RESPIRATORY notes
advertisement

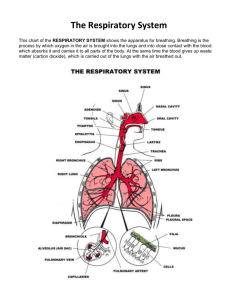
RESPIRATORY SYSTEM The respiratory system functions to exchange gases between the blood and the external environment. Using blood as a transporting fluid, the cardiovascular system organs transport respiratory gases between the lungs and the tissue cells. If either system fails, body cells begin to die from oxygen starvation and accumulation of carbon dioxide. Nose – The nasal cavity is divided by the nasal septum and is lined with ciliated mucosa. Olfactory receptors for smell are located in the mucosa. The internal mucosa lining moistens and warms the inhaled air. Mucus traps inhaled foreign particles and contains lysozyme enzymes which destroy the inhaled bacteria. Cilia move the mucus toward the pharynx, where it is swallowed and digested. Mucosa-covered projections called conchae increase the surface area exposed to air. Paranasal sinuses surround the nasal cavity and act as resonance chambers for speech. Pharynx (throat) – is lined with mucous membranes and is a muscular pathway for food and air to enter. Pharynx is divided into the nasopharynx, oropharynx, and laryngopharynx. The Eustachian tube opens into the nasopharynx. The tonsils are located in the upper region of the pharynx. Larynx (voice box) – superior part of trachea lined with mucous that routes air and food into proper channels. It contains vocal cords, fibrous bands, which vibrate with expelled air to produce sound. The larynx contains rigid hyaline cartilages and a flap of elastic cartilage called the epiglottis. The thyroid cartilage is the largest of the hyaline and protrudes forming the “Adam’s apple”. The epiglottis protects the superior opening of the larynx. When swallowing, the epiglottis closes off the trachea so food enters the esophagus. Trachea (windpipe) – is reinforced with C-shaped rings of hyaline cartilage to support this passageway for air. The passageway is lined with ciliated mucosa to trap and propel foreign debris. Bronchi – the trachea branches into the right and left primary bronchi which run obliquely before entering the medial depression (hilum) of each lung. The right main bronchus is wider, shorter and straighter than the left which makes it easier for inhaled objects to become lodged. Smaller subdivisions of the bronchi are within the lungs and direct air towards the alveoli (air sacs). These bronchi continue to divide forming a bronchial tree and ending in the smallest conducting passageway called bronchioles. The terminal bronchioles lead into the respiratory bronchioles into alveoli ducts which feed air to the alveoli sacs/alveoli. Alveoli - The alveoli walls contain elastic fibers and simple squamous epithelium. The external surface is covered with pulmonary capillaries where gas exchange occurs between the alveoli and the blood. Roughly 600 million alveoli are located in the lungs. They contain alveolar macrophages to engulf bacteria and other debris. The cuboidal cells in the alveolar walls produce surfactant which coats the surfaces to prevent the alveoli from collapsing and reduce surface tension from the air. Lungs – found in the thoracic cavity. The superior apex is deep to the clavicle and the inferior base rest on the diaphragm. The diaphragm muscle contracts and relaxes to alter the volume of the chest cavity. Each lung is divided into fissures --- left lung has 2 lobes and a cardiac notch and the right lung has 3 lobes. The surface of the lung is covered with visceral pleura and the walls of the thoracic cavity are lined with parietal pleura. Pleural fluid in the pleural space allows the lungs to move during breathing without friction. o o Atelectasis – lungs collapse resulting from air entering the pleural space; usually associated with a chest wound Pleurisy – inflammation of the pleural space. PHYSIOLOGY – to supply the body with O2 and dispose of CO2 these four events must occur: 1. Pulmonary Ventilation – air moves into and out of the lungs in the alveoli (breathing) 2. External Respiration – gas exchange between the pulmonary capillaries and the alveoli 3. Respiratory Gas Transport - O2 is transported in the hemoglobin and CO2 is transported in the bicarbonate ion (HCO3-) in the plasma 4. Internal Respiration – gas exchange between capillaries and tissue Mechanisms of Breathing Inspiration – diaphragm and external intercostals contract increasing the size of the thoracic cavity. As intrapulmonary volume increase, gases within the lungs spread out to fill the space causing a decrease in pressure in the lungs. The decrease in pressure produces a partial vacuum which sucks air into the lungs. Air continues to move into the lungs until the intrapulmonary pressure equals atmospheric pressure. Expiration – inspiratory muscles relax, the rib cage descends and the lungs recoil. As the intrapulmonary volume decreases, the gases inside the lungs are forced more closely together, and the intrapulmonary pressure rises above atmospheric pressure. This increase in pressure causes gases to flow out to equalize the pressure inside and outside the lungs. The normal pressure within the pleural space is intrapleural pressure, is always negative, and is the major factor preventing collapse of the lungs. If intrapleural pressure becomes equal to atmospheric pressure, the lungs immediately recoil completely and collapse. Nonrespiratory air movements – reflex activities such as coughing, sneezing, crying, laughing, hiccups, yawning Respiratory Volumes & Capacities Tidal volume (TV) – amount of air in a normal breath (500 ml) Inspiratory reserve volume (IRV) – amount of air that can be taken in forcibly over the TV Expiratory reserve volume (ERV) – amount of air that can be forcibly exhaled after TV Residual volume – amount of air that remains in the lungs that can NOT be voluntarily expelled (1200 ml); Residual air allows gas exchange to go on continuously and keep the alveoli inflated Vital capacity (4800 ml) – sum of TV+IRV+ ERV ….. Vital capacity varies with age, gender, and physical condition. Measuring VC gives a device for diagnosis of disorders and judging effectiveness of treatment. Dead space volume (150 ml) – air that remains in conducting pathway of tract & never reaches alveoli Control of Respiration – activity of diaphragm and external intercostals is regulated by nerve impulses transmitted by the phrenic & intercostal nerves. Neural centers in the pons and medulla oblongata control respiratory rhythm and depth. Homeostatic Imbalances o Asthma – chronically inflamed and hypersensitive bronchial passages lead to spasms of bronchioles o Apnea – cessation of respiration o Dyspnea – labored breathing o Eupnea – normal breathing rate o Hyperpnea – breathing more vigorously o Bronchitis – mucosa become severely inflamed and produce excessive amounts of mucus o Emphysema – alveoli enlarge and chronic inflammation promotes fibrosis of the lungs. Lungs lose elasticity and airways collapse.