EVALUATION OF THE HORSE WITH COLIC WHEN AND HOW TO
advertisement

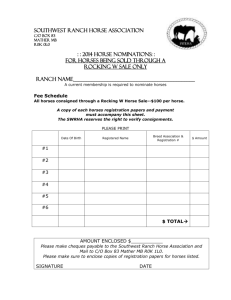
EVALUATION OF THE HORSE WITH COLIC WHEN AND HOW TO REFER? Joanne Hardy, DVM, PhD, Diplomate ACVS, The Ohio State University Colic is the number one cause of death in horses. In our hospital, 60% of emergencies are colics. Over the years, medical and surgical outcome of horses with colics has gradually improved, partly due to improved therapies, but more importantly, early recognition of patients requiring aggressive medical or surgical intervention. Colic refers to the presence of abdominal pain, which can result from gastrointestinal or non-gastrointestinal disorders, and can sometimes be mimicked by extra-abdominal pain. Examples of extra-abdominal disorders that can present as colic include rhabdomyolysis, pleuritis, and CNS diseases. Disorders of abdominal organs other than the GI tract can manifest as colic, and may include liver disease (cholelithiasis) or urogenital disorders such as uterine or testicular torsion, impending abortion, ovarian disease and urolithiasis. The specific cause of colic may not be identified on physical examination, and is not required in order to decide for the need for referral, surgical intervention, or aggressive cardiovascular support. History will often provide an insight into the possible cause of colic, but the clinician must rely on a thorough physical examination, repeated as the horse’s condition is changing, to decide on appropriate intervention. The physical examination of a colicky horse identifies three related areas that require the clinician’s attention: 1) Evaluation and management of pain; 2) Evaluation of the cardiovascular status; 3) Evaluation of the gastrointestinal tract. History A good and pertinent history is essential in the evaluation of a colicky horse. There are specific breed, gender, age and management conditions affecting the equine gastrointestinal tract. Arabians are at increased risk for enterolithiasis, particularly in the South and Western regions of the country. Miniature horses are at increased risk for small colon impactions. Standardbred and Belgian horses have an increased incidence of inguinal hernias. Broodmares with a foal at foot are commonly affected with large colon displacement/torsion. Late gestation mares are at risk for uterine torsion, whereas post-partum mares may suffer from middle uterine rupture or small colon mesenteric avulsion. Stallions are at risk for inguinal hernias. Gastrointestinal disorders affecting foals can include meconium impaction, enterocolitis, atresia coli, ruptured bladder, intussusception, ascarid impaction and volvulus nodosus. In older horses, small intestinal strangulating obstructions are commonly caused by strangulating lipomas or epiploic foramen entrapment. Older horses with poor dentition are at risk for impaction. Management practices should be inquired. Colic in general is more frequent in the performance horse. Horses receiving little hay in their diet, particularly if bedded on sawdust, are at risk for ileal impaction. Gas colic is frequently observed in show animals, and these colics can lead to large colon displacements. Horses that are regularly exercised in a swimming pool often suffer from gas colic. Large strongyle infestation is less common, but horses wormed exclusively with ivermectin or moxidectin are at risk for tapeworm infestation, if they have access to pasture. Horses bedded on sand or having access to a sandy paddock can develop sand colic. Overweight ponies, Miniature horses and Miniature donkeys are at risk for development of hyperlipemia when fasted because of colic. Past medical or surgical history as well as insurance status, vaccination and current medication should be obtained. A colic template form is useful for medical record keeping, particularly if the problem is recurrent. Evaluation and Management of Pain Abdominal pain results from distention of hollow organs (stomach, small intestine, and large colon), mesenteric stretching, or stretching of the parietal peritoneum. Of all parameters used in deciding for surgery (pain, nasogastric reflux, abnormal rectal exam, abnormal abdominocentesis, elevated heart rate), pain is the only criteria that stands alone in deciding for surgery. Horses suffering from abdominal pain only without cardiovascular deterioration will rarely have heart rates over 60 BPM. The initial management of pain includes 1) pain relief, if possible, by passing the nasogastric tube or trocarization of the large colon; 2) controlling the pain to enable an initial exam to be performed. The ideal drug to use should result in minimal CV compromise; provide temporary relief until an assessment is reached; have a rapid onset of action. Alpha-2 agonists such as xylazine and detomidine are well suited for these goals. The onset of action of both drugs is rapid (1-2 minutes). Xylazine will provide analgesia for 15-20 minutes IV, or about 40 minutes IM. Detomidine will last for 60 minutes and should be reserved for cases unresponsive to xylazine. Butorphanol can be given with xylazine to provide additional analgesia with minimal cardiovascular compromise. NSAID are commonly used for the management of colic in horses. Common NSAID in decreasing order of efficacy for abdominal pain are flunixin, ketoprofen, and phenylbutazone. Aspirin is not used because its half-life is very short in the horse. Flunixin is the most effective NSAID for the management of visceral pain. Its onset of action is approximately 15 to 20 minutes, and response will lasts about 4 to 6 hours. The dose range varies from 0.25 to 1.1 mg/kg, and the analgesia is dose dependent up until the higher dose range. Flunixin is also efficacious at the lower dose to counter the negative effects of endotoxin (hypotension) on the cardiovascular system. There is no advantage in giving more than the maximal dose, and there is increased risk of GI and renal toxicity, particularly in a dehydrated animal. Acepromazine is not an analgesic, and has the potential for hypotension in dehydrated or highly stressed animals. In horses with a known cause of GI disease, where longterm pain management with minimal side effects is desired, we have used a lidocaine infusion. When combined with other analgesics, lidocaine has a synergistic effect, and by interrupting the intestinal reflex arc, can promote GI motility. Pain should be monitored: response to nasogastric decompression or trocarization may provide an insight to the initiating cause of pain. Recurrence of pain after the mediation wears off can help obtain a differential and may indicate the need for referral or surgical intervention. Cardiovascular Status The circulatory status of the horse should be evaluated next, and if shock is present, should be treated immediately before continuing the exam. Circulatory status is evaluated by: HR, MM color, CRT, palpation of extremities, and complemented with PCV/TP. The heart rate of horses with little CV compromise remains below 60. As dehydration and/or endotoxemia evolve, the heart rate will gradually increase. Horses with heart rates over 80 BPM require immediate cardiovascular support. The volume of intestinal secretion in the horse on a daily basis is equivalent to the extracellular fluid volume (30% of body weight or, for a 400 kg horse, 120 liters!!!!). This explains the rapid dehydration and cardiovascular collapse of horses with small intestinal obstruction. Shock therapy in the horse includes administration of large volumes of fluids. If the heart rate is over 80, administration of 40 to 60 ml/kg in the first hour (16 to 24 liters of fluids) is recommended. Because fluid losses are usually isotonic, a balanced electrolyte solution (Lactated Ringers) is recommended. If fluid administration is not possible, referral is indicated. Examination of the Gastrointestinal Tract The elements of examination of the GI tract include auscultation, nasogastric intubation, rectal palpation, and abdominocentesis. Ancillary methods include; ultrasound, radiographs, and gastroscopy GI Auscultation The abdomen is divided into 4 quadrants corresponding to specific anatomical structures. In the upper left quadrant, referred sounds from the stomach or small intestine can be heard. Since transit time from stomach to caecum is approximately 2 hours, this quadrant can be quiet if the horse has been fasted. The lower left and lower right quadrants correspond to the large colon, and should normally constantly have motility. The upper right quadrant corresponds to the cecal base, which should have motility. Gas can also be pinged in that area. In addition to these 4 zones, the area behind the xyphoid can be auscultated for sand. Interpretation: Horses with impending enterocolitis will often have hypermotile gut sounds, with fluidy sounds and gas. In early obstructive disease, hypermotility can also be heard. Hypomotility or absent gut sounds indicate ileus or obstruction. The inability to hear sand does not rule out a sand impaction. Nasogastric intubation. A large bore tube should be used for this diagnostic procedure, and the tube should be primed with water and moved back and forth. Reflux is not present in the normal horse. Small amounts of reflux can be present with large colon disease if large colon distention exerts pressure on the duodenum. The onset of reflux is delayed in distal (ileal) small intestinal obstruction. Large amounts of reflux are characteristic of: late distal SI lesions or SI lesions including anterior enteritis and SI obstruction. The character of the reflux can be: normal GI contents, fermented or bloody. Typically, horses with anterior enteritis will have large amounts of foulsmelling reflux, which can sometimes be bloody. If reflux is obtained, medication should not be administered orally, and the tube needs to be left in place for transportation. Rectal palpation This procedure should be performed with caution in young, small or fractious horses. The presence and character of feces should be noted. Scant feces indicate ileus or obstruction. Feces with mucus are an indication of large colon stasis. Unformed, fibrous feces intermixed with blood are often seen with small colon impactions. Complete absence of feces on repeated exams may indicate a small colon obstruction. Of note that feces can still be passed with complete small intestinal obstruction. Palpation identifies the type of distention (gas, fluid or feces), the location (small intestine, large colon, small colon), and the location of the organs. Interpretation: Small intestinal distention: differentials include small intestinal obstruction (simple or strangulating) or ileus. If fluid therapy is unavailable, the horse should be referred with a stomach tube in place. Cecal distention: firm (impaction): cecal impaction: if aggressive fluid therapy not available the horse needs to be referred (cecal impaction can rupture without warning). Gas: cecal dilatation, which can be primary or secondary to a large colon displacement. Trocarization can be performed; if pain recurs, suspect a displacement. Large colon distention: firm and to the left: pelvic flexure impaction: treat with oral and IV fluids, superhydration, and laxatives. The impaction must be palpated carefully and differentiated from a right dorsal displacement of the large colon: if the impaction can be followed to the right of the abdomen, it is more likely to be a large colon displacement, which will not respond to medical therapy. Large colon gas distention: differentials include gas colic, displacement/torsion of the large colon, small colon obstruction. Some horses with impending colitis also show some abdominal pain and large colon distention with fluid or gas. Response to analgesics is important. Large colon torsions will be very painful and only show transient response. THESE NEED TO BE REFERRED IMMEDIATELY. Recurring pain after analgesics wear off: displacement or small colon obstruction likely. Small colon obstruction: If a total obstruction is present (enterolith or fecalith), typically, no feces are present in the rectum. The obstruction itself is rarely palpable, but is suggested by recurring pain and absence of feces. Small colon impaction: feces are very typical: not formed, mixed with blood. A long tubular structure without sacculations is palpated on rectal. Ancillary Diagnostic Methods: Ultrasonography, radiographs and gastroscopy are additional methods that can be used to arrive at a diagnosis. Ultrasound can be used to identify the presence of peritoneal effusion, peritonitis, small intestinal distention, intussusceptions, and nephrosplenic entrapment. Radiographs are useful in the adult to identify enteroliths or sand. In the foal radiographs and ultrasound are used instead of rectal palpation. Gastroscopy is useful for evaluation of gastric disorders, particularly ulcers. EVALUATION OF COLIC: WHEN IS REFERRAL INDICATED? Of all the elements of the physical exam, the number one prognostic indicator for survival is the cardiovascular status. Deterioration in cardiovascular parameters is a key indicator towards referral. Each element of the physical exam can provide an indication for referral: Pain Severe and unrelenting, or quickly recurring. Intermittent chronic pain. CV status Deterioration as indicated by increasing heart rate and poor color. NG intubation Large volume of reflux is an indication for rehydration, and is a sign of ileus or mechanical obstruction. Rectal palpation Small intestinal distention indicates the need for nasogastric intubation, if not already performed. Because of large volumes of fluid secreted in the GI tract daily, ileus or mechanical obstruction of the small intestine results in rapid dehydration. Large colon distention indicates gas colic, displacement or torsion, or aboral obstruction. This finding must be correlated with other physical exam finding and level of pain. Abdominocentesis The total protein will increase within one hour of a strangulating obstruction, followed by red blood cells within 3-4 hours, followed by WBC within 6 hours, as intestinal necrosis progresses. It is always better to refer before changes have taken place in the abdominocentesis, particularly before a significant elevation in WBC. Therefore, one should not wait until changes in the abdominocentesis have occurred. Furthermore, an abdominocentesis should not be performed if it will not alter the decision making process. Sequential evaluations can help identify a trend towards deterioration. Abdominocentesis is not helpful to differentiate between anterior enteritis and a small intestinal obstruction. Surviving horses with large colon torsion do not have time to develop changes in the abdominocentesis, and intervention needs to occur before any changes have occurred. In large colon torsion, an increased total protein is a poor prognostic indicator. HOW TO REFER? In preparing a colicky for referral, several things need to be considered: control of pain during transport, ongoing dehydration, and need for gastric decompression. It is always better to educate the client about referrals before the need occurs. Clients should be prepared by having a file of their horse’s medical history, insurance policy, and directions to the referral center. They also need to be informed of payment policies, to avoid unpleasant surprises. If it is a mare and foal that are transported, it is always wise to separate the foal particularly if the mare has colic, to avoid trauma to the foal. Control of pain If the pain is severe before sedation, it will probably recur when sedation wears off, so providing the owner with additional sedation I often needed during transportation. We will assume that flunixin (1.1 mg/kg, IV) has already been administered, and is not effective in controlling the pain. If the pain is severe, detomidine (0.02 mg/kg, IV, can be combined with IM for longer duration). Can be given just before loading the horse. If the pain is mild, xylazine (0.2 to 0.4 mg/kg IV, can be combined with IM) can be used. For long distance, a catheter should be placed, to allow the owner to administer additional sedation, if needed. It is better to not give the owner needles, but to put the medication in a capped syringe. If the owner were to accidentally prick him/herself with a needle from a xylazine loaded syringe, a fatal reaction could occur. Naso-gastric intubation A naso-gastric tube should be passed and secured in place, even if there is no reflux. This is particularly true for long distances, where fluid may start to accumulate in the stomach. The tube should be secured in place with tape, and for additional security, a muzzle can be placed on the horse’s nose. Fluid therapy If there is evidence of dehydration, fluids can be administered during transportation. The great majority of horses have isotonic dehydration so Lactated Ringers is the fluid of choice. If the horse is in shock, hypertonic saline (4 ml/kg, over 10 minutes) can be given, but should be followed with large volume isotonic fluids. Feed and water should be withheld during transportation. CONCLUSION The need for referral is not identified only when surgical intervention is required, but also any time cardiovascular support through the administration of large volumes of fluids is needed. Horses with severe large colon impaction can respond to medical treatment by superhydration with large volumes of intravenous fluids (60-80 liters a day). Horses with large volume of reflux require replacement fluid therapy, even if a medical condition such as anterior enteritis is diagnosed. Referral may also be indicated for additional diagnostic procedures. Gastroscopy is the gold standard for evaluation of the equine stomach. Ultrasonography or abdominal radiography may provide additional information as to the cause of the colic. Biopsy of liver, kidney or palpable masses may be indicated. Laparoscopy or flank laparotomy provide minimally invasive techniques to explore the abdomen, particularly when the cost of a ventral midline precludes that approach, when the horse’s general condition is poor, or when the need for a complete exploratory has not been confirmed. In conclusion, a thorough history and physical examination are key in the approach of the horse with abdominal pain. Physical examination can dictate initial intervention such as referral, cardiovascular support or surgery, even if a specific diagnosis is not reached. Referral facilities can provide additional diagnostic tools and intensive care management of horses with colic, and are highly dependent on the initial work-up provided by the practitioner for timely and appropriate referral.