GI II: Small Intestine, Large Intestine, Salivary Glands, Pancreas, Liver
advertisement

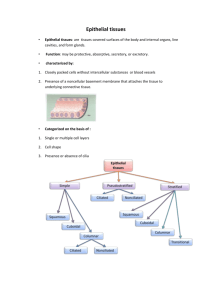
GI II: Small Intestine, Large Intestine, Salivary Glands, Pancreas, Liver Small Intestine Anatomic Three parts: 1) duodenum 2) jejunum 3) ileum Cross section: Ross p.441 (See below) Mucosa Submucosa Components: 1) epithelium: simple columnar 2) lamina propria a) inflammatory cells: macrophages and mast cells – stain pink on PAS b) lacteals: lymphatic capillaries used in fat absorption 3) muscularis mucosae: two thin layers of smooth muscle cells Crypts of Lieberkuhn = intestinal gland: simple tubular structures which extend from m. mucosae to base of villi (empty into lumen) Ross p.485 Fig. 1 Dense CT (many cells), arteries, veins, lymphatics, Meissner’s plexus Functional Surface area maximized for digestion and absorption: 1) plicae circularis: luminal folds with submucosal core 2) villi: mucosal projections with lamina propria core 3) microvilli: cellular appendages of actin filaments Cell types: 1) Enterocytes: absorptive function and secretion of digestive enzymes 2) Goblet cells: secrete mucus; white on H&E 3) Paneth cells: found at base of crypts of Lieb.; contain apical acidophilic granules and secrete lysozyme and other antibacterial products 4) Enteroendocrine cells: also in the crypts; secrete CCK, GIP, secretin; stain with Bodian silver (look granular) 5) M cells: found over Peyer’s patches; phagocytose macromolecules and unload them into the lymphatic nodules below In duodenum submucosa contains Brunner’s glands: 1) alkaline secretions to protect duodenum from gastric acid 2) good way to distinguish stomach from duodenum at the junction Muscularis externa Serosa Large Intestine Recto-Anal Junction 1) Inner circular smooth muscle layer: segmental contractions 2) Outer longitudinal layer: propulsion of contents forward (peristalsis) A layer of simple squamous epithelium (mesothelium) and some underlying dense irregular CT 1) Smooth mucosal surface: NO plicae or villi 2) Teniae coli: 3 bands formed by longitudinal layer of muscularis externa 3) Many goblet cells, increasing number as you progress distally 4) Crypts with goblet cells and regenerative cells Simple columnar → stratified columnar → stratified squamous keratinized 1) Internal anal sphincter: circular smooth muscle 2) External anal sphincter: striated muscle of perineum Auerbach’s plexus: part of the enteric nervous system; found in between the two muscularis externa layers It’s equivalent to visceral peritoneum GALT (gut-associated lymphatic tissue) well developed for handling microorganisms and noxious metabolic and other products Plexus of veins in submucosa of rectum can become hemorrhoidal with portal hypertension Anatomic Salivary Glands Parotid gland Sublingual gland Functional Acinus: May contain serous, mucus or basic secretory unit of the both types of cells: salivary gland; looks like a 1) serous cells: RER and bunch of grapes ribosomes basally (blue), secretory Ducts: granules apically 1) Intercalated ducts: (pink) cuboidal epithelium; 2) mucus cells: granules absorb Cl- secrete HCO3 lost in H&E preps 2) Striated ducts 3) mixed acini: serous (intralobular ducts): more demilunes – mucus columnar; absorb Na+ cell with a serous cap secrete K+; render primary secretion hypotonic; nucleus found in central position 3) Excretory ducts (interlobar ducts): Parotid and Submandibular ducts; located within large CT septa; no modification of secretions 1) Purely serous 2) Striated ducts and adipose tissue helps to distinguish it from pancreas 1) Mixed gland 2) More heterogenous than the parotid Pancreas Liver 1) Exocrine component: serous gland; secretes inactive enzymes into duodenum necessary for digestion (ex: trypsinogen) 2) Endocrine component: secretes into blood insulin and glucagon (Islets of Langerhans – useful landmark to distinguish pancreas) -- The duct system of the pancreas begins with the oval, pale, centroacinar cell unique to pancreas “Classic lobule” organization (Ross p. 498 diagram) 1) Hexagon with central vein in the center 2) Each corner has a portal triad: a) hepatic artery (thick wall) b) portal vein (thin wall, irreg. shape) c) bile duct (lymph also drains from liver around portal “triad” area) 3) Each lobule is filled with hepatocytes and sinusoids (sinusoids perfuse cells with mixed portal and arterial blood) Bile canaliculi are formed by apposition of two hepatocytes Canaliculi → canals of Hering → bile ducts (interlobular) Bile ducts are lined by simple cuboidal epithelium that gradually becomes columnar -- Zymogens (inactive enzymes) are located in acidophilic secretory vesicles in apical part of cell. -- Basal parts of cell: basophilic due to RER, ribosomes -- CCK secreted by enteroendocrine cells induces zymogen release -- Intercalated ducts secrete bicarbonate and respond to secretin “Liver acinus” organization emphasizes function – Three zones: -- hepatocytes of Zone 1, closest to periphery of classic lobule, get most oxygenated blood -- in Zone 3, closest to central vein, hepatocytes get least oxygenated blood → has significance for liver pathology (ex: in hypoperfusion of the liver Zone 3 affected first) Space of Disse: lies b/w the basal surface of hepatocytes and endothelial and Kupffer cells that line sinusoids – exchange of materials b/w blood and liver cells Kupffer cells: macrophages found in sinusoidal space; participate in destroying senescent RBCs