Vascular Surgery

Vascular Surgery
Angie Allen, ACNP
Stacey Becker, RN
Objectives
5.
6.
7.
8.
9.
3.
4.
1.
2.
Identify our team.
Peripheral Artery Disease
Cerebral Revascularization
Lower Extremity Revascularization
Lower Extremity Amputation
Abdominal Aortic Aneurysms (endovascular)
Thoracic Aortic Aneurysms (endovascular)
Abdominal Aortic Aneurysms (open)
Thoracic Outlet
Who are we?
Attendings
Dr. Thomas Naslund-
Division Chief
Dr. Raul Guzman
Who are We?
Attendings Continued
Dr. Jeff Dattilo
Dr. Colleen Brophy
Who are we?
Fellows
Dr. Ali Khoobehi
Dr. Syed Rizvi
Interns:
Carry the consult/resident pager:
831-6374
Who are we?
Nurse Practitioner
Angie Allen, ACNP-BC
First Call for Vascular
M-F 0730-1600
886-0163 (cell)
835-8202 (pager)
Who are we?
Case Management
Stacey Becker, RN (Dr. Naslund)
Ann Luther, RN
Social Worker
Ann Lacy, RN
Other Numbers
Vascular Office: 322-2343
Vascular Clinic: 936-7485
Vascular Lab: 343-9561
Arterial Disease
Peripheral Artery Disease (PAD): leading case of death worldwide. Polyvascular disease.
Atherosclerosis: Most likely the cause of PAD. Hardening of the artery or loss of elasticity.
Arterial Pathophysiology:
1. Occlusive disease: Atherosclerosis is symptomatic by gradually occluding the artery to the target organ or extremity. (kidneys, colon, legs, or arms)
2. Symptoms occur with critical arterial stenosis (75 % of cross sectional of lumen is obliterated)
Arterial Disease
Aneurysmal Disease: occurs due to loss of structural integrity of vessel wall. Over time this will result in dilation and aneurysm formation.
Cerebral Revascularization
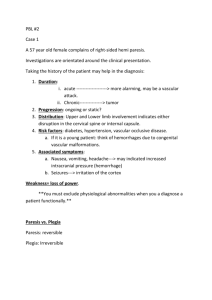
Symptomatic: Patients who have carotid stenosis or occlusion that have exhibited a
CVA or TIA
Asymptomatic: Patients who have carotid stenosis or occlusion that are high risk for CVA
(i.e. hypertension, hyperlipidemia, smoker, obesity, CAD, etc.)
Symptoms
Right sided symptoms:
-Left hemiplegia or monoparesis and right eye visual loss
Left sided symptoms:
-Right hemiplegia or monoparesis and left eye visual loss
-aphasia
Symptoms
Visual symptoms are due to ischemia of the retina.
Amaurosis fugax
-Transient visual loss
-”Window shade”, “flashing lights”, or
“sparks”
Cerebral Revascularization
Surgical Intervention
Carotid Endarterectomy
Or
Carotid Artery Stenting
Carotid Endarterectomy
Carotid Artery Stenting
Cerebral Revascularization
Post Operative Care
Neuro Assessment: VERY IMPORTANT. Essential for recognizing neurological deficits.
Contralateral hemiparesis: technical problem with endarterectomy with immediate return to OR. Notify team ASAP. Arterial duplex may be ordered.
Defuse neurological deficit: possible internal capsule stroke secondary to hypotensive episode.
Delayed neurological deficit: 12-24 hours postoperatively. Arterial Duplex with possible CTA of head and neck for evaluation of brain hemorrhage or CVA and evaluation of carotid.
Post Operative Care
Continued
Dextran 40: instituted for antiplatelet purposes and may be continued for 24 hours postoperatively.
NPO until POD 1 for possible exploration.
D5 ½ NS while patient is NPO
POD 1: Initiation of Plavix 75 mg subcutaneous daily
(if no concerns for hematoma)
Incision: Leave dressing dry and intact until POD 1, may remove. Incision will be closed with disolvable sutures, leave open to air unless draining.
Cerebral Revascularization
Complications
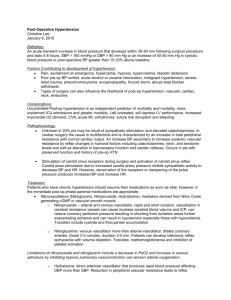
Hypertension: 20 % of patients. SBP 100-140
Neck Hematoma: May compromise breathing and swallowing.
-May require immediate surgical intervention for evacuation
-Order tracheostomy kit Stat to the bedside
Local Nerve Injuries: Most common laryngeal and hypoglossal nerves presenting as temporary weakness in speech, swallowing, tongue or lip movement. Less than 0.5% result in permanent damage.
Hyperperfusion Syndrome: 1-2 % occur 3-7 days post operatively. Headache, Seizures, and Intracranial
Hemorrhage. Hypertension may accompany. Supportive management
Cerebral Vascularization
Discharge Instructions
Incision Care: Leave open to air, unless draining. Wash with antibacterial soap and water and use white wash cloths.
Immediately call 911 with patient has headache with associated decreased level of consciousness or seizure activities.
Follow up in Vascular Clinic 4 weeks postoperatively.
Discharge Medications: Plavix and pain medication
Plavix injection education.
Activity: Do not resume normal work activities until follow up apt. No driving until that time, do not return to work.
(?????)
Lower Extremity Revascularization
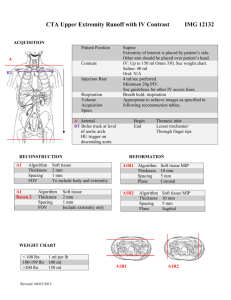
Anatomy
Lower Extremity Vascular Disease
Symptoms
Claudication: pain at rest, present with ambulation.
Typically seen one level below the disease.
Critical Ischemia: Rest pain may be first symptoms of severe ischemia. Sharp, localized pain to forefoot to below the ankle, dependent rubor and pallor with elevation. 95% loose limb in 1 yr without revascularization.
Critical Ischemia: Non healing ulcers. (arterial vs venous)
Critical Ischemia-Gangrene: Skin and subcutaneous tissue involvement. Dry (noninfected black eschar) vs Wet (macerated, purulent drainage).
Gangrene-Dry
Symptoms Continued
Microemboli: Blue Toe Syndrome causes blue, mottled spots over the toes. May be painful.
Acute Arterial Ischemia: Sudden onset of extremity pain, pallor, paresthesia, pulselessness, and poikilothermia. Caused by stenotic artery or emboli if no previous vascular disease.
TREATMENT
Treatment is based on duration, disability, progression, general medical condition, non-invasive diagnostic testing AND pathology
Non-op management: walking program, lifestyle modification, with possible medication.
Diagnostic Testing: Arterial duplex with segmental pressures/ABI’s (vascular lab), CTA or MRA, arteriogram, plain films, ECG (if ischemic toes-could be from a-fib), PT /PTT/INR/Platelet workup.
Operative Managment
Percutaneous transluminal angioplasty/stenting
Femoropopliteal or Pop-DP, etc. bypass
(saphenous vein, Dakron, ePTFE)
Femoropopliteal percutaneous endovascular intervention
Aortoiliac or Aortobifemoral bypass or angioplasty with or without stenting
Thromboembolectomy
Amputation
Post-Operative Care
ICU stabilization after aortic operations
(stability of vitals/hemodynamics, respiratory, fluid, electrolyte, cardiac, laboratory -pcv, blood glucose, lytes, coags- management).
Fluids: D51/2 NS 20 KCL at 75 mL/hr
Rewarm and vasodilate: bolus may be warranted
Post op day 3-4: mobilization of fluids-may see lasix given.
Post-Operative Care Continued
Pain Control: essential for mobilization. PCA or percocet or lortab
Ambulation: PT/OT consult, POD 1
Rooke Perioperative Boots
Antibiotics: continued for 24 hours
Wound Care: remove dressing POD 1, may leave open to air unless draining. Wash with antibacterial soap and water and use white wash cloths.
Amputation Wounds: Takedown is on POD 2, will require knee immobilizer.
High Risk for Pressure Ulcers
Complications
Hemorrhage from graft: Exploration required.
Thrombis (graft occlusion) PULSES< PULSES<PULSES
Infection
Stage 1: Involving skin and dermis-wound care, antibiotics.
Stage 2: Extending to subcutaneous and fatty tissue but not graft-Exploration and washout in the OR, continued wound care and antibiotics.
Stage 3: Graft involvement-Exploration and washout in the OR with graft removal with establishment of new route of perfusion. Continued wound care and 6 weeks of IV antibiotics.
Complications Continued
Compartment Syndrome: Caused by prolonged ischemia (> 6 hrs) then revascularization resulting in edema in the calf muscles. Leg pain with sensory deficits to the dorsum of the foot and weakness of toe dorsiflexion. Measure Compartment Pressure.
Treatment: fasciotomy.