Aortic Valve Disease: Evaluation of insufficiency
advertisement

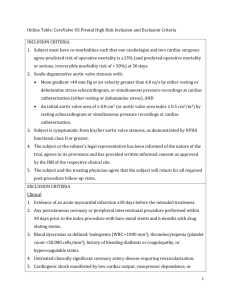
Aortic Insufficiency Lori Heller, MD Swedish Heart and Vascular Institute Swedish Medical Center Acting Instructor, University of Washington Seattle, WA Aortic Valve Anatomy ME SAX view of the aortic valve and its location in the center of the heart The aortic valve is a semilunar trileaflet valve with three symmetric cusps of similar size. Each cusp has a small fibrous nodule at the center of the coaptation edge called the node of Arantius. The plain of the aortic valve is oblique with the right posterior side angled inferiorly. The aortic leaflets attach from the ventricular wall (yellow arrows) to the STJ (red dotted line). This area makes up the aortic root. The aortic valve is contained within the aortic root which extends from the basal attachment of the leaflets within the LV to the distal attachment of the leaflets at the sinotubular junction. The root provides the supporting structures for the leaflets of the aortic valve and forms the bridge between the LV and the ascending aorta. The tips of the aortic leaflets protrude into the lumen of the aorta. The three cusps of the valve are named according to their relationship to the coronary arteries: the left cusp adjacent to the left coronary artery, the right cusp adjacent to the right coronary artery. The third cusp is not associated with a coronary artery and is therefore called the non-coronary cusp. At the mid portion of the aortic root are the three sinuses of Valsalva which are outpouchings directly behind each cusp. They serve to absorb some of the stress associated within the high pressure system as well as facilitate the smooth closing of the aortic valve and provide a reservoir of blood for coronary blood flow during diastole. Each sinus is associated with an aortic cusp, two of which are associated with coronary arteries. The coronary arteries originate from the center of the superior aspects of the sinuses just below the STJ. Etiology of Aortic Insufficiency The two major causes of isolated AR are conditions affecting primarily the valve and conditions affecting the aorta and secondarily causing valve incompetence. Leaflet Damage Bicuspid Valve Endocarditis Rheumatic Valve Disease Traumatic Rupture Failed Surgical Valve Balloon Valvulotomy Rheumatoid Arthritis Aortic Abnormalities/Dilation Aortic Root Dissection Connective Tissue Disorders (Marfan, Ehlers-Danlos) Hypertension Annuloaortic ectasia Ankylosing Spondylitis OsteogenesisImperfecta Syphilitic Aortitis The most common cause of isolated AR is now aortic root dilation. 1,3,4 This is vastly different than before 1980 when the majority of AR was post-inflammatory, generally related to the effects from rheumatic fever.2 In a single center review of 268 adults referred for aortic valve replacement for isolated AR United States for aortic valve replacement between 1993 and 2005, 46% of the patients’ AR resulted from a problem with the leaflets.3 The most common was a congenital bicuspid valve (unaffected by endocarditis), followed by endocarditis, 33% of whom had a bicuspid valve. Thus for those with valvular conditions causing AR, 61% had a bicuspid valve. In this study, the majority of known causes of isolated AR was the consequence of a condition affecting the ascending aorta: dissection was the most common, followed by Marfan’s syndrome and aortitis. Interestingly in a third of all of the cases, the cause of the AR was not determined. Those with an undetermined etiology were the oldest group and the majority (91%) had hypertension, suggesting that altered elasticity and/or geometry of the aortic root may have been the cause of valve incompetence. Systemic hypertension is thought to play a role in aortic dilation through wall stress as well as contributing to cystic medial necrosis in the elderly.17 There is also evidence that many patients with a bicuspid aortic valve have disorders of the connective tissue which can result in aortic dilation. The aortic expansion rate is higher in patients with bicuspid valves than in patients with tricuspid valves. 5 Most commonly, however, aortic insufficiency occurs in conjunction with aortic stenosis and is secondary to degenerative (senile) calcification. In one study of 236 surgically excised valves at the Mayo clinic, 46% of the combined insufficiency and stenosis was secondary to degenerative calcification. Bicuspid and post-inflammatory etiologies (17% each), post-therapeutic (13%), and indeterminate (8%) etiologies made up the rest. Chronic V. Acute Aortic Regurgitation In general, about 20% of AR is acute, the remainder is chronic. Acute AR is almost entirely due to endocarditis or acute aortic dissection. Different physiologic parameters are present in acute v. chronic AR due to the lack of adaptation of LV compliance.6,7 Chronic Bicuspid Valve, Hypertension Dilated Normal Wide Flat Etiology LV size LVEDP Pulse Pressure CW Doppler Slope Acute Endocarditis, Aortic Dissection Normal Elevated Narrow Steep Evaluation The evaluation of aortic insufficiency is accomplished by 4 echocardiographic methods: 2 D inspection Color Flow Doppler CW PW Doppler 2D Imaging 2 D inspection is used to evaluate the etiology of the regurgitation. AR may be due to either abnormalities of either the leaflets or the aortic root. Using the SAX and LAX views, the aortic valve leaflets are inspected for poor coaptation and other abnormalities and the root is examined for changes that would alter the geometry of the structures supporting the leaflets. Leaflet prolapse, perforations, bicuspid valves and annular dilation SAX of AV in end diastole. Leaflets are unable to coaptcompletly due to healing vegetation are all diagnosed from 2D imaging. Leaflet prolapse is identified on the RCC when any portion of the leaflet extends past the annular plane into the LVOT. Regurgitation from endocarditis can be caused by either leaflet perforation or from vegetation(s) causing improper leaflet closure. LAX view of aorta showing a measurement of the annulus, and effacement of the sinotubular junction (arrow) in a patient with Marfan Syndrome Annular dilation, by preventing complete leaflet coaptation, also causes aortic regurgitation and may be secondary to hypertension, connective tissue disorders (Marfan syndrome), or cystic medial necrosis. Marfan syndrome is characterized by effacement of the sinotubular junction with dilation of the annulus as well as the sinuses of Valsalva. In contrast, cystic medial necrosis usually has an identifiable STJ. Less common causes of aortic annulus dilation are syphilitic aortitis and osteogenesis imperfecta.5 The disease processes that cause aortic stenosis (bicuspid valve, rheumatic and calcific disease) also may result in aortic insufficiency. This is due to changes in the flexibility and/or shape of the valve resulting in poor coaptation of the leaflets. Associated 2D findings Chronic left ventricular volume overload from aortic regurgitation results in progressive dilation of the ventricle. The LV shape becomes more spherical. Systolic function is initially able to be maintained, ME 4 ch – dilated, spherical LV however over time LV performance declines and the changes can be irreversible. In contrast, acute AI does not result in LV dilation, however without the compensatory dilation, more symptoms may be appreciated. 7 Indirect 2D and M-Mode findings If the regurgitant jet impinges on the anterior leaflet of the mitral valve, it can cause impaired mitral leaflet opening. This results in an increased distance between the maximal anterior motion of the mitral valve in early diastole (the E point) and the most posterior motion of the interventricular septum. This is referred to as increased E point septal separation (normal is < 6 mm). Increased E point separation is also seen in LV dysfunction. Eccentric AR jet directed toward the anterior mitral valve leaflet A discrete area of curvature of the anterior mitral valve leaflet into the left atrium secondary to the pressure from the regurgitant jet may also be seen. This is termed “reversed doming” since the direction of curvature is opposite to that seen in rheumatic mitral stenosis. A raised fibrotic lesion on either the anterior leaflet or the septum may develop in chronic AI, due to the flow abnormalities. This can be visualized as a brighter area on 2D imaging. In addition, high frequency fluttering of the anterior mitral valve leaflet may also be seen on M mode but rarely appreciated on 2D imaging due to the difference in sampling rate. This is the equivalent of the Austin-Flint murmur. 8 . Reverse doming of the AML resulting from an eccentric AR jet Indirect Signs of Aortic Regurgitation Increased E point-septal separation (> 6mm) High Frequency fluttering of AMVL “Reverse doming” of the AMVL Jet lesion on septum or AMVL Color Flow Doppler M-mode of the mitral valve, demonstrating high-frequency diastolic fluttering of the anterior mitral leaflet due to severe AR COLOR FLOW DOPPLER CFD can be applied in both the AV SAX and the AV LAX view to evaluate the aortic valve. If color Doppler cannot be applied to the LVOT from the ME AV LAX view because of annular calcification or shadowing of the LVOT from a prosthetic mitral or aortic valve, a deep TG LAX or TG LAX view is used. Standard technique is to use a Nyquist limit of 50–60 cm/s, and a color gain that just eliminates random color speckle from non-moving regions. Typically, a central jet implies dilation of the annulus and an eccentric jet indicates a leaflet abnormality. The regurgitant jet flow has three components that can be visualized in the AV LAX view: the flow convergence in the aorta, the vena contracta through the regurgitant orifice and the jet direction and size in the LVOT. Vena Contracta Flow Convergence LVOT jet JET WIDTH/LVOT RATIO The width of the jet in the LVOT and its ratio to the diameter of the LVOT is one indication of AR severity. The jet should be measured just below the valve and within 1 cm of the valve. A central jet that takes up greater than 65% (or 2/3) of the LVOT is graded as severe.9, 10, 11 Jet width LVOT width 10 Jet Width to LV ratio Central Jet* Mild Moderate Severe < 25% LVOT 25-65% LVOT > 65% LVOT *At Nyquist limit of 50-60 cm/s There are important limitations to CF imaging of the regurgitant jet. If the jet is not uniform or have parallel borders in the LV outflow, it can be difficult to know where to measure it. Eccentric jets often appear narrow and their severity can be underestimated. Conversely, central jets tend to expand fully in the LVOT and may be overestimated. In addition, diffuse jets that arise from the entire coaptation line are difficult to measure. This type of jet can be suspected and identified from the SAX view. In addition, the size of the jet will depend on hemodynamic conditions. 18, 19 Of note, the length of the jet into the LVOT is not a reliable method for determining severity. 9 VENA CONTRACTA LA Vena Contracta AO LV RV The Vena Contracta is defined as the smallest portion of the jet at the level of the aortic valve, immediately below the flow convergence region. It is different from the jet width (measured in the LVOT, BELOW the aortic valve). The VC will be significantly smaller than that of the jet width because the jet expands immediately after the VC. The VC is an estimation of the Regurgitant Orifice Area. The size of the vena contracta is independent of flow rate and driving pressure for a fixed orifice and has been shown to correlate well with angiographic findings as well as accuracy with eccentric jets. It is much less load and SVR dependent than measurement of CFD jet width. A VC of 0.6 is consistent with severe AI. 10, 11, 12 Vena Contracta* Mild Moderate < 0.3 mm 0.3-0.6 mm *At Nyquist limit of 50-60 cm/s Severe > 0.6 mm 10 Continuous Wave Doppler Jet Intensity and Duration AR flow Aortic systolic flow CW tracing in the deep TG view displaying an aortic regurgitant density nearly equal to that of the aortic forward flow, which can indicate moderate to severe AI The spectral recording of AI begins at aortic valve closure with a rapid increase in velocity to a maximum of 3-5 m/s, followed by a gradual decline in velocity during diastole. An easy screening evaluation of the AI severity is to compare the intensity of the regurgitant signal to that of the antegrade signal. The density of the signal reflects the volume of regurgitation, therefore intensity of the regurgitant signal that matches or is close to the intensity of the antegrade signal can indicate moderate to severe AI. A faint spectral display is compatible with trace or mild AR. The intensity is also related to the direction of the jet relative to the ultrasound beam and therefore can sometimes be misleading. This should be considered a qualitative measure and recognized as not as accurate as others. 13, 14 To obtain the CW profile, the deep transgastic LAX or the transgastic LAX view can be used. Color Doppler can localize the jet and assure proper placement of the Doppler curser. Additionally, in moderate or severe regurgitation, the signal can easily be recorded throughout diastole, whereas mild AR may not appear holodiastolic, with a recordable signal only at the beginning or end of diastole. SLOPE Slope of AI jet obtained in TG LAX view. > 3 m/sec = severe The shape of the CW Doppler spectral profile depends on the timevarying instantaneous pressure gradient across the valve in diastole. The slope of the wave profile therefore can reflect the severity of the regurgitation since a larger regurgitant orifice allows for more rapid equilibration of pressures between the aorta and the LV. As a result, in severe AI, the slope of the spectral profile will be steeper. A regurgitant velocity slope greater than 3 m/sec is consistent with severe AI. 13, 14 Pressure Half Time Pressure Half Time is the time required for the peak pressure to reach one half of its maximum value and is used as another measurement of the rate of pressure equilibration. With the steeper slope that is seen in severe AI, the PHT is shorter. A PHT of 500 ms is consistent with mild AI whereas a PHT of 200 ms is considered severe AR. 13,14 Peak Pressure ½ Peak Pressure PHT = Time required to reach ½ peak pressure 10 Mild <2 >500 Slope m/s PHT ms Moderate 2-3 500-200 Severe >3 < 200 It should be noted that in acute AR, even if only moderate, a significant increase in end diastolic pressure can be seen due to the lack of LV compliance. The LV has not yet adapted, as it has in chronic AR, therefore the slope may be quite steep. Similarly, any other factors that affect LV diastolic pressure (ischemia, systolic dysfunction) or aortic pressure (sepsis, patent ductus, vasodilators) will result in more rapid equilibration of pressures and a steeper slope (and an inaccurate/increased grading of the AR). Another limitation of this method is seen in eccentric jets. Precise placement of the CW Doppler may be difficult with these jets and can be unreliable. Pulsed-Wave Doppler Flow Calculations Regurgitant fractions and orifice areas can be calculated using the continuity equation. 11, 15 The Aortic Regurgitant Volume is the difference between the forward stroke volume across the LVOT and the stroke volume across the mitral or pulmonic Valve (provided there is no significant MR or intracardiac shunt). Aortic Regurgitant Volume= AV Systolic Forward Volume- PV Volume (or MV volume) Volume = CSA x VTI PV flow = PV area x PV VTI Severe > 60 cc/beat MV flow = MV area x MV VTI To determine stroke volume across the PV, measure the PA diameter and determine the area by 2π(d/2)2. Obtain the TVI by placing CW through the PV (at the ME ascending aorta SAX view). Similarly, measure the diameter of the LVOT and determine the area by 2π(d/2)2. Multiply this by the AV VTI obtained in the deep transgastric view of the LV. Once Aortic Regurgitant Volume is determined, Regurgitant Fraction and Effective Regurgitant Orifice Area (ERO) can also be calculated: Regurgitant Fraction = Aortic Regurgitant Volumex 100 % LVOT Stroke Volume Severe > 50% Effective Regurgitant Orifice Area (ERO) = Aortic Regurgitant Volume Aortic Regurgitant TVI Severe > .30 cm2 10 Regurgitant Volume cc/min Regurgitant Fraction % EROA cm2 Mild < 30 < 30 < 0.1 Moderate 30-59 30-49 0.1-0.29 Aortic Diastolic Flow Reversal Regurgitant flow reversal in the descending aorta that lasts throughout the diastolic period is often a sign of significant AR. Brief diastolic flow reversal is normal, however with increasing severity of aortic regurgitation both the duration and the velocity of the flow increase. Holodiastolic flow reversal is usually indicative of at least moderate AR. One limitation to this measure is that the reduced aortic compliance seen with advancing age may also result in reversal of the diastolic flow. Severe 60 cc/min >50 > 0.3 Caudad Cephalad Desc LAX view of the aorta Pulsed Doppler obtained in the thoracoabdominal aorta showing flow reversal throughout diastole From: ACC/AHA 2006 Practice Guidelines for the Management of Patients With Valvular Heart Disease: Executive Summary 10JACC Vol. 48, No. 3, 2006 Bonow et al. 605 August 1, 2006:598–675ACC/AHA PRACTICE GUIDELINES—EXECUTIVE SUMMARY References 1. 2 3 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Dare AJ , Veinot JP, Edwards WD, Tazelaar HD, Schaff HVHum Pathol. 1993 Dec;24(12):1330-8. New observations on the etiology of aortic valve disease: a surgical pathologic study of 236 cases from 1990. Olson LJ , Subramanian R , Edwards WD . Surgical pathology of pure aortic insufficiency: a study of 225 cases . Mayo ClinProc . 1984;59:835–841 Roberts WC, Jong MK, Moore TR, Jones WH. Circulation. Causes of pure aortic regurgitation in patients having isolated aortic valve replacement at a single US tertiary hospital (1993 to 2005). Circulation. 2006; 114: 422-429 William CR, Jong M Some observations on mitral and aortic valve disease Proc (BaylUniv Med Cent) 2008;21(3):282– 299. Luc Cozijnsen, Richard L. Braam, Reinier A. Waalewijn, Marc A.A.M. Schepens, Bart L. What Is New in Dilatation of the Ascending Aorta? : Review of Current Literature and Practical Advice for the Cardiologist Circulation. 2011;123:924928 Tift Mann, M.D., McLaurin, L, Grossman W, Craige, E. Assessing the Hemodynamic Severity of Acute Aortic Regurgitation Due to Infective Endocarditis. N Engl J Med 293:108-113 July 1975 Karen K. Stout, Edward D. Verrier, Valvular Heart Disease: Changing Concepts in Disease Managemen Acute Valvular Regurgitation. Circulation.2009; 119: 3232-3241 RobersonWS, Reverse doming of the anterior mitral leaflet with severe aortic regurgitation J am CollCardiol 1984:3:431 Perry GJ, Helmcke F, Nanda NC, Byard C, Soto B Evaluation of aortic insufficiency by Doppler color flow mapping J Am Coll Cardiol. 1987 Apr;9(4):952-9. Bonow et al 675ACC/AHA PRACTICE GUIDELINES—EXECUTIVE SUMMARY ACC/AHA 2006 Practice Guidelines for the Management of Patients With Valvular Heart Disease: Executive Summary JACC Vol. 48, No. 3, 2006. 605 August 1, 2006:598–675 American Society of Echocardiography: recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography Eur J Echocardiogr (2003) 4 (4):237-261. Christophe M. Tribouilloy, et al; Assessment of Severity of Aortic Regurgitation Using the Width of the Vena Contracta A Clinical Color Doppler Imaging Study Circulation. 2000; 102: 558-564 Arthur J. Labovitz, MD, FACC; Robert P. Ferrara, MD; Morton J. Kern, MD, FACC; Robert J. Bryg, MD; Denise G. Mrosek; George A. Williams, MD, FACC Quantitative evaluation of aortic insufficiency by continuous wave Doppler echocardiography J Am Coll Cardiol. 1986;8(6):1341-1347. Lancellotti et al. Assessment of Valvular Regurgitation. Eurpoean Journal of Echocardiography 2010;11 :223-244 Rokey R., Sterling L.L., Zoghbi W.A., et al. Determination of regurgitant fraction in isolated mitral or aortic regurgitation by pulsed Doppler two-dimensional echocardiography. J Am CollCardiol 1986;7:1273-1278. 16 Damon C. Sutton, MB, BS, FANZCA*, Roman Kluger, MB, BS, FANZCA*, Shihab U. Ahmed, MB, BS, MPH, Sharon C. Reimold, MD, Jonathan B. Mark, MD Flow reversal in the descending aorta: A guide to intraoperative assessment of aortic regurgitation with transesophageal echocardiography J Thorac Cardiovasc Surg 1994;108:576-582 Kim M, Roman M, Cavallini M, Schwartz J, Pickering T, Devereux R. Effect of Hypertension on Aortic Root Size and Prevalence of Aortic Regurgitation. Hypertension. 119;28:47-52 Simpson IA, Valdes-Cruz LM, Sahn DJ, et al. Doppler color flow mapping of simulated in vitro regurgitant jets: evaluation of the effects of orifice size and hemodynamic variables. J Am Coll Cardiol. 1989;13:1195–1207. Bolger AF, Eigler NL, Pfaff JM, et al. Computer analysis of Doppler color flow mapping images for quantitative assessment of in vitro fluid jets. J Am Coll Cardiol. 1988;12:450–457.