Pulmonary Arterial Enlargement And Acute Exacerbations of COPD
advertisement

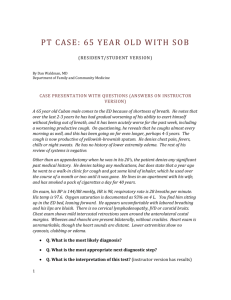
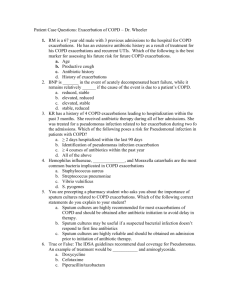
Presented by: MaCie Rogers Pharm.D Candidate 2013 • Accelerated loss of lung function and death are often associated with acute exacerbations of Chronic Obstructive Pulmonary Disease (COPD) • An acute exacerbation of COPD is defined as “an increase in dyspnea, cough, or sputum production warranting a change in therapy.” • Pulmonary hypertension is a major complication of COPD and can predict the occurrence of an acute exacerbation • Identifying patient’s at high risk of exacerbation would be paramount to improving quality of life and preserving lung function • Computed tomography (CT) can be used to measure the diameter of the pulmonary artery and the ratio of that diameter to the diameter of the aorta (PA:A ratio) • The authors of this study hypothesized that a PA:A ratio>1would be associated with a history of severe exacerbations of COPD and independently associated with an increased risk of future events • A multi-center observational trial including current and former smokers with COPD (the COPDGene Trial) • Inclusion criteria: 45 to 80 years old, current or former smoker with a history of 10 pack-years or more • Total enrollment: 10,300 participants, 3464 with Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage II to IV. Of these patients, 2985(86%) participated in a longitudinal follow-up study to prospectively track clinical course • 2005 participants from the ECLIPSE trial (a 3-year longitudinal study with the objective to identify surrogate endpoints associated with COPD exacerbations) were used as a validation cohort • Acute exacerbations were self-reported in both the COPDGene and the ECLIPSE studies, defined and quantified by answers to questions in a respiratory questionnaire • Severe and Mild-to-moderate exacerbations were differentiated by required hospital admission for treatment vs. outpatient treatment with antibiotics or systemic glucocorticoids • The occurrence and frequency of all exacerbations (mild-tomoderate and severe) were documented as secondary endpoints • More patients with PA:A ratio >1reported a severe exacerbation in the year before enrollment. (53% vs. 13%; Odds ratio, 7.44; 95% CI, 6.23 to 8.89; P<.001) • The occurrence of severe exacerbations were also associated with increased pulmonary artery diameter, increased percentage of lung volume with emphysema on CT, and increased gas trapping on CT • Severe exacerbations were shown to be independently associated with younger age, lower FEV1 scores, higher SGRQ scores, and PA:A ratio >1 • At enrollment (OR 4.78; 95% CI, 3.43-6.65; P<0.001), • During longitudinal follow-up (OR 3.44; 95% CI, 2.784.25; P<0.001) • Associations with age and presence of GERD were no longer significant during follow-up A PA:A ratio >1(as detected through CT) is associated with future exacerbations of COPD, especially those requiring hospitalization and therefore can be used to identify a subpopulation at high risk for hospitalization • Limitation: This is an observational study and therefore the conclusion that PA:A ratio elevations cause acute exacerbations of COPD cannot be definitively drawn. • Strength: Agreement of findings with the external validation, ECLIPSE trial, cohort significantly strengthen the results • Wells MJ, Washko GR, MeiLan HK, et al. Pulmonary Arterial Enlargement and Acute Exacerbations of COPD. N Eng J Med 2012;367(10); 913-921