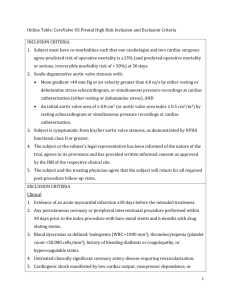
Online Appendix for the following October 20 JACC article
advertisement

Online Appendix for the following April 6 JACC article TITLE: Risk and Fate of Cerebral Embolism After Transfemoral Aortic Valve Implantation: A Prospective Pilot Study With Diffusion-Weighted Magnetic Resonance Imaging AUTHORS: Alexander Ghanem, MD, Andreas Müller, MD, Claas P. Nähle, MD, Justine Kocurek, MD, Nikos Werner, MD, Christoph Hammersting, MD, Hans H. Schild, MD, PhD, Jörg O. Schwab, MD, PhD, Fritz Mellert, MD, Rolf Fimmers, MD, Georg Nickenig, MD, PhD, Daniel Thomas, MD APPENDIX Supplementary methods Inclusion criteria Study inclusion criteria were: a) severe, symptomatic aortic stenosis with or without regurgitation and high perioperative risk, b) echocardiographic aortic valve annulus diameter >20 and <27 mm, and c) diameter of the ascending aorta <45 mm at the sinotubular junction. Exclusion criteria were contraindications to MRI, such as the post-interventional necessity of permanent pacemaker implantation, claustrophobia or hemodynamic instability impeding transport to DW-MRI, hypersensitivity, or contraindication to post-interventional dual platelet inhibition; sepsis or active endocarditis; excessive femoral, iliac or aortic atherosclerosis, calcification, or tortuosity; aortic aneurysm; bleeding diathesis or coagulopathy; recent cerebrovascular accident; mitral or tricuspid valvular insufficiency (> grade II); left ventricular or atrial thrombus; uncontrolled atrial fibrillation; previous aortic valve replacement; progressive disease with life expectancy <1 year and inability to give written informed consent. To identify potential sources of cerebral embolism, pre-interventional sonography of the carotid arteries, transthoracic and transesophageal echocardiography were conducted. All patients underwent coronary angiography and cardiac catheterizations with 6 French (F) catheters by use of a Terumo wire. Cranial MRI and imaging analysis The imaging protocol included transversal and coronal DWI, transversal T2-weighted turbo spin echo (Turbo spin echo (TSE); Repetition time (TR) / Echo time (TE): 4800 / 100 ms) and fluid attenuated inversion recovery (FLAIR; TR/TE 6000/120 ms) sequences. DWI was performed with a spin-echo echo-planar pulse sequence (TE: 78 ms; TR: 2921 ms; echoplanar imaging factor: 77; field of view: 240 mm; matrix: 128 x 256; section thickness: 5 mm; intersection gap: 1 mm; total acquisition time, 21.4 seconds) with diffusion sensitization bvalues of 0, 500 and 1000 s/mm2. Apparent diffusion coefficient maps were obtained in all cases. Follow-up MR imaging was performed at E3, using the same protocol of sequences in order to assess the presence or absence of a subsequent infarct at the location of the diffusion abnormality. Pre-existing brain abnormalities (e.g. microangiopathy, infarctions or atrophy) and the appearance of new hyperintense lesions in DWI on postoperative scans were evaluated. Only diffusion abnormalities consistent with embolic lesions were included in the analysis. Diffuse alterations in the diffusion-weighted image or patterns of watershed ischemia were excluded. Likewise, post-interventional new lesions were determined on the DWI images with maximum contrast between lesion and normal tissue signal. For volume quantification of new hyperintense lesions in DWI, the images were magnified fourfold, the area of lesion was manually delineated in each image slice by region of interest. For image analysis, the commercially available software of the MRI unit was used (Viewforum, Philips Healthcare, Best, The Netherlands). Transfemoral aortic valve implantation In the present study only third-generation (18F) devices were used. TAVI was performed with local anesthesia in combination with a mild systemic sedative treatment. The arterial sheath for transfemoral insertion of the prosthesis was gained by percutaneous puncture, mainly of the right femoral artery. Venous (7F) and arterial vascular access sites (6F) were inserted contralaterally. The aortic valve was passed with a Terumo guidewire and changed to an Amplatz Super Stiff wire (Boston Scientific Corp.). Balloon valvuloplasty was performed with a 20- to 25-mm balloon under rapid cardiac pacing The CoreValve® device was positioned during fluoroscopic guidance and deployed into the valve orifice in a retrograde approach. Hemodynamic parameters were assessed continuously during the procedure. Evaluation of post-procedural regurgitations was performed using a supra-aortic angiogram and transthoracic echocardiography. In case of post-interventional aortic regurgitation >grade II additional valvuloplasty within the CoreValve® prosthesis was performed. Percutaneous closure system (Prostar XL, Abbott Inc.) was routinely used for the closure of the 18 F arterial access sites. During TAVI, the patients received weight-adjusted intravenous heparin to achieve an activated clotting time of 300 – 350 s for the duration of the procedure. Additionally, acetylsalicylic acid and clopidogrel hydrogen sulfate were administered as recommended.