Hb-CO concentrations in patients at stage IV (0.83 ⫾ 0.05%, n ⫽ 6, p ⬍ 0.01) were higher than those in patients at stage II (0.58 ⫾ 0.05%, n ⫽ 4). However, the venous blood Hb-CO concentrations in patients at stage III (0.65 ⫾ 0.07%, n ⫽ 4, p ⬎ 0.3) did not differ from those in patients at stage II. Likewise, the venous blood Hb-CO concentrations in patients at stage IV did not differ from those in patients at stage III (p ⫽ 0.052). The venous blood Hb-CO concentrations in all patients with COPD at the exacerbations (1.02 ⫾ 0.09%, n ⫽ 14) were higher than those at a stable condition (p ⬍ 0.0001). In contrast, among the patients at the exacerbations, the venous blood Hb-CO did not increase at the severe stage of COPD (data not shown). A-v Blood Hb-CO Concentration Differences To examine the site of endogenous production of CO, we measured the a-v blood Hb-CO concentration differences in patients with COPD. In these patients, the a-v Hb-CO differences at a stable condition (0.14 ⫾ 0.02%, n ⫽ 14) did not differ from those in control subjects (0.13 ⫾ 0.03%, n ⫽ 16, p ⬎ 0.7). Furthermore, among the patients at a stable condition, the a-v Hb-CO differences did not increase at the severe stage of COPD (data not shown). The a-v Hb-CO differences in all patients with COPD at the exacerbations (0.16 ⫾ 0.03%, n ⫽ 14) did not differ from those in control subjects (p ⬎ 0.5; Figure 2). Furthermore, among the patients at the exacerbations, the a-v Hb-CO differences did not increase with severity of COPD (data not shown). The a-v Hb-CO differences in patients with COPD who had URTIs also did not differ from those in patients without URTIs at the exacerbations (data not shown). Exhaled CO Concentrations Exhaled CO concentrations in patients with COPD at the stable conditions (3.5 ⫾ 0.1 ppm, n ⫽ 58) were significantly higher than those in control subjects (1.8 ⫾ 0.1 ppm, n ⫽ 61, p ⬍ 0.0001). In the patients at stage II and stage III, exhaled CO concentrations (3.8 ⫾ 0.2 ppm, n ⫽ 38) at the exacerbations were higher than those at the stable conditions (p ⬍ 0.001). In Figure 2. Relationship between the arterial blood Hb-CO concentrations and FEV1 in patients with COPD (n ⫽ 54) at the exacerbations (p ⬍ 0.0001, r ⫽ ⫺0.70). contrast, in the patients at stage IV, exhaled CO concentrations at the exacerbations did not differ from those at the stable conditions (data not shown). Exhaled CO concentrations in patients with URTIs (4.0 ⫾ 0.2 ppm, n ⫽ 18) were also higher than those in control subjects (p ⬍ 0.0001) and those in the patients at stable conditions (3.2 ⫾ 0.2 ppm, p ⬍ 0.05). Exhaled CO correlated with the Hb-CO in patients at stage II and stage III at the exacerbations (n ⫽ 38, r ⫽ 0.530, p ⬍ 0.001), but did not correlate with the Hb-CO in patients at stage IV at the exacerbations (data not shown). In patients with COPD at stage III, the exhaled CO concentrations in patients treated with inhaled corticosteroids (3.8 ⫾ 0.5 ppm, n ⫽ 4) did not differ from those in patients without inhalation of corticosteroids at the exacerbations (4.4 ⫾ 0.3 ppm, n ⫽ 6, p ⬎ 0.3). Likewise, in patients at stage IV, the exhaled CO concentrations in patients treated with inhaled corticosteroids (3.1 ⫾ 0.8 ppm, n ⫽ 5) did not differ from those in patients without inhaled corticosteroids at the exacerbations (3.3 ⫾ 0.6 ppm, n ⫽ 12, p ⬎ 0.8). Factors Associated with Arterial Blood Hb-CO Concentrations In patients with COPD at the exacerbations, arterial Hb-CO concentrations inversely correlated with arterial blood PaO2 values (63.3 ⫾ 1.4 mm Hg, n ⫽ 58; r ⫽ ⫺0.70, p ⬍ 0.0001), and correlated with arterial blood PaCO2 values (53.5 ⫾ 2.1 mm Hg, n ⫽ 58; r ⫽ 0.52, p ⬍ 0.0001). Likewise, in the patients at the exacerbations, arterial blood Hb-CO concentrations correlated with serum CRP values (4.9 ⫾ 0.6 mg/dl, n ⫽ 58; r ⫽ 0.56, p ⬍ 0.0001). Arterial Hb-CO concentrations also correlated with serum LPO concentrations (5.63 ⫾ 0.39 nmol/ml, n ⫽ 58; r ⫽ 0.56, p ⬍ 0.0001). Furthermore, in patients at the exacerbations, the Hb-CO inversely correlated with FEV1 (n ⫽ 54, r ⫽ ⫺0.70, p ⬍ 0.0001; Figure 2). On the other hand, in all four patients with an Hb-CO of more than 1.4% at the exacerbations, FEV1 was less than 40%, and in all eight patients with the Hb-CO of more than 1.2% at the exacerbations, FEV1 was less than 50% (Figure 2). DISCUSSION The present study demonstrated that, at stable conditions, Hb-CO concentrations in patients with COPD were higher than those of control subjects. At stable conditions and exacerbations, the Hb-CO concentrations in patients at stage III were higher than those in patients at stage II, and the Hb-CO concentrations in patients at stage IV were also higher than those in patients at stage III. In patients at stage IV, the Hb-CO changes between stable conditions and exacerbations were higher than those in patients at stage III, and the Hb-CO changes in patients at stage III Yasuda, Yamaya, Nakayama, et al.: Carboxyhemoglobin in COPD were higher than those in patients at stage II. In patients with COPD at the exacerbations, Hb-CO concentrations also inversely correlated with FEV1 and arterial blood PaO2. At the exacerbations, FEV1 was less than 40% in all four patients with the Hb-CO concentrations of more than 1.4%, and FEV1 was less than 50% in all eight patients with Hb-CO concentrations of more than 1.2%. These findings suggest that measurement of Hb-CO may be a useful marker of severity, especially to define the severe exacerbations of COPD, although there is an overlap of the Hb-CO concentrations between control subjects and patients with COPD and between patients with COPD at stable conditions and exacerbations. The Hb-CO concentrations also correlated with serum values of CRP and LPO, suggesting that the Hb-CO concentrations might be also associated with the lung and airway inflammation and production of reactive oxygen species in the patients. Smoking history in control subjects differed from that in patients with COPD in the present study, although all control subjects and all patients with COPD were ex-smokers. To avoid the effects of ambient CO from smoking on Hb-CO and exhaled CO levels, we excluded current smokers by measuring urinary cotinine concentrations (41), and we confirmed that all subjects had not smoked for at least 3 months before the samplings. Furthermore, none of the control subjects and patients with COPD was a passive smoker. On the other hand, the Hb-CO concentrations in control subjects with a smoking history of more than 60 pack-years, which was the average smoking history of patients with COPD in this study, did not differ from the Hb-CO concentrations in the control subjects with a smoking history of less than 60 pack-years. These findings suggest that a different smoking history did not influence the Hb-CO in the control subjects. Increased Hb-CO in patients with COPD in this study is consistent with that observed in previous studies in patients with bronchial asthma, pneumonia, and interstitial lung disease (27, 28), in which increased Hb-CO might relate to the inflammation in airway and/or lung parenchyma. At stable conditions in this study, airway inflammation (5) and production of reactive oxygen species (15) might be associated with increased Hb-CO (23) in patients with COPD. Airway inflammation caused by infection of bacteria and viruses (10, 11, 25) might further increase endogenous CO production in patients with COPD at exacerbations. In patients with COPD at the exacerbations caused by bacterial and viral infections, PaO2 and FEV1 decrease and PaCO2 concentrations increase (10, 11). At the exacerbations in this study, 18 of 55 patients (31%) represented the symptoms of URTI, 13 patients (24%) had acute bronchitis with purulent sputum, and six patients (11%) had pneumonia. The Hb-CO concentrations might be increased through the production of proinflammatory cytokines and NO (9, 23, 42–44) in airway virus infection, and through reactive oxygen species (15, 23) from neutrophils (8) in bacterial infection. These factors might also relate to the increased CRP and LPO levels (45, 46). Systemic inflammation and production of reactive oxygen species in the organs, including muscles, have been reported in patients with COPD (30, 31). To examine the site of endogenous production of CO, we measured the a-v Hb-CO difference, which is a better way to define the site of inflammation, in the lung or other organs, in patients with bronchial asthma and pneumonia (28). In patients with COPD, the a-v Hb-CO differences at stable conditions and exacerbations did not differ from those in control subjects. Furthermore, among the patients with COPD at stable conditions, the a-v Hb-CO differences in patients were not increased in the severe stage of COPD. The loss of a-v Hb-CO differences in the patients in the present study suggests that CO might be also produced in organs other than the lung, such as 1249 muscles (30). On the other hand, Hb-CO inversely correlated with FEV1 in the patients at the exacerbations, suggesting that lung and airway might be also the site of CO production. The estimation of Hb-CO from exhaled CO measurements is suggested to be inaccurate in patients with severe airflow obstruction (47), and Hb-CO might be increased in patients with severe airflow obstruction because of reabsorption of CO (47). In fact, in patients with COPD at stage IV, exhaled CO concentrations at the exacerbations were lower than those at stable conditions. Therefore, we performed direct measurement of Hb-CO concentrations in the present study. Furthermore, increased exhaled CO concentrations were associated with increased Hb-CO concentrations in patients at the exacerbations in patients at stage II and stage III. These findings suggest that increased Hb-CO concentrations might represent the elevated endogenous CO production, although the influence of reabsorption of CO on Hb-CO was not excluded. We previously reported that arterial Hb-CO is correlated with FEV1 in asthma exacerbations (28). This study also demonstrated that the Hb-CO concentrations inversely correlated with FEV1 in patients with COPD. These findings suggest that airway narrowing might relate to the increased Hb-CO concentrations. However, many mechanisms have been reported to be associated with COPD exacerbations, including mucus hypersecretion, airway edema, and bronchoconstriction (48), all of which cause airway narrowing. On the other hand, CRP values in patients with COPD at exacerbations in this study were higher than those in patients with bronchial asthma in the previous study (27). The stronger inflammation in patients with COPD might be associated with the greater Hb-CO concentrations in patients with COPD compared with those in patients with bronchial asthma (11). However, we could not estimate the effect of bronchoconstriction on Hb-CO in this study, because we did not measure the changes in FEV1 after inhalation of anticholinergic drugs or -adrenergic stimulants. In the present study, Hb-CO concentrations in patients with COPD receiving inhaled corticosteroids did not differ from those in patients with COPD without inhalation of corticosteroids. Inhaled corticosteroids might fail to inhibit airway inflammation in these patients with severe COPD with frequent exacerbations, as demonstrated in patients with severe asthma (49). Exhaled CO levels are reported to be low in patients deficient in ␣1-antitrypsin (41). However, we did not examine the relationship between ␣1-antitrypsin levels and Hb-CO levels, because ␣1-antitrypsin deficiency in patients with COPD is very rare in the Japanese population (50). In summary, we have demonstrated that arterial Hb-CO concentrations increased in patients with COPD at a stable condition compared with those in normal control subjects. The Hb-CO concentrations at the exacerbations were significantly higher than those at stable conditions. The patients needed to stop breathing for 20 seconds to measure the exhaled CO concentrations. This procedure was difficult to repeat for the patients with COPD with severe dyspnea. The Hb-CO concentrations can be measured at the same time as the blood gas analysis, and should be measured first at a medical examination. The measurement of arterial Hb-CO concentration may be a simple and valuable marker to monitor the severity of systemic and lung inflammation and disease activities in patients with COPD. Conflict of Interest Statement : H.Y. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.Y. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; K.N. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; T.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.O. does 1250 AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE VOL 171 2005 not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; D.I. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.N. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; H.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. Acknowledgment : The authors thank Grant Crittenden for the English correction. References 1. Barnes PJ, Kleinert S. COPD—a neglected disease. Lancet 2004;364:564– 565. 2. Repine JE, Bast A, Lankhorst I. Oxidative stress in chronic obstructive pulmonary disease. Oxidative Stress Study Group. Am J Respir Crit Care Med 1997;156:341–357. 3. Pesci A, Balbi B, Majori M, Cacciani G, Bertacco S, Alciato P, Donner CF. Inflammatory cells and mediators in bronchial lavage of patients with chronic obstructive pulmonary disease. Eur Respir J 1998;12:380– 386. 4. Vernooy JH, Küçükaycan M, Jacobs JA, Chavannes NH, Buurman WA, Dentener MA, Wouters EF. Local and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:1218–1224. 5. Hogg JC, Chu F, Utokaparch S, Woods R, Elliott WM, Buzatu L, Cherniack RM, Rogers RM, Sciurba FC, Coxson HO, et al. The nature of small-airway obstruction in chronic obstructive pulmonary disease. N Engl J Med 2004;350:2645–2653. 6. Keatings VM, Collins PD, Scott DM, Barnes PJ. Differences in interleukin-8 and tumor necrosis factor-alpha in induced sputum from patients with chronic obstructive pulmonary disease or asthma. Am J Respir Crit Care Med 1996;153:530–534. 7. Boots AW, Haenen GR, Bast A. Oxidant metabolism in chronic obstructive pulmonary disease. Eur Respir J 2003;46:14S–27S. 8. Qui Y, Zhu J, Bandi V, Atmar RL, Hattotuwa K, Guntupalli KK, Jeffery PK. Biopsy neutrophilia, neutrophil chemokine and receptor gene expression in severe exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2003;168:968–975. 9. Terajima M, Yamaya M, Sekizawa K, Okinaga S, Suzuki T, Yamada N, Nakayama K, Ohrui T, Oshima T, Numazaki Y, et al. Rhinovirus infection of primary cultures of human tracheal epithelium: role of ICAM-1 and IL-1. Am J Physiol 1997;273:L749–L759. 10. Sethi S. New developments in the pathogenesis of acute exacerbations of chronic obstructive pulmonary disease. Curr Opin Infect Dis 2004;17: 113–119. 11. Seemungal T, Harper-Owen R, Bhowmik A, Moric I, Sanderson G, Message S, Maccallum P, Meade TW, Jeffries DJ, Johnston SL, et al. Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001;164:1618–1623. 12. Maziak W, Loukides S, Culpitt S, Sullivan P, Kharitonov SA, Barnes PJ. Exhaled nitric oxide in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:998–1002. 13. Ansarin K, Chatkin JM, Ferreira IM, Gutierrez CA, Zamel N, Chapman KR. Exhaled nitric oxide in chronic obstructive pulmonary disease: relationship to pulmonary function. Eur Respir J 2001;17:934–938. 14. Rahman I, van Schadewijk AA, Crowther AJ, Hiemstra PS, Stolk J, MacNee W, De Boer WI. 4-Hydroxy-2-nonenal, a specific lipid peroxidation product, is elevated in lungs of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:490–495. 15. Dekhuijzen PN, Aben KK, Dekker I, Aarts LP, Wielders PL, Van Herwaarden CL, Bast A. Increased exhalation of hydrogen peroxide in patients with stable and unstable chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1996;154:813–816. 16. Paredi P, Kharitonov SA, Leak D, Ward S, Cramer D, Barnes PJ. Exhaled ethane, a marker of lipid peroxidation, is elevated in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000;162:369–373. 17. Santus P, Sola A, Carlucci P, Fumagalli F, Di Gennaro A, Mondoni M, Carnini C, Centanni S, Sala A. Lipid peroxidation and 5-lipoxygenase activity in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;171:838–843. 18. Yamada N, Yamaya M, Okinaga S, Lie R, Suzuki T, Nakayama K, Takeda A, Yamaguchi T, Itoyama Y, Sekizawa K, et al. Protective effects of heme oxygenase-1 against oxidant-induced injury in the cultured human tracheal epithelium. Am J Respir Cell Mol Biol 1999;21:428–435. 19. Otterbein L, Sylvester SL, Choi AMK. Hemoglobin provides protection against lethal endotoxemia in rats: the role of heme oxygenase-1. Am J Respir Cell Mol Biol 1995;13:595–601. 20. Horváth I, Donnelly LE, Kiss A, Paredi P, Kharitonov SA, Barnes PJ. Raised levels of exhaled carbon monoxide are associated with an increased expression of heme oxygenase-1 in airway macrophages in asthma: a new marker of oxidative stress. Thorax 1998;53:668–672. 21. Jarvis MJ, Russell MAH, Saloojee Y. Expired air carbon monoxide: a simple breath test of tobacco smoke intake. BMJ 1980;281:484–485. 22. Zayasu K, Sekizawa K, Okinaga S, Yamaya M, Ohrui T, Sasaki H. Increased carbon monoxide in exhaled air of asthmatic patients. Am J Respir Crit Care Med 1997;156:1140–1143. 23. Mines MD. The heme oxygenase system: a regulator of second messenger gases. Annu Rev Pharmacol Toxicol 1997;37:517–554. 24. Horváth I, Loukides S, Wodehouse T, Kharitonov SA, Cole PJ, Barnes PJ. Increased levels of exhaled carbon monoxide in bronchiectasis: a new marker of oxidative stress. Thorax 1998;53:867–887. 25. Yamaya M, Sekizawa K, Ishizuka S, Monma M, Mizuta K, Sasaki H. Increased carbon monoxide in exhaled air of subjects with upper respiratory tract infections. Am J Respir Crit Care Med 1998;158:311–314. 26. Monma M, Yamaya M, Sekizawa K, Ikeda K, Suzuki N, Kikuchi T, Takasasa T, Sasaki H. Increased carbon monoxide in exhaled air of patients with seasonal allergic rhinitis. Clin Exp Allergy 1999;29:1537– 1541. 27. Yasuda H, Yamaya M, Yanai M, Ohrui T, Sasaki H. Increased carboxyhaemoglobin concentrations in inflammatory diseases. Thorax 2002;57: 779–783. 28. Yasuda H, Sasaki T, Yamaya M, Ebihara S, Maruyama M, Kanda A, Sasaki H. Increased arteriovenous carboxyhemoglobin differences in patients with inflammatory pulmonary diseases. Chest 2004;125:2160– 2168. 29. Yasuda H, Ebihara S, Yamaya M, Masito Y, Nakamura M, Sasaki H. Increased arterial carboxyhemoglobin concentrations in elderly patients with silicosis. J Am Geriatr Soc 2004;52:1403–1404. 30. Ribera F, N’Guessan B, Zoll J, Fortin D, Serrurier B, Mettauer B, Bigard X, Ventura-Clapier R, Lampert E. Mitochondrial electron transport chain function is enhanced in inspiratory muscles of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2003;167:873–879. 31. Sin DD, Lacy P, York E, Man SF. Effects of fluticasone on systemic markers of inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004;170:760–765. 32. Yasuda H, Yamaya M, Shinkawa M, Ebihara S, Sasaki H. Increased arterial carboxyhemoglobin concentrations in patients with chronic obstructive pulmonary diseases [abstract]. Am J Respir Crit Care Med 2003;167:A232. 33. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. NHLBI/WHO workshop report. Bethesda, MD: National Heart, Lung and Blood Institute; April 2001. Update of the Management Sections, GOLD website (www.goldcopd.com). Updated: 1 July 2003. 34. Turner BB, Wecker MT, Pohl G, Witek TJ, McNally E, St. George R, Winther B, Hayden FG. Efficacy of tremacamra, a soluble intercellular adhesion molecule 1, for experimental rhinovirus infection. JAMA 1999;281:1797–1804. 35. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987;106:196–204. 36. Hariharan M, VanNoord T, Greden JF. A high-performance liquidchromatographic method for routine simultaneous determination of nicotine and cotinine in plasma. Clin Chem 1988;34:724–729. 37. Ewing GW. Instrumental methods of chemical analysis, 3rd ed. [international student ed.]. New York and Tokyo: McGraw-Hill/Kogakuska; 1969. pp. 48–1 and 48–5. 38. Yamaya M, Sekizawa K, Ishizuka S, Monma M, Sasaki H. Exhaled carbon monoxide levels during treatment of acute asthma. Eur Respir J 1999;13:757–760. 39. Girotti AW. Mechanism of lipid peroxidation. J Free Radic Biol Med 1985;1:87–95. 40. Yagi K. Assay for blood plasma or serum. Methods Enzymol 1984; 105:328–331. 41. Henderson FW, Reid HF, Morris R, Wang OL, Hu PC, Helms PW, Forehand L, Mumford J, Lewtas J, Haley NJ, et al. Home air nicotine levels and urinary cotinine excretion in preschool children. Am Rev Respir Dis 1989;140:197–201. 42. de Gouw HW, Grunberg K, Schot R, Kroes AC, Dick EC, Sterk PJ. Yasuda, Yamaya, Nakayama, et al.: Carboxyhemoglobin in COPD 43. 44. 45. 46. Relationship between exhaled nitric oxide and airway hyperresponsiveness following experimental rhinovirus infection in asthmatic subjects. Eur Respir J 1998;11:126–132. Cantoni L, Rossi C, Rizzardini M, Gadina M, Ghezzi P. Interleukin-1 and tumour necrosis factor induce hepatic heme oxygenase: feedback regulation by glucocorticoids. Biochem J 1991;279:891–894. Kim YM, Bergonia HA, Muller C, Pitt BR, Watkins WD, Lancaster JR Jr. Loss and degradation of enzyme-bound heme induced by cellular nitric oxide synthesis. J Biol Chem 1995;270:5710–5713. Akira S, Hirano T, Taga T, Kishimoto T. Biology of multifunctional cytokines: IL 6 and related molecules (IL 1 and TNF). FASEB J 1990;4:2860–2867. Girotti AW. Lipid hydroperoxide generation, turnover, and effector action in biological systems. J Lipid Res 1998;39:1529–1542. 1251 47. Togores B, Bosch M, Augusti AG. The measurement of exhaled carbon monoxide is influenced by airflow obstruction. Eur Respir J 2000;15: 177–180. 48. Wedzicha JA, Donaldson GC. Exacerbations of chronic obstructive pulmonary disease. Respir Care 2003;48:1204–1213. 49. Yamaya M, Hosoda M, Ishizuka S, Monma M, Matsui T, Suzuki T, Sekizawa K, Sasaki H. Relation between exhaled carbon monoxide levels and clinical severity of asthma. Clin Exp Allergy 2001;31:417– 422. 50. Seyama K, Nukiwa T, Souma S, Shimizu K, Kira S. Alpha 1-antitrypsindeficient variant Siiyama (Ser53[TCC] to Phe53[TTC]) is prevalent in Japan: status of alpha 1-antitrypsin deficiency in Japan. Am J Respir Crit Care Med 1995;152:2119–2126.