Get connected with Electronic Data Interchange (EDI)
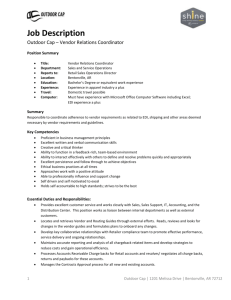
advertisement

What is EDI? Electronic Data Interchange (EDI) allows providers to submit and receive electronic transactions from their computer systems. EDI is available for most common health care business transactions, such as claims processing, electronic remittance advices, claims status, eligibility inquiries, and automated claims payments. Contacting an EDI Specialist For more information about electronic claims filing, electronic remittance advice, eligibility benefit inquiry, claim status and other transactions, call an Anthem EDI specialist for details. Our specialists can address questions regarding registration, testing and the implementation process. Providers can visit our website and view the Anthem Companion Guide for specific instructions on filing transactions electronically. The site is also the link to EDI registration, announcements and electronic submission information. Get connected with Electronic Data Interchange (EDI) Advantages of Submitting Claims Electronically Reduces inefficiencies associated with paper claims processing and speeds claims processing. }} Accelerates payments. }} Front-end editing results in cleaner claims. }} Reduces administrative costs when compared to paper claims. }} Live Chat Session Produces daily reports, providing an audit trail and claim status. }} Live Chat is an instant messaging service where EDI Solutions specialists are available to answer questions from our customers. Getting Connected Providers have two options for electronic filing or submission: Direct Submission Providers can use their internal programming staff or purchase vendor software to enhance their existing systems to meet the Health Insurance Portability and Accountability Act (HIPAA) and Anthem data format and quality standards. }} A copy of the EDI Companion Guide is available at anthem.com/edi (select state) and may be downloaded to assist with direct connection set-up. }} Once the testing process is completed with Anthem, providers can begin electronic claim submissions without a charge from Anthem. }} Clearinghouse/EDI Vendor Approach Providers contract with an EDI vendor or clearinghouse who may charge a fee for data formatting and routing services. }} For more information, visit our website at anthem.com/edi. The clearinghouse will edit, format and transmit electronic transactions to the appropriate insurance company. }} Anthem works directly with clearinghouses and EDI vendors to ensure that our formatting and quality standards have been satisfied. }} A current list of approved clearinghouses is available at anthem.com/edi (select state). }} In Connecticut: Anthem Blue Cross and Blue Shield is the trade name for Anthem Health Plans, Inc. In Maine: Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Maine, Inc. In New Hampshire: Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of New Hampshire, Inc. Independent licensees of the Blue Cross and Blue Shield Association. ® ANTHEM is a registered trademark. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association. PLNBR0756A Rev. 10/10 Five Easy Steps to Electronic Connectivity Select a submission approach. }} Install/test submission approach. }} Register/test with EDI Solutions. }} Train office staff. }} Begin electronic submissions to Anthem. }} Electronic Remittance Advice (ERA) Take Advantage of Automated Remittance Posting Anthem offers electronic delivery of remittance advices. The remittance advice provides information for the payee regarding claims in their final status. The content on the remittance advice meets HIPAA requirements, containing nationally recognized HIPAA-compliant remark codes used by Medicare and other payers like Anthem. Benefits of Electronic Remittance Advices Reduces accounts receivable errors and administrative costs. }} Provides prompt delivery of electronic remittance advices to providers — usually before paper copies arrive. }} We encourage providers to contact their electronic vendors and clearinghouses to learn more about additional options available for ERA such as: Manual and automated posting options. }} Single easy-to-read, printer friendly format for multiple payers. }} Electronic Funds Transfer (EFT) EFT is secure, efficient process for directly depositing payments into the providers’ bank accounts. Providers have immediate access to funds. Real Time Electronic Transactions Many health care organizations, including health care partners, payers, clearinghouses, software vendors and fiscal intermediaries offer electronic solutions as a fast, inexpensive and secure method of automating business processes. Anthem has electronic and web solutions, giving providers access to patient insurance information before or at the time of service, using the system of their choice. Advantages Allows providers to perform online transactions. }} Provides coverage verification before services are provided. }} Collect copayments at the time of service. }} Streamlines claim management and reduces payer calls. Easy access to payer Explanation of Benefits (EOBs). Automated coordination of benefit claims filing. }} Capability to quickly locate documents for research and customer service. }} }} }} Image retrieval, eliminating loss of misfiled documents. }} Support and staff training. }} Please download the ERA enrollment form from anthem.com/edi. Reduces rejections and denials due to eligibility errors. Provides mechanisms to automatically track claim status and correct patient information for future claims submission. Register at Anthem Online Provider Services Online Web Portal Web-based transaction system for health care partners. Participants with Anthem can easily and quickly access pertinent patient information. }} To learn more about enrollment, password resets and available features, contact your support representative at 866-755-2680. }} Please download theEFT enrollment form from anthem.com/edi. }} }} Many health care organizations, including health care partners, payers, vendors and fiscal intermediaries choose EDI as a fast, inexpensive and secure method of automating their business processes. Features 270/271 Health Care Eligibility Benefit Inquiry and Response – This “real time” transaction provides information on patient eligibility, coverage verification, and patient liability (deductible, copayment, coinsurance). }} To learn more about enrollment, cost and available features, please contact the EDI Solutions Helpdesk at 800-334-8262 or visit our website at anthem.com/edi. 276/277 Health Care Claim Status Request and Response – Also real time, this transaction indicates whether an electronic claim has been paid, denied or in progress. }} Getting Connected Providers can access these HIPAA compliant transactions: Clearinghouse or EDI software vendor Clearinghouses and EDI vendors often have easyto-use web and automated solutions to verify information for multiple payers simultaneously through one portal in a consistent format. }} Contact your EDI software vendor or clearinghouse to learn more about options available. }} For connectivity options and file specifications our Anthem EDI Companion Guide is available at anthem.com/edi. }} Contact (EDI Specialist): EDI HELP DESK Hours available: 8:00 a.m. - 4:30 p.m. ET Telephone: 800-334-8262 Web address: anthem.com/edi E-mail address: edi-ne@anthem.com