The Essentials of Valvular Heart Disease
advertisement
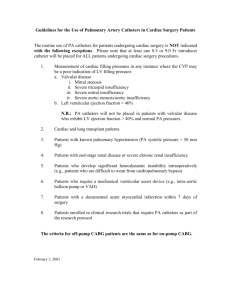
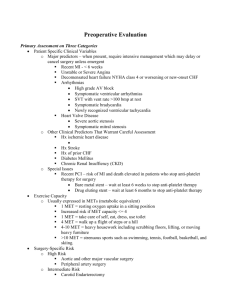
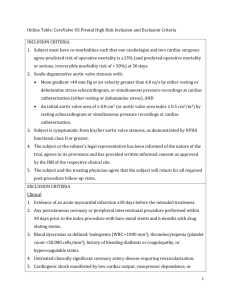
Some Essentials of Valvular Heart Disease CCU lecture series Case 1 • • • • • • 56 YO M presents for DOE 6 months Denies CP, syncope, palpitations PMH significant for hypercholesterolemia Had “murmur since I was a child” Mother died of heart failure in 60s Non-smoker Case 1 • • • • • • HR 66 BP 120/85 Neck: No bruits Chest: CTA CVS: RRR, harsh 3/6 SEM radiating to carotids Abdomen: Soft, NT Ext: No c/c/e Aortic Stenosis • • • • Obstruction most commonly located at the level of the aortic valve May be congenital or acquired (most common) Calcific AS is associated with traditional risk factors for atherosclerosis (smoking, high LDL, HTN) Also seen in ESRD, Pagets, SLE, alkaptonuria Pathophysiology • • • Aortic stenosis generally develops gradually, leading to LV hypertrophy As stenosis progresses, LVEDP begins to increase – LV function usually remains normal until late in disease process Diastolic dysfunction may also contribute to symptom onset Clinical Features • 1) 2) 3) 3 classic symptoms of severe AS DOE Syncope Angina Physical Exam • • • • Pulse Heart sounds (second heart sound) Murmur Other clinical manifestations (bleeding, embolic events, CAD) Testing • • • • • EKG CXR Echo Cardiac catheterization CT/MRI? Catheterization findings Cardiac MRI and CT Grading Severity of AS Low Gradient AS Indications for Surgery Indications for Surgery Treatment • • • • • No effective medical therapy for what is primarily a mechanical obstruction Aortic valve replacement is standard of care Mechanical vs. Bioprosthetic valves The Ross procedure Aortic root replacement? Balloon Valvuloplasty • • • 31 patients >90 years old who underwent balloon valvuloplasty from 2003-2006 Patients all had severe symptomatic AS and were deemed high risk for surgery Mean STS score was 18.5% Results • • • • 25 patients underwent retrograde BAV, 6 anterograde Mean AVA increased from 0.52 to 0.92 cm² Mean NYHA Class increased from 3.4 to 1.8 30 day mortality was 9.7% CoreValve • • 86 patients with symptomatic severe AS, >80 years old and high risk for cardiac surgery enrolled Percutaneous AV replacement attempted with 18 and 21 French systems Results • • • • • Acute device success was 88% Successful implantation led to a significant reduction in gradient Aortic regurgitation remained unchanged Procedural mortality was 6% 30 day mortality was 12% The SALTIRE Study • • • 155 patients with moderate to severe AS enrolled – randomized to 80 mg atorvastatin or placebo AV stenosis and calcification assessed by echocardiography and cardiac CT Primary endpoints changes in aortic jet velocity and AV calcium score SALTIRE • • LDL decreased to 62 mg/dl in the atorvastatin group, 131 in placebo No significant change in endpoints The Critically Ill AS patient 1) 2) 3) 4) Remember… Atrial fibrillation is bad! Vasopressor agents are preferable to inotropes for blood pressure support Think IABP early Always auscultate before you give NTG for chest pain! Management Recommendations Case Number 2 • • • • • 72 YO M in the emergency department has had CP x 5 days Finally decides to come to the ED Hypoxic on room air, rales 1/2 way up Heart sounds difficult to appreciate Troponin is 44 EKG Stat Echo performed… Acute Mitral Regurgitation Three main mechanisms • Flail leaflet due to mitral valve prolapse • Chordae tendinae rupture due to trauma, infective endocarditis or rheumatic fever • Papillary muscle dysfunction due to ischemia/infarction (what kind of infarction will more often present with acute MR?) Mitral Valve Anatomy Pathophysiology • • • Hemodynamic changes much more pronounced than in chronic MR due to lack of time for adaptation The abrupt increase in left atrial pressure is transmitted to the pulmonary circulation Cardiac output falls and systemic vascular resistance increases Clinical Manifestations • • • • Often present in cardiogenic shock and acute pulmonary edema Physical exam may reveal a hyperdynamic precordium (will the apex be displaced?) The murmur Up to 50% of patients will not have an audible murmur at the time of evaluation Testing • • • Echocardiography mainstay of diagnosis Cardiac catheterization may be required for determination of the extent and severity of concomitant CAD Hemodynamics are characteristic Mitral Regurgitation Treatment • • • Definitive treatment is surgical Supportive measures include nitroprusside (what is the mechanism?) and possibly dobutamine for low cardiac output IABP Class I Indications for MV Surgery in Severe MR Acute symptomatic MR • Chronic severe MR with NYHA class II, III or IV in absence of severe LV dysfunction and/or LVESD>55 mm. • Symptomatic or asymptomatic patients with mild/mod LV dysfunction (EF 30-60%) and endsystolic dimension >40 mm • MV repair recommended over replacement for majority of pts; pts should be referred to experienced surgical center. • Surgery • • • Surgical mortality can be as high as 50% however mortality is uniformly worse without surgical intervention Valve repair is always preferable to replacement, if possible The success rates depend on the etiology of the valvular dysfunction