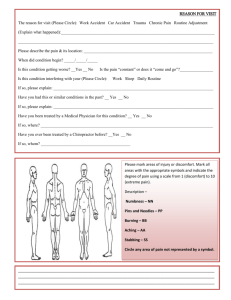
0 = no pain 10 = worst pain ever
advertisement
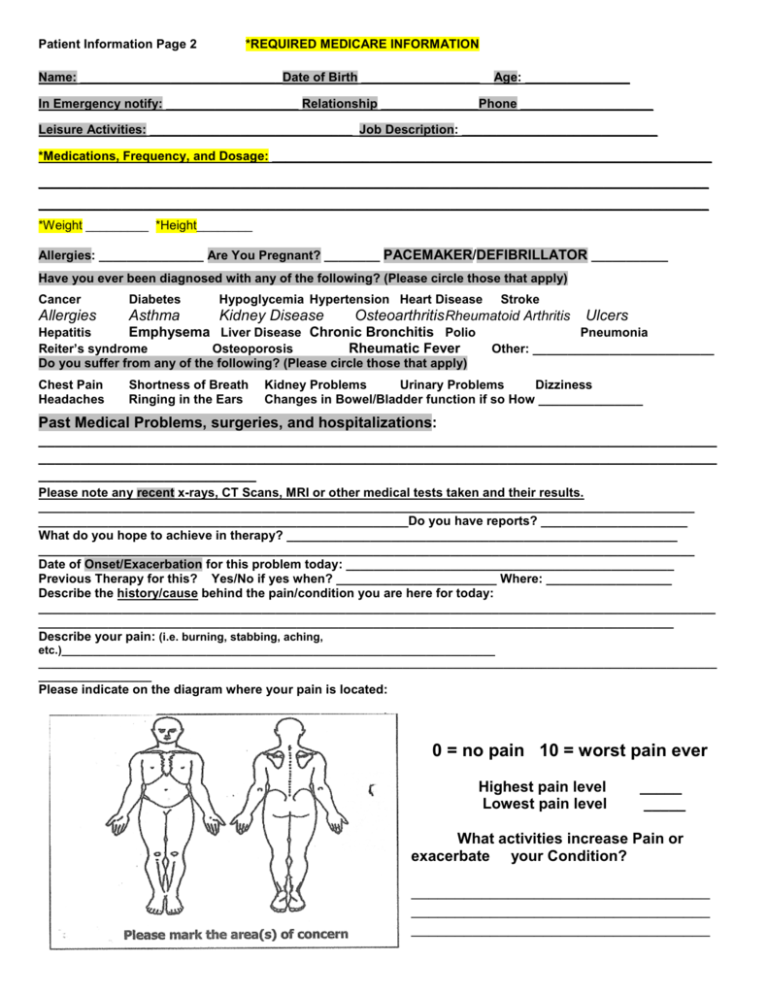
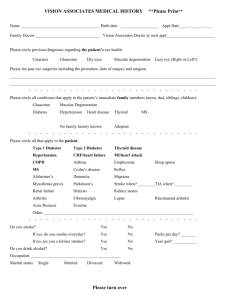
Patient Information Page 2 *REQUIRED MEDICARE INFORMATION Name: _____________________________Date of Birth _________________ Age: _______________ In Emergency notify: ___________________ Relationship ______________Phone ___________________ Leisure Activities: _____________________________ Job Description: ____________________________ *Medications, Frequency, and Dosage: _______________________________________________________________ ________________________________________________________________________________________________ ________________________________________________________________________________________________ *Weight _________ *Height________ Allergies: _______________ Are You Pregnant? ________ PACEMAKER/DEFIBRILLATOR ___________ Have you ever been diagnosed with any of the following? (Please circle those that apply) Cancer Diabetes Hypoglycemia Hypertension Heart Disease Allergies Asthma Kidney Disease Hepatitis Emphysema Liver Disease Chronic Bronchitis Polio Rheumatic Fever Reiter’s syndrome Osteoporosis Do you suffer from any of the following? (Please circle those that apply) Chest Pain Headaches Shortness of Breath Ringing in the Ears Stroke Osteoarthritis Rheumatoid Arthritis Ulcers Pneumonia Other: __________________________ Kidney Problems Urinary Problems Dizziness Changes in Bowel/Bladder function if so How _______________ Past Medical Problems, surgeries, and hospitalizations: _________________________________________________________________________________ _________________________________________________________________________________ __________________________ Please note any recent x-rays, CT Scans, MRI or other medical tests taken and their results. ______________________________________________________________________________________________ _____________________________________________________Do you have reports? _____________________ What do you hope to achieve in therapy? ________________________________________________________ ______________________________________________________________________________________________ Date of Onset/Exacerbation for this problem today: _______________________________________________ Previous Therapy for this? Yes/No if yes when? _______________________ Where: __________________ Describe the history/cause behind the pain/condition you are here for today: _________________________________________________________________________________________________ ___________________________________________________________________________________________ Describe your pain: (i.e. burning, stabbing, aching, etc.)_____________________________________________________________________ ____________________________________________________________________________________________________________ __________________ Please indicate on the diagram where your pain is located: 0 = no pain 10 = worst pain ever Highest pain level Lowest pain level _____ _____ What activities increase Pain or exacerbate your Condition? __________________________________ __________________________________ __________________________________