Case study Re-emergence of Diphtheria
advertisement

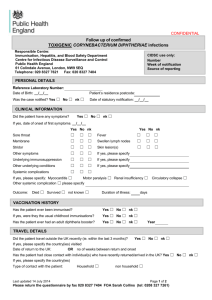
Case study Re-emergence of Diphtheria-evaluation and outcome--- An institutional overview Swagata Khanna1, Manabendra Debnath2,Manas P Das3- Guwahati (Assam) Abstract: Diphtheria was quite prevalent in the pre-immunisation era. But with the advent of proper immunisation the prevalence of Diphtheria has gradually decreased&it is very rare in developed countries.Classical Diphtheria still persists in many parts of India despite wide immunisation coverage. This study was carried out in the Department of ENT,Gauhati Medical College&Hospital,Guwahati,Assam for a period of 4years from January2010toDecember2013 with the purpose(1)To study the patients with membranes in throat & related deaths,(2)To find out the difficulties & constraints in diagnosis and treatment,(3)To evaluate & formulate a proper institutional treatment protocol and outcome of treatment.A total of 70 patients with membranes in throat were studied,45were suspected to be due to Diphtheria & of these 20patients died.It was found that inadequate immunisation,late presentation to tertiary health centres,lack of ICU facilities, poor availability&high costs of essential drugs like Anti-Diphtheric Serum & lack of proper institutional treatment protocol were the main reasons for such a scenario.We formulated a definitive approach & proper treatment protocol for treating such patients.Thereafter,15patients although all cases not proved by microbiological tests but with high clinical suspicion of Diphtheria were treated according to our institutional treatment protocol&these patients recovered&survived and the efforts are still continuing. Key words: Diphtheria, immunisation, Anti-Diphtheric Serum. Introduction Diphtheria was quite prevalent in the pre-immunisation era. But with the advent of proper immunisation the prevalence of Diphtheria has gradually decreased & it is very rare in developed countries. Classical Diphtheria still persists in many parts of India despite wide immunisation coverage.Diphtheria is a highly contagious and potentially life threatening bacterial disease caused by Corynebacterium diphtheriae.In 2008, India contributed 6081 (86.66%) of the 7017 diphtheria cases reported globally. There were no reports of outbreaks of diphtheria in Assam since last few years, though sporadic cases were reported in UIP monthly report, which were never investigated and documented. The immunization coverage in Assam was 19.30% in 2006 (RHS), which has improved to 67.60% in 2006-2007 [1]. But in spite of all efforts the cases of membranous tonsillitis with high suspicion of Diphtheria and related deaths are on the rise recently. Aim and objectives- The aim of this study is to find out the cause of the sudden rise in Diphtheria cases with the following objectives,to study the patients with membranes in throat & related deaths,to find out the difficulties & constraints in diagnosis and treatment,to evaluate & formulate a proper institutional treatment protocol and outcome of treatment. Materials and methods The study was carried out in the Department of ENT, Gauhati 1 25 Medical College & Hospital, Guwahati for a duration of 4 years from 1st January 2010 to 31st December 2013. It is a hospital based study.The data was collected from hospital records since January 2010 onwards. All details regarding the patients like Age, Sex, residential address, Diagnosis, treatment given were studied. Also, death due to diphtheria if any were also noted. The patients with membranous tonsillitis those are admitted in our department, proper history regarding the onset of the disease process, immunisation status, associated symptoms like fever, odynophagia, cervical lymphadenopathy, nasal blockage, respiratory distress etc were evaluated.Proper general, local and systemic examinations were carried out.The pseudo membrane over the tonsils and soft palate is properly studied and also if there is any bull neck appearance. Respiratory as well as cardiac involvement is also examined properly.After proper history and clinical examination, multiple throat swabs were sent for smear for KLB and culture and sensitivity.Chest X-ray and ECG on repeated occasions were done to rule out any cardiac involvement.Benzyl Penicillin was started immediately in required doses.Anti-Diphtheric Serum in required doses according to the extent of the disease was started on high clinical suspicion of Diphtheria.In 2 cases,emergency tracheostomy was also done.The cases as far as possible was notified to NRHM office for information regarding immunization process.The data obtained were critically analysed with the various data found in the State Programme Professor & Head, 2Senior Resident, 3Resident, Department of ENT and Head and Neck Surgery, Guwahati Medical College, Guwahati, Assam National Journal of Otorhinolaryngology and Head & Neck Surgery, Vol. 2(11) No. 2, August 2014 Implementation Plan 2011-2012. Results and observations A total of 70 patients with membranes over tonsils, oropharynx and nasopharynx were studied, out of which 45 patients were clinically suspected to be due to Diphtheria. Only 9 out of these 45 were proven microbiologically.In our study it is seen that in 2010, 50% patients diagnosed with membranes in throat was suspected to be due to Diphtheria. Out of these ,57.14% patients died due to Diphtheria and its complications.In the year 2011, 57.14% patients with membranes in throat were due to clinically suspected diphtheria. Out of these, 25% died.Similarly, in the year 2012, 63.16% patients with membranes in throat were due to diphtheria and 33.33% patients died.In 2013, 81.81% cases with membranous tonsillitis were due to diphtheria and 55.55% patients succumbed to it. Also, there was a sudden spurt in Diphtheria cases in the year 2013. It is observed that the incidence of diphtheria cases was more among Muslims compared to other religions. Discussion In 1613, Spain experienced an epidemic of diphtheria. The year is known as "El Año de los Garotillos" (The Year of Strangulations) in history of Spain[2]. Before 1826, diphtheria was known by different names across the world. In England, it was known as Boulogne sour throat, as it spread from France. In 1826, Pierre Bretonneau gave the name to disease as diphtérite (from Greek diphthera "leather")describing the appearance of pseudomembrane in the throat[3].In 1883, Edwin Klebs identified the bacterium and named it Klebs-Loeffler bacterium. The club shape of bacterium helped Edwin to differentiate it from other bacteria. Over the period of time, it was called Microsporon diphtheriticum, Bacillus diphtheriae and Mycobacterium diphtheriae. Current nomenclature is Corynebacterium diphtheriae.Friedrich Loeffler was the first one to cultivate Corynebacterium diphtheriae in 1884. He used Koch's postulates to prove association between Corynebacterium diphtheriae and Diphtheria.In 1890, Shibasaburo Kitasato and immunized guinea pigs with heat-treated diphtheria toxin. Von Behring won the first Nobel Prize in medicine in 1901 for his work on diphtheria. Over the Christmas holiday in 1891 in Berlin, the first attempt to cure a person of diphtheria was made. It succeeded. ... it was the first cure[4].Corynebacteria are Gram-positive pleomorphic bacilli with a Chinese lettering-like appearance on Gram stain. Nontoxigenic strains rarely cause more than local selflimiting disease but lysogenic conversion can occur at a site of colonization, and this has been suspected to have happened in several outbreaks[5][6]. The diphtheria toxin exerts a lethal 26 effect on all human cells by inhibition of protein synthesis with resulting pharyngeal damage and with absorption into the bloodstream, subsequent myocardial and neurological toxicity. Three biotypes of C. Diphtheriae exist: gravis, mitis and intermedius types; the gravis and intermedius types are associated with a higher rate of mortality which is probably related to the amount of toxin production. Less commonly Corynebacterium ulcerans can also be infected by this bacteriophage and produce a Diphtheria-like presentation[7].Diphtheria is a rare condition in countries which have a routine childhood immunization programme, but remains an important differential particularly in immigrant populations in the diagnosis of acute laryngeal infection in children. Diphtheria remains a significant public health problem in the developing world. The causative organism is Corynebacterium Diphtheriae. There are three strains, gravis, intermedius and mitis; it is the gravis strain which is responsible for major epidemics and for the high mortality. The early clinical picture of upper respiratory tract symptoms is due to the effects of the organism itself. Delayed effects are due to the release of endotoxin. Diphtheria is a disease particularly affecting young children; it is rare over the age of ten years[8]. Initial symptoms are of pharyngitis with sore throat and malaise. The child is feverish and on examination there is a typical appearance of the pharyngeal tonsils with necrosis and the development of a characteristic grey pseudomembrane over the surface. This consists of necrotic tissue, bacteria and a rich fibrinous exudate.Early removal causes bleeding but the pseudomembrane may separate more easily later in the course of the disease. There may be a bull-neck appearance due to cellulitis and regional lymphadenopathy[8]. Laryngeal diphtheria rarely occurs without prior pharyngeal infection. After progressive dysphagia and toxaemia, inspiratory stridor and a barking cough develop; the cough is frequently paroxysmal and exhausting.Death may follow owing to acute airway obstruction or as a result of the later effects of the endotoxin[8].The endotoxin can cause a toxic myocarditis in the second week of the disease and this may be fatal. Peripheral neuritis may also occur, palatal paralysis being the most common effect of peripheral neuropathy and presenting with nasal regurgitation of food and hypernasal speech.Successful treatment depends on early diagnosis, and the administration of high dose benzylpenicillin and antitoxin (10,000 to 100,000 units depending on the severity of infection). Airway management consists of removal of the laryngeal membrane, administration of oxygen and humidification, and endotracheal intubation or tracheostomy if necessary. Systemic steroids may reduce the need for National Journal of Otorhinolaryngology and Head & Neck Surgery, Vol. 2(11) No. 2, August 2014 airway intervention. Bed rest is recommended until the danger of myocarditis is past[9].The EPI of WHO recommends three doses of DPT vaccine starting at six weeks of age with additional doses of diphtheria vaccine in countries where resources permit. Many national immunization programs, including the UIP in India offer two booster doses at 18 months and between 54 to 72 months of age; after three doses of primary vaccines, protective levels of antitoxin develop in 94-100% of the children. However without booster doses, over time toxoid induced antibody drops below protective level[1].In Assam, the immunization status of DPT from 2005 to beginning of 2010 was more or less stable but in the year 2010-2011 there was a sudden dip in the immunization of DPT which may have lead to the spurt in cases of Diphtheria.Moreover, the overall immunization status of Assam in the year 2010-11 up to Dec2010 is 65.07%, also, a dip can be seen compared to earlier years.Also it is observed in our above Result & Observation section that there was sudden and gradual increase in Diphtheria cases 2012 onwards.After the above observations we put forward some leading questions to ourselves like:What are the reasons of this spurt in (?) Diphtheria cases?,What are the causes of increase in death due to (?) Diphtheria? Is there a need of an institutional protocol for treating (?) Diphtheria?,Above all the main problem we have faced in those that cases where throat swab results are negative for KLB. Going ahead with all these leading questions in mind, several mortality meetings were held in our Department where we critically discussed most of the deaths due to (?) Diphtheria.After critically analysing the cases it was seen that almost all the cases that died suffered from (?)Diphtheria had incomplete immunisation history or had not taken immunisation at all.Moreover, the incidence was on the higher side in a definite religious group as seen in the study.The reasons for this inadequate immunisation could be patients hailing from difficult areas, ignorance of the people regarding immunisation and reluctance of some group of people or communities to avail immunisation due to the false myth persisting in them regarding immunisation. The sudden increase in deaths due to (?)Diphtheria may be due to:Late presentation of the patients in hospitals, An institutional treatment protocol was formulated in consultation with Department of Paediatrics:-Proper history specially immunisation status,Isolation of the patient,Proper clinical examination and early diagnosis,Vitals to be monitored continuously, Proper resuscitation and ICU care if required,Repeated throat swab for KLB and culture and S e n s i t i v i t y, S e r i a l E C G t o r u l e o u t c a r d i a c manifestations,Start Benzyl Penicillin empirically in required 27 doses (varies from case to case),Start ADS on clinical Suspicion in required doses (varies from case to case).Add antibiotics depending on culture & sensitivity reports,Also to add steroids depending on symptoms,Notify cases to the hospital authority as well as NRHM office.After formulating the protocol for treating Diphtheria cases in our department, 15 cases were treated according to the said protocol and results are fruitful. The patients recovered and efforts are still continuing in our department and we are trying to improve ourselves more and more in the days to come. References 1. Nath B, Mahanta TG: Investigation of an outbreak of diptheria in Borborooah block of Dibrugarh district, Assam. Indian J Community Med 2010, 35(3):436–438. 2. LAVAL, Enrique (March 2006). "El garotillo (Difteria) en España (Siglos XVI y XVII)". Revista chilena de infectología 23. doi:10.4067/S071610182006000100012. Retrieved 29 November 2012. 3. "Diphtheria”. Online Etymology Dictionary. Retrieved 29 November 2012 4. John M. Barry, The Great Influenza; The Story of the Deadliest Pandemic in History (New York: Penguin Books, c2004, 2005) p. 70. 5. Pappenheimer Jr AM, Murphy JR. Studies on the molecular epidemiology of diphtheria. Lancet. 1983; 2: 923-6. 6. Wilson AP. Treatment of infection caused by toxigenic and non-toxigenic strains of Corynebacterium diphtheriae. Journal of Antimicrobial Chemotherapy. 1995; 35: 712-20. 7. Lipsky BA, Goldberger AC, Tompkins LS, Plorde JJ.Infections caused by nondiphtheria corynebacteria.Review of Infectious Diseases. 1982; 4: 1220-35. 8. “Diphtheria”.Paediatric Otorhinolaryngology Part 12. Scott-Brown'D Otorhinolaryngology,Head and Neck Surgery.p-1130. 9. Havaldar PV. Dexamethasone in laryngeal diphtheritic croup. Annals of Tropical Paediatrics. 1997; 17: 21-3. Address for correspondence Dr. Swagata Khanna, SWAGAT, J.P. Agarwalla road, Bharalumukh, Guwahati District-Kamrup Metro, Assam 781009 Email:drswagatakhanna@gmail.com, Cell : +91 9864094140 National Journal of Otorhinolaryngology and Head & Neck Surgery, Vol. 2(11) No. 2, August 2014