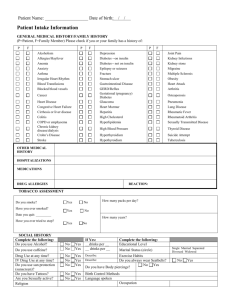
Review of Systems: Please circle all that apply.
advertisement
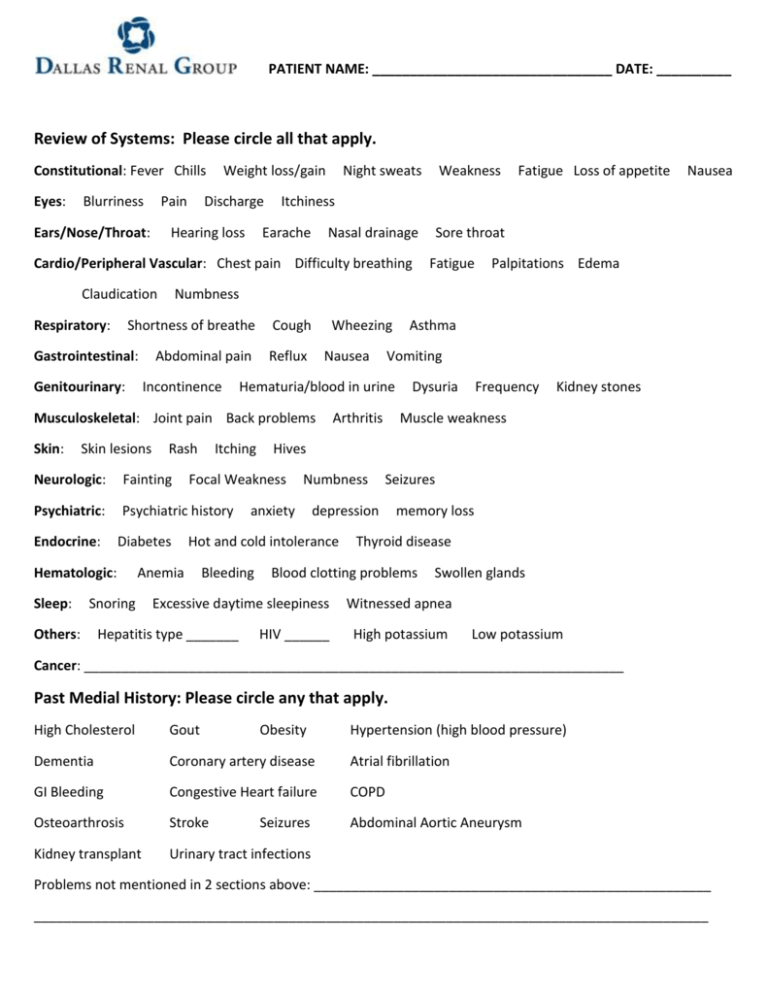
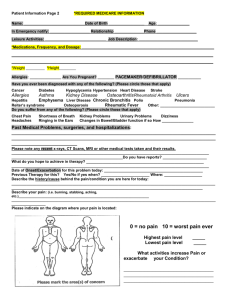
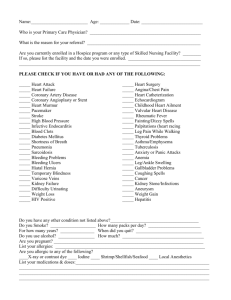
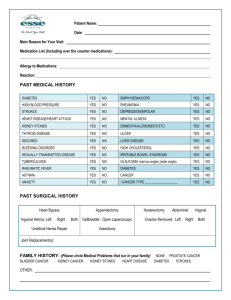
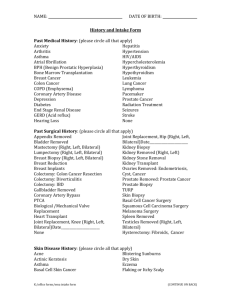
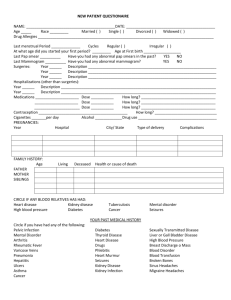
PATIENT NAME: ________________________________ DATE: __________ Review of Systems: Please circle all that apply. Constitutional: Fever Chills Eyes: Blurriness Pain Ears/Nose/Throat: Weight loss/gain Discharge Hearing loss Night sweats Weakness Nasal drainage Sore throat Respiratory: Earache Genitourinary: Abdominal pain Incontinence Cough Wheezing Reflux Nausea Skin lesions Rash Itching Neurologic: Fainting Psychiatric: Psychiatric history Endocrine: Diabetes Hematologic: Sleep: Others: Arthritis Numbness anxiety Frequency Kidney stones Seizures memory loss Thyroid disease Blood clotting problems Excessive daytime sleepiness Hepatitis type _______ Dysuria Muscle weakness depression Hot and cold intolerance Bleeding Asthma Hives Focal Weakness Anemia Snoring Palpitations Edema Vomiting Hematuria/blood in urine Musculoskeletal: Joint pain Back problems Skin: Fatigue Numbness Shortness of breathe Gastrointestinal: Nausea Itchiness Cardio/Peripheral Vascular: Chest pain Difficulty breathing Claudication Fatigue Loss of appetite HIV ______ Swollen glands Witnessed apnea High potassium Low potassium Cancer: ________________________________________________________________________ Past Medial History: Please circle any that apply. High Cholesterol Gout Obesity Dementia Coronary artery disease Atrial fibrillation GI Bleeding Congestive Heart failure COPD Osteoarthrosis Stroke Abdominal Aortic Aneurysm Kidney transplant Urinary tract infections Seizures Hypertension (high blood pressure) Problems not mentioned in 2 sections above: _____________________________________________________ __________________________________________________________________________________________ Page 2 PATIENT NAME: ______________________________ DATE: __________________ Check any surgeries and list year. __Appendectomy ______ ___Kidney biopsy _______ ___Tonsillectomy______ ___Prostate _______ __Gallbladder ______ ___Hysterectomy _______ ___Pacemaker________ __Breast biopsy ______ ___Mastectomy ______ ___Coronary artery bypass _________ ___Other: _______________________________________________________________________________ Family History: please list family member and disease. Kidney disease: ___________________________________________________________________________ Diabetes: ________________________________________________________________________________ Hypertension: ____________________________________________________________________________ Heart disease: ____________________________________________________________________________ Cancer: _________________________________________________________________________________ Other: __________________________________________________________________________________ Social History: please circle and list explanation. Marital Status: Employed: Married Full-time Single Divorced Part-time Separated Partnered Spouse deceased Retired Current or Previous Occupation: _______________________ Education: High school diploma Tobacco use: Non-smoker Alcohol use: None Drug use: Never GED Some College College graduate Previous Smoker Smoker per day: 1-9 Occasional 10-19 20-39 40+ Everyday: ______________________________________ Previous: ____________________ Current: ________________________ Caffeine consumption: Never Some Cups per day: _____ Filled out by: ___________________________________ Relationship: __________________