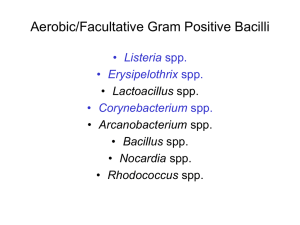
Non-Sporing Gram positive bacilli
advertisement

Non-Spore-Forming Gram-Positive Bacilli Non-Spore-Forming Gram-Positive Bacilli • Corynebacterium C. diphtheriae Disease Diphteria Opportunistic infections by other Corynebacterium species (diphteroids) Properties • Club-shaped also V- or L-shaped • Methachromatic granules (Albert staining): Beaded appearance • Nonmotile, no capsule • Facultative anaerobic • Classified in CNM (Corynebacterium, Nocardia, Mycobacterium) group. Biotypes (based on colony shape, biochemical properties and virulence) Gravis Mitis Intermedius Belfanti Culture • Sheep blood agar: It supports the growth of C.diphtheriae: Granular, gray, irregular edges, alpha hemolysis (sometimes) • Loeffler serum slope: It is not a selective medium but gives abundant growth and morphology of C.diphtheriae. This medium can also be used as a transport medium. • Culture • Blood tellurite agar: - Tellurite reduction - It enhances the chances of isolation of C.diphtheriae from clinical specimen in which commensal bacterial flora may also be present - It differentiate different vars. Growing colonies of Corynebacterium diphtheria on Telorit potassium Blood agar Clinical finding • Common diphtheria (Nasopharyngitis) Incubation period of 2–5 days. Fibrinous exudate “pseudomembrane” - Sore throat - Fever - Enlargement of neck lymph nodes and neck edema - Irregulatory of cardiac rhythm and myocarditis - Difficulties with vision, speech and swallowing This micrograph reveals an intranuclear inclusion body in a heart section from a patient with diphtheria-related myocarditis. Clinical findings • Corrosion of myelin sheaths in the central and peripheral nervous system leading to degenerating motor control. Cutanous diphtheria (a secondary infection) Transmission • Humans are the only natural host • C. diphtheriae reside in the upper respiratory tract • Transmitted by airborn droplet • Infection at the site of a pre-existing skin lesion Pathogenesis • Invasivness - Cord factor A glycolipid inhibits eukaryotic cell oxidation. - Nuraminidase Removes N-acetyl nuraminic acid from musine membranes. • Exotoxin Exotoxin (Encoded by gen tox from a temperate phage) Fragment B. Binding of the toxin Fragment A. Enzymatic activity A B Exotoxin mechanism Nicotinamide adenine dinucleotide phosphate (NAD) Exotoxin (A fragment) Nicotinamide ADP Reaction with EF2 Protein synthesis inhibition ADP-EF2 Testing immunity (Schick’s test) • Toxin Intradermal injection (0.1 mL): I. Cause inflammation (4-7 days later): No antitoxin in patient II. No inflammation: Antitoxin is present (Immune person) Important points about diagnosis of diphtheria • The diagnosis is a laboratory emergency. • Mild cases resemble pharyngitis and pseudomembrane may be lacking. • Diphtheria is not diagnosed easily on clinical grounds: Streptococcal pharyngitis & Vincent's pharyngitis Important points about diagnosis of diphtheria • Non-toxigenic strains of C.diphtheriae have the potential to cause invasive disease and to undergo lysogenic conversion to toxin producers in vivo leading to disease. • Specimen should be transported (e.i. by Amies medium)and processed as soon as possible. Laboratory diagnosis • Swabs should be taken both from the throat and the nose. • Preferably two swabs should be collected from the site most affected. • Microscopic observation (differentiation from streptococcal and Vincent's pharyngitis) Laboratory diagnosis • Isolating the organism • Demonstrating toxin production - Animal inoculation - Eleck test - ELISA (Enzyme-linked immunosorbent assay) • PCR to detect tox gene Elek test Treatment • Tracheostomy in children (to prevent croup) • Antitoxin (Intra muscular) • Penicillin or erythromycin Prevention • Vaccination DPT vaccine: A combination of diphtheria toxoid, tetanus toxoid, and killed pertusis organism. Given at 2, 4 an 6 months of age, with a booster at 1 and 6 years of age and then each 10 years afterward. (DPT or DT) The toxoid is prepared by treating the exotoxin with 0.3% formaldehyde. Listeria monocytogenes • Small rod (Coccobacillus: 1-2 micron) like “chinese character”. • In old cultures 6-20 micrones. • No capsule, Facultative aerobic. • Tumbling movement in 25 c • Growing in 4c • Resistant to cold, heat, salt, pH extremes, and bile In 37 centigrade In 20 – 25 centigrade Listeria monocytogenes • Small, gray and smooth colonies with a narrow zone of beta hemolysis. • Growth in low O2 and 5-10% CO2 • Fermentater, Catalase +, Oxidase + Transmission • The organism is distributed worldwide in animals, plants, soil, stream water, sewage, unpasteurized milk, vegetables. • Transmission to human by contact with animals or their feces. • Endogenously from gasterointestinal tract. Listeriosis • Rarely the cause of human disease • Potentially lethal food-borne infection case fatality rate: For those with a severe form of infection is 25%. (Salmonella, in comparison, has a mortality rate estimated at less than 1%) Virulence Factors • Soluble components: - Hemolysins - Soluble antigens : Lypolytic Ags - Endotoxins (LPS): Cold Aglotinin: Abs react with RBC at low temp (28-31 c): Lysis of RBC Epidemiology • Primary reservoir is soil and water; animal intestines. It contaminates foods and grow during refrigeration • Listeriosis – most cases associated with dairy products, poultry, and meat • Often mild or subclinical in normal adults. • In immunocompromised, fetuses, and neonates affects brain and meninges. 52 Epidemiology • Pregnant women susceptible • Infection passed to fetus prenatally across placenta • Postnatal neonates acquire infection in birth canal 53 Disease • Meningitis and sepsis in: 1. The fetus or newborn I. Granulomatis Infantiseptica (during pregnancy) or II. Late listeriosis (5 days after giving birth). 2. Immunosuppressed adults (especially renal transplant patients) 3. The infected mother: asymptomatic or influenzalike illness/ Abortion Pathogenesis • Listeria induces macrophage phagocytic uptake: • Internalins & D-galactose (in their teichoic acids) bound by the macrophage's polysaccharide receptors (E-cadherin) • Once phagocytosed (as Phagosome), then encapsulated by the host cell's acidic phagolysosome. • Listeria, escapes the phagolysosome by lysing the vacuole‘s membrane with hemolysin (listeriolysin O). Pathogenesis Internalin E-cadherin Phagocytosis Into macrophages & epithelial cells Forming filopods Phagocytiosis By macrophages and hepatocytes Inducing actin polymerization in cytoplasm Release from phagolysosome Phagolysosome formation (acidic condition) Lysteriolysin O secretion Figure 19.10 Multiplication cycle of Listeria monocytogenes 58 Lab. diagnosis • Microscopic observation: Diphtheroids • Isolation by culture: Blood and CSF samples on blood agar • Cold Enrichment • Rapid diagnostic tests using ELISA, immunofluorescence, and DNA analysis Prevention • Effective sanitation of food contact surfaces: Alcohol & Quaternary ammonium • 4°C discourages bacterial growth. • pasteurization and well cooking • Cell-mediated immunity is active (but no immunization) Treatment • Penicillin Resistant are rare • Ampicillin and trimethoprim/ sulfamethoxazole Lactobacilli Lactobacillus • Methachromatic granules (Albert staining) • Nonmotile • no capsule • Facultative anaerobic, microaerophilic or aerotolerant anaerobic • L. casei L. acidophilus, L. salivarius, L. reuteri Are the representatives of distinct subclades. Lactobacillus are a major part of lactic acid bacteria group: mostly convert lactose and other sugars to lactic acid. They are common and usually benign. In humans they are present in vagina and gastrointestinal tract inhibiting the growth of some harmful bacteria. Erysipelothrix rhusiopathiae (causing Erysipeloid) • Gram-positive rod (sometimes looks like GNB) • Single, streptobacilli, sometimes filamentous. • Catalase -, Oxidase -, Indol – • SH2 in TSI • Microaerophilic needed 5% co2 72 • Small shiny or white colonies • Alpha hemolytic on BA • Differentiated from Listeria by Alpha hemolysis and SH2 & catalase. Transmission • in environment and normal flora in sheep, chickens, and fish, duck (indigenous zoonotic Infectious disease) • Transmission from animals or their products to human • Primary reservoir – tonsils of healthy sheep & pigs. • On the surface of fresh fish Erysipeloid on hand 75 Pathogenesis & Clinical findings • Enters through skin abrasion, multiplies to produce erysipeloid, dark red lesions without systemic symptoms. • Latent period: 2-7 days • Sever pain, inflamation with purple color lesions on skin. • No pus (differentiation from Staphyloccocal and Streptococcal infections) • Endocardit 76 Control and treatment • • • • Penicillin or erythromycin Treated after 3-4 weeks Always resistant to vancomycin Vaccine for sheep and pigs Lab diagnosis • Biopsy or aspirated liquids from the edge of lesions. • Blood sample in case of endocardit. Chronic swimming pool granuloma 80 • In severe cases, they may penetrate the surrounding bone and muscle to the skin, where they break open and leak large amounts of pus. The purulent leakage via the sinus cavities contains "sulfur granules," not actually sulfur-containing but resembling such particles. These granules contain progeny bacteria. Diagnosis • The disease is suggested by a supportive lesion with Gram-positive filaments in the exudate. • Sulfur granules may be present. • Bacterial isolation and identification Control • Good oral hygiene • Antibiotic trapy: Penicillin • Drainage of lesion Actinobacteria • They include some of the most common soil life, freshwater life, and marine life, playing an important role in decomposition of organic materials, such as cellulose and chitin, and thereby playing a vital part in organic matter turnover and carbon cycle. • Actinobacteria are well known as secondary metabolite producers and hence of high pharmacological and commercial interest. In 1940 Selman Waksman discovered that the soil bacteria he was studying made actinomycin, a discovery for which he received a Nobel Prize. • Since then, hundreds of naturally occurring antibiotics have been discovered in these terrestrial microorganisms, especially from the genus Streptomyces. • Some Actinobacteria form branching filaments, which somewhat resemble the mycelia of the unrelated fungi, among which they were originally classified under the older name Actinomycetes. Most members are aerobic, • a few, such as Actinomyces israelii, can grow under anaerobic conditions. Unlike the Firmicutes, the other main group of Grampositive bacteria, they have DNA with a high GC-content, and some Actinomycetes species produce external spores. • Some types of Actinobacteria are responsible for the peculiar odor emanating from the soil after rain, mainly in warmer climates.[7