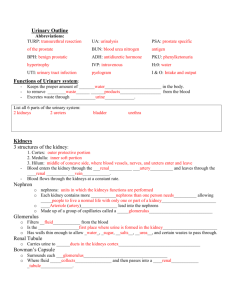
Urinary System Lecture Outline
advertisement

Chapter 26: Urinary System Functions of Urinary System: 1. Excretion – excrete wastes 2. Regulate blood volume and blood pressure by: a. adjusting water loss in urine b. releasing erythropoietin c. releasing renin 3. Regulate plasma concentrations of Na+, K+, Cl-, Ca++ 4. Stabilize blood pH by controlling excretion of H+ and HCO3 - 5. Assist liver with detoxifying poisons Main Organs: kidneys form urine send it through urinary tract (ureter → urinary bladder → urethra) Urinary Tract Organs Ureters: (see page 985) Smooth muscle tubes transport urine from renal pelvis of kidney to bladder Retroperitoneal Empty into posterior wall of bladder Histology of the Ureters: -inner lining is mucosa: transitional epithelial tissue -middle layer is smooth muscle peristaltic contractions roughly every 30 seconds -outer layer visceral peritoneum – connective tissue Urinary Bladder: Hollow, muscular organ , posterior to pubic symphysis lies anterior to the uterus in females held in place via peritoneum & ligaments (middle & lateral umbilical ligaments) trigone: triangular region with openings for urethra – works as a funnel internal urethral sphincter: located in “neck” of bladder involuntary innervated by both sympathetic and parasympathetic divisions of ANS -parasympathetic: relaxes internal sphincter 1 Histology of Urinary Bladder: lining is mucosa consisting of transitional epithelial tissue muscularis layer is smooth muscle: forms detrusor muscle: contracts to expel urine detrusor muscle also prevents urine from flowing back into ureters distends: muscles stretch (can hold up to 1 L) when empty collapses into folds called Urethra: drains urine from urinary bladder to outside female: urethra: anterior to vagina male urethra longer and subdivided into: 1.) prostatic urethra: 2.) membranous urethra: very short segment in floor of pelvic cavity 3.) penile (spongy) urethra: external urethral meatus (orifice): opening external urethral sphincter: (urogenital diaphragm): the valve for urine voluntary lining of urethra stratified squamous epithelial tissue Micturition Reflex: voiding or urination (page 989 figure 26-20) 1.) distension in urinary bladder activates stretch receptors ( reflex) 2.) afferent fibers in pelvic nerves carry impulses to spinal cord to thalamus to cerebral cortex of brain so become aware of urge. 3.) stimulates parasymp. fibers which cause contraction of bladder & relaxation of internal sphincter. external sphincter: voluntary can keep it closed reflex begins when urinary bladder contains about 200 ml of urine – cycles as bladder volume increases at 500 ml pressure will open internal urethral sphincter Incontinence: May be caused by trauma to internal/external urethral sphincters Or damage to CNS, spinal cord or nerves to urinary bladder 2 stress incontinence: from stretched or damaged sphincter muscles: increased intra-abdominal pressure causes urine to leak Urinary Retention: occurs in males due to enlarged prostate gland (prostatic hypertrophy) Kidneys: bean shaped T12 - L3: medial indentation termed - hilus: leads into renal sinus -renal blood vessels, ureters, adrenal gland is found superior to each kidney held in place via peritoneum & connective tissue 3 layers of connective tissue surround each kidney 1. fibrous renal capsule: innermost layer, directly attaches to kidney covers outer surface of kidney (layer of collagen) 2. perinephric fat (adipose) capsule: 3. renal fascia: dense irregular connective tissue surrounds both the kidney & adrenal gland anchors kidney to surrounding structures – fuses with peritoneum Sectional Anatomy of Kidney (page 956) Cortex, Medulla, Pelvis 1. Renal Cortex: 2. Renal Medulla: contains renal (medullary) pyramids papilla : rounded tip – faces renal pelvis base: flat portion – faces cortex each renal pyramid forms renal lobe each renal lobe contains nephrons which make urine 3. Renal Pelvis: formed from the minor and major calyces (minor calyx, major calyx) funnel shaped area collects pyelitis: infection of renal pelvis (usually from untreated UTI) pyelonephritis: infection of kidney 3 ● Signs/symptoms: high fever, intense pain on affected side, vomiting, diarrhea, blood and pus in urine ● Tx: intense antibiotic therapy Blood and Nerve Supply: (p. 958) kidneys receive 20-25% of cardiac output blood leaves heart to aorta – aortic arch – thoracic aorta – abdominal aorta: renal arteries enter thru hilus branch into ↓ segmental (lobar) arteries ↓ interlobar arteries ( pyramids to cortex) ↓ arcuate arteries(arch along boundary of cortex & medulla ↓ interlobular (cortical radiate) arteries (supply cortex) ↓ afferent arteriole (takes blood into glomerulus) ↓ glomerulus (capillary network) ↓ efferent arteriole (drains blood from glomerulus) ↓ peritubular capillaries (surround nephron tubules) ↓ venules ↓ interlobular veins ↓ arcuate veins ↓ Interlobar (cortical radiate) veins ↓ renal vein Note: Glomerulus is special capillary network: Receives blood from afferent arteriole Drained by the efferent arteriole Fenestrated capillaries Has higher pressure than systemic capillary beds Renal plexus: ANS: -sympathetic stimulation controls blood vessels: vasoconstriction/vasodilation Nephrons: each kidney contains consists of: 1. glomerular (Bowman's ) capsule (surrounds glomerulus) note Renal Corpuscle is Bowman’s capsule & glomerulus 4 2. proximal convoluted tubule (PCT) 3. Loop of Henle – descending & ascending limbs 4. distal convoluted tubule (DCT) 5. collecting duct Adaptations for each region of the nephron: (p. 960 Summary Table 26-1) 1. Bowman’s (Glomerular) Capsule: Site of Filtration Two layers: parietal epithelium: outer wall of capsule visceral epithelium: covers glomerulus podocytes: filtration slits: Lamina densa (basal lamina) 2. Proximal Convoluted Tubule: Main site of reabsorption - simple cuboidal epithelium -have microvilli 3. Loop of Henle: descending & ascending limbs -lower part of descend limb (thin segment) contains simple squamous epithelial tissue -permeable to water - impermeable to -ascending limb thick segment: -permeable to salts -impermeable to 4. Distal Convoluted Tubule: - simple cuboidal epithelial cells -lack -better suited for 5 Two types of Nephrons: 1. Cortical Nephrons: 85% of all nephrons Located mostly within Loop of Henle is short Efferent arteriole delivers blood into 2. Juxtamedullary Nephrons: 15% of all nephrons Loop of Henle extends deep into medulla Peritubular capillaries connect to vasa recta Juxtaglomerular Apparatus: regulates BP & rate of filtrate formation located at junction of DCT & afferent arteriole 3 Types of Cells: 1.) Mesangial Cells: support capillaries 2.) Granular (JG) cells in afferent arteriole: -smooth muscle cells -contain granules of renin -mechanoreceptors: 3.) macula densa cells -contains chemoreceptors (osmoreceptors) respond Principles of Renal Physiology 47 gallons fluid enter each day only 1% becomes urine and eliminated uses 20-25% of cardiac output nephrons form the urine by filtering blood - maintain homeostasis by regulating volume & composition of blood -excrete wastes (urea, creatinine, uric acidfrom blood, nephron filters them out of blood to eliminate them in urine Basic Processes of Urine Formation 1.) Filtration: hydrostatic pressure forces water/solutes out of blood into nephron (Bowman’s capsule) 2.) Reabsorption: removal of water/solutes from filtrate back into blood 3.) Secretion: transport of solutes from peritubular capillaries back into filtrate 6 Key Terms: Osmolarity: Is the osmotic concentration of a solution Total milliosmoles per liter (mOsm/L) number of solute particles per liter Body fluids have osmotic concentration of about 300 mOsm/L Ion concentrations In milliequivalents per liter (mEq/L) Concentrations of large organic molecules Grams or milligrams per unit volume of solution (mg/dL or g/dL) Reabsorption and Secretion use the following methods of transport: Osmosis Diffusion Carrier-mediated transport: requires carrier protein – if saturate carrier protein cannot transport molecule (termed transport maximum or Tm) which indicates renal threshold if renal threshold reached for reabsorption cannot reabsorb the substance and it is lost in urine example: Tm for glucose is 180 mg/dL If plasma glucose is greater than 180 mg/dL Tm of tubular cells is exceeded Glucose appears in urine: – glycosuria facilitated diffusion: active transport cotransport (symport) countertransport 1. Glomerular Filtration filtration is passive driven by hydrostatic pressure note: glomerular blood pressure is 50 mmHg vs 35 at arterial end of capillary bed nonselective: water, ions, glucose, AA, wastes all are filtered filtration membrane: barrier materials pass through membrane into capsule space and is termed filtrate Filtration Membrane: -filters b/w blood (in glomerulus) and glomerular (Bowman’s) capsule 7 -porous w/ 3 layers: 1. Fenestrated capillaries: 2. Visceral membrane of podocytes 3. Basement membrane (lamina densa): keeps most proteins out Net Filtration Pressure (NFP): The net force that causes filtration The balance between HP and OP of the glomerulus Pressures (forces) that push materials out of glomerulus – pressures that pull back into glomerulus NFP = G.H.P. - (G.O.P.+ Cs.H.P.) G.H.P. = glomeruluar hydrostatic pressure: (50 mmHg) – dependent on G.O.P.= glomerular osmotic pressure: (25 mmHg) – dependent on Cs.H.P.= capsule hydrostatic pressure: (15 mmHg) No Cs.O.P. why not? What type of factors would increase NFP? NFP = 50 - (25 + 15) NFP = 10 mmHg What type of factors would decrease NFP? Glomerular Filtration Rate (GFR) -amount of fluid filtered from blood into kidney per minute – 125 ml/minute Depends on: 1. total surface area for filtration 2. permeability of filtration membrane 3. NFP GFR is directly proportional to NFP therefore anything that alters NFP effects GFR Regulation of Glomerular Filtration A. Intrinsic: kidneys autoregulate B. Hormonal: initiated by kidneys C. Extrinsic: Sympathetic division of ANS A. Intrinsic: kidneys (renal) autoregulation Maintains GFR despite changes in kidney regulate glomerular filtration thru monitoring flow speed & contents (osmolarity) 8 if flow rapid (large amounts of filtrate produced) might not have time for reabsorption or if there is decreased filtrate and flow it will move too slowly and might absorb 1. Myogenic Mech.: responds to pressure changes: if systemic BP increases = rise in renal BP stretches walls of afferent arteriole which then causes the smooth muscle to contract which constricts the so it keeps glomerular pressure if reduced blood flow and/or systemic BP falls, causes dilation of the Kidneys can autoregulate at SBPs b/w 80 – 180 mmHg 2. Tubuloglomerular Feedback Mechanism Controlled by Macula Densa cells of juxtaglomerular apparatus in distal tubules respond to slow flowing filtrate and/or osmotic signals: if the flow is too slow need to speed it up by dilating the afferent arteriole but if flow is fast or high osmolarity, will constrict B. Hormonal Mechanisms (pg. 971) 1.) Hormones of the rennin-angiotensin system 2.) ANP ( ANF) 1.) Juxtaglomerular (JG) cells release renin cause anigiotensinogen →angtiotensin I which is converted to angiotensin II (with A.C.E.) Angtiotensin II: 1.) Triggers release of aldosterone 2.) Constricts efferent arteriole to increase glomerular blood pressure & GFR 3.) Powerful vasoconstrictor (systemic) 4.) Triggers release of ADH 5.) Stimulates thirst 3 factors trigger release of rennin from the JG cells 1. Decreased stretch of JG cells from decreased BP and/or decreased BV 2. Macula Densa cells cause vasodilation due to decrease is osmolarity of filtrate 3. Sympathetic nervous system 9 2.) ANP ( ANF) Released from the atria of the heart in response to stretching walls due to Increases Na+ excretion in the urine C. Extrinsic (Autonomic):sympathetic nervous system stress or emergency want to shunt blood to muscles Sympathetic activation: (NE & Epi) 1. constricts afferent arterioles 2. decreases GFR - slows filtrate 3. triggers the release of renin by JG cells 2. Tubular Reabsorption Reabsorbing substances from filtrate that were reabsorbed earlier filtrate similar to blood plasma except urine: mainly water, wastes need to get materials from filtrate back into blood so it doesn't become urine and is lost begins when filtrate enters the PCT Reabsorbed substances must pass through 3 cell layers to enter peritubular capillaries 1.) into tubule cell 2.) out of tubule cell into IF 3.) into peritubular capillary Glucose, AA reabsorbed via secondary active transport: cotransport with Na active transport: ion pumps for Na +, K+, HCO3-, Mg++, PO43 passive reabsorption of: water urea, Cl- and lipid soluble molecules Na+ reabsorbed several ways Cotransport Countertransport Solvent Drag: substances reabsorbed because water reabsorption increases their concentration in the filtrate (creates a concentration gradient for them). Nonreabsorbed Substances: because some urea, creatinine, uric acid 10 Different Regions of Tubules and What They Absorb: Proximal Convoluted Tubule: most involved in reabsorption Absorbs: 100% of the glucose & amino acids 75-80% of the Na+, ClLoop of Henle: Decending limb: permeable to water: water leaves via osmosis Ascending limb: permeable to salts: Na +, Cl- pumped out Distal convoluted tubule: Under hormonal control -Aldosterone: controls -ADH: controls 3. Tubular Secretion blood secretes molecules back into tubule (filtrate) last chance for Blood entering peritubular capillaries contains substances that did not cross filtration memrane H+ & K+ are both secreted in exchange for Na+ Countertransport: compete for secretion: secretion depends on their amounts in peritubular capillary blood Important for: 1. Disposing of undesirable substances 2. Eliminating excess K+ 3. Getting rid of substances that were 4. Controlling blood pH when pH decreases: when pH increases: note: aldosterone controls secretion of K + 11 Regulation of Urine Concentration and Volume: Loop of Henle Refers to exchange between tubular fluids moving in opposite directions Fluid in descending limb flows toward renal pelvis Fluid in ascending limb flows toward cortex The countercurrent mechanisms establish and maintain an osmotic gradient extending from the cortex through the depths of the medulla that allows the kidneys to vary urine concentration dramatically. Loop of Henle: (thin) Descending Limb: permeable to water osmolarity increases as filtrate moves from cortex to medulla concentrated filtrate in ascending limb accelerates Na + Cl- transport into peritubular fluid (thick) Ascending Limb: impermeable to water Contains active transport proteins to pump Salts elevate osmotic concentration in peritubular fluid Higher osmolarity of peritubular fluid creates osmotic pressure to pull water out of descending limb due to countercurrent mechanism This creates a hypertonic medulla which facilitated the removal of water from the descending limb The concentration of the interstitial fluid of the kidney increases as it moves from the cortex to the medulla. Increases solute concentration of filtrate: peaks 1200 mosm Na+ and Cl- account for aprx. 750 ml of the total 1200 ml of the IF of the medulla The rest is from urea Collecting tubules in deep medullary regions: permeable to urea as urine passes thru deep medullary regions urea leaves filtrate & enters IF of medulla to concentrate it diet deficient in protein would effect ability of medulla to be concentrated Vasa recta: special capillary loop found near Loop of Henle in juxtamedullary nephrons acts as countercurrent exchanger: 12 maintains osmotic gradient Formation of Dilute Urine: filtrate diluted as passes thru: when ADH not released by posterior pituitary: Formation of Concentrated Urine: ADH: decreases urine, by opening aquaporins hypertonic medulla creates OP to pull water from filtrate facultative water reabsorption: obligatory water reabsorption: release of ADH: continuously (when plasma osmolarity rises above 300 mosm) Urine production: typical urine has osmotic concentration of 800 – 1000 mOsm/L Diuresis: The elimination of urine Typically indicates production of large volumes of urine Diuretics: Drugs that promote water loss in urine: (Loop diuretics: Lasix: block Na+ pumps in ascending limb) Given to reduce: Osmotic diuretic: substance that is in the filtrate in collecting tubule in excessively high amounts and shouldn’t be there (glucose). Acts as an osmotic diuretic b/c ↑ tonicity of filtrate which creates OP Alcohol: inhibits ADH Caffeine: increases GFR – acts as diuretic 13 Renal Clearance: creatinine clearance test used to estimate GFR monitor creatinine in blood and amount in urine over 24 hr. period inulin is gold standard b/c its not secreted or reabsorbed – what goes in comes out RC of inulin is 125 ml/min RC< 125 means: some was absorbed RC = 0 indicates: completely reabsorbed RC > 125 means: some was secreted RC of urea= 70 ml/min of sodium= .9 ml/min creatinine= glucose=0 ml/min Aging and the Urinary System: ●decrease in number of functional nephrons (30-40% loss between ages 25 – 85) ● reduction in GFR ● reduced sensitivity to ADH ● problems with micturition reflex Characteristics of Urine: Urine sample depends on osmotic movement of water across walls of tubules & collecting ducts Clear, sterile solution Water content: Color: Urinalysis: the analysis of a urine sample is an important diagnostic tool Normal components of urine: urea, creatinine, ammonia, uric acid, bilirubin, urobilin Na+, Cl-, K+ Volume: Oliguria Polyuria pH: Specific gravity: the density of urine compared to water Specific gravity of water is 1.00 Clinical Applications Urinalysis: Hematuria Glycosuria 14 Proteinuria (albuminuria) Ketonuria Pyuria Blood Tests done to assess Kidney function: BUN: Creatinine: Potassium: Clinical Applications: 1. Kidney stones (renal calculi) Urine crystallizes to form hard stones S/S: pain, nausea, vomiting, hematuria Usually calcium phosphate or calcium oxalate or struvite Associated with higher intake of calcium & uric acid Seen on x-ray or CT scan medication, surgery or lithotropy Maintain hydration – less caffeine & dark sodas 15 2. Urinary Tract Infections (UTIs) bacterial or fungal pathogens more common in females (shorter, close to anus, sexual intercourse can push bacteria into urethra) ● urethritis: inflammation of urethra ● cystitis: inflammation of urinary bladder ● dysuria: 3. Bladder cancer 4X more prevalent in males most patiens are b/w 60-70 yrs. of age highest among cigarette smokers & employees in chemical & rubber companies S/S: hematuria, dysuria, change in bladder habits (usually no symptoms until cancer has progressed) spreads through adjacent lymph nodes/tissue quickly – prognosis for metastasized bladder cancer poor 4. Glomerulonephritis: Acute: usually associated with streptococcal infection (7-21 days after infect) ∙immune complexes becomes lodged in glomerulus, damages basement membrane Also can occur from bacterial endocarditis, viral infections, Lupus, signs/symptoms: hematuria, proteinuria (foamy urine), edema, hypertension, fatigue, decrease in urination, elevated BUN and creatinine levels Tx: depends on cause: antibiotics OR corticosteroids, plasmapheresis, dialysis Chronic: many causes: hypercholesterolemia, diabetes mellitus and lupus erythmatosus occurs from untreated acute glomerulonephritis irreversible – results in decrease GFR and accumulation of toxins often progresses to chronic kidney disease & end-stage renal disease 5. Renal Failure: kidney unable to perform functions Affects fluid balance, pH, muscle contraction, metabolism & digestion S/S: elevated BUN, plasma creatinine Oliguria Often hypertension occurs Decreased EPO causes decreased Hct Affects CNS: sleeplessness, seizures, delirium and even coma Acute renal failure: Occurs when renal ischemia, urinary obstruction, trauma or exposure of nephrotoxic drugs causes filtration to slow or stop. 16 Decreased kidney function occurs over a few days and might persist for weeks. Require dialysis Kidneys may regain partial or complete function once underlying problems is treated. Chronic renal failure Kidney function deteriorates gradually and problems accumulate over years Irreversible – progression only slowed Go into “end-stage renal failure”: when kidneys function at <10% of normal capacity requires dialysis and/or kidney transplant 17