002-Case of the Month - STA HealthCare Communications
advertisement

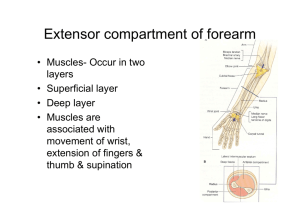
Emergency Department’s Case of the Month “ Am I having a stroke?” Katrina Hurley, MD and; Dave Petrie, MD, FRCPC Natalie’s wrist • Natalie, 77, presents to the ED with concerns that she has had a stroke. • Upon waking in her Lazyboy chair in the morning, she noticed a weakness in her left arm and hand. • She denies having any other symptoms and is otherwise feeling well. • She has a history of hypertension, diet-controlled diabetes and a remote myocardial infarction. • Her medications include: - enteric coated acetylsalicylic acid - metoprolol - atorvastatin • A visual examination reveals an apparent wrist-drop (Figure 1). Figure 1. The patient is asked to hold up her hands (extend wrists and fingers). She has a noticeable left-sided wrist-drop. Questions & Answers How is an upper motor neuron lesion (UMNL) differentiated from a lower motor neuron lesion (LMNL) in a physical examination? 1. Upper motor neurons project from the cerebral cortex to the anterior horn of the spinal cord (proximal to the -motor neuron). Classic signs of an UMNL include muscle weakness, increased muscle tone and increased reflexes. Lower motor neurons project from the anterior horn of the spinal cord via peripheral nerves to directly innervate skeletal muscle. Signs of a LMNL include muscle weakness, atrophy, fasciculations and decreased reflexes (Table 1). What are the features of radial neuropathy? 2. The radial nerve (C5-T1 roots) arises at the brachial plexus, passes through the spiral groove and divides into the posterior interosseous nerve and superficial radial nerve at the antecubital fossa. The radial nerve innervates the muscles that extend the fingers, thumb, wrist and elbow. The superficial radial nerve innervates the skin over the first interosseous muscle. Patients with classic wrist-drop have weak extensors (wrist, fingers and thumb) and impaired sensation over the first interosseous muscle. Depending on the cause of the neuropathy, the deficits may be incomplete. For example, a compressive neuropathy may spare some fascicles. The superficial radial nerve may be variably affected, making sensory loss an inconsistent finding. Axillary radial neuropathy is distinguished from classic wrist-drop by the addition of tricep involvement. Tricep weakness in the context of a radial neuropathy implies a lesion proximal to the spiral groove. The length of recovery depends on the degree of damage. Demyelination should improve over several weeks while axonal loss may take months or more. For more on Natalie see page 4. 2 The Canadian Journal of Diagnosis / May 2006 Case of the Month What is the differential diagnosis for radial mononeuropathy? 3. More on Natalie • On examination, the patient has a decreased brachioradialis reflex. The biceps and triceps reflexes are symmetric. Decreased power is limited to extensors of wrist, fingers and thumb. There is no discernable sensory deficit. In general, isolated mononeuropathies result from trauma. The most common etiology of radial mononeuropathy is compression. It occurs in several well-described scenarios: improper use of crutches causing axillary radial neuropathy; Saturday night palsy from malposition dur• Based on the history and physical ing drunken sleep, compressing the nerve in the spiral groove and findings, the patient is diagnosed with Bridegroom’s palsy inflicted on a sleeping groom as his bride’s head compression radial mononeuropathy. compresses the nerve in the spiral groove. Other causes of compression • Natalie was splinted in wrist and finger include mass lesions, as in neurofibromatosis or a fibrous band. Wristextensions and referred to both physioand occupational therapists. drop is also a reported manifestation of lead poisoning. Mononeuropathy can be associated with the use of Dapsone, excessive use of Ergotamine and abuse of opiates, sedatives and amphetamines. The differential diagnosis for neuropathy is broad, including diabetes mellitus, Lyme disease, numerous toxins Table 1 and entities like acute intermittent porphyria. Using physical examination to differentiate an UMNL from a LMNL UMNL LMNL Fasciculations Absent Present Muscle bulk Symmetric or slight atrophy Pronounced focal atrophy Motor tone Increased Decreased Motor power Non-focal weakness (distributed over muscle groups) Focal weakness (peripheral nerve or root distribution) Reflexes Increased Decreased Coordination Ataxia, dysmetria Not affected Dr. Hurley is a fourth-year resident in Emergency Medicine and a graduate student in Health Informatics, Dalhousie University, Halifax, Nova Scotia. Dr. Petrie is the Director, Division of EMS, Dalhousie University, Halifax, Nova Scotia. This department covers selected points to avoid pitfalls and improve patient care by family physicians in the ED. Submissions and feedback can be sent to diagnosis@sta.ca. Publication Mail Agreement No.: 40063348 Return undeliverable Canadian addresses to: STA Communications Inc. 955 boulevard St-Jean, Suite 306 Pointe-Claire, QC, H9R 5K3 4 What is the role of investigations in patients with mononeuropathy? 4. The physical examination is the most important tool to delineate the nature of a neuropathy. Consider a complete blood count, blood lead levels and serum glucose. If the patient fails to improve in a matter of weeks, an electromyograph would be prudent to confirm the diagnosis and localize the lesion. What treatment should be provided to patients with wrist-drop? 5. The most important treatment is to remove offending factors (i.e. compression). Supportive care, such as splinting to keep the wrist and fingers extended, is important during convalescence. Consultation with an occupational therapist would ensure a properly fitted splint. Failure to improve over the short term should also prompt a consultation with a physiotherapist. Dx References Available upon request The Canadian Journal of Diagnosis / May 2006