Corynebacterium diphtheriae file
advertisement

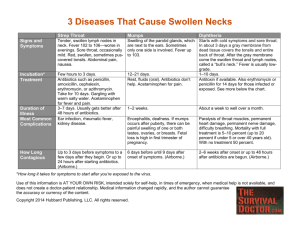
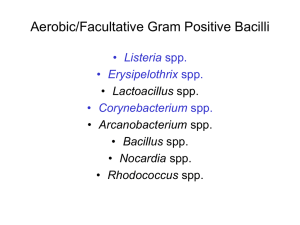
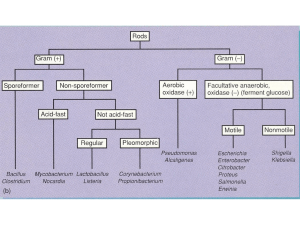
Introduction • • • • Klebs--1883 discovered Loefflers--1884 cultured Also known as KLB Emil von Behring- 1890 produced antitoxin • Awarded nobel prize Emil Von Behring Morphology • • • • Gram positive bacilli. 3-6 μ x 0.5-0.8 μ. v or k or L shape. Chinese letter pattern, angular arrangement Metachromatic granules. volutin granules, polymetaphosphate energy storage depots • Alberts stain – green and bluish black • Nonmotile noncapsulated, nonsporing • pleomorphic Cultivation • Loefflers serum slope– creamy white colonies in 6-8 hrs • Potassium tellurite medium—black colonies • Blood agar Biochemical reactions • • • • • Hiss serum Ferments glucose ,maltose with acid only Lactose, sucrose, mannitol not fermented Urease negative Starch –only gravis type, not intermedius or mitis Pathogenicity • • • • • • • Produces exotoxin Lysogenic conversion with beta phage Toxin – heat labile protein A and B fraction Toxicity- disease Antigenicity- immunity Toxoid – toxin without toxicity Toxin Mechanism of action -B subunit binds to receptor -toxin molecule cleaved at protease sensitive site between A-B portion (remain bonded by disulfide link) -receptor-toxin complex englufed into vesicle of host cell -reduction of disulfide bond, A subunit released into cytoplasm -Necrosis/neuotoxic effects on organism by exotoxin Biotypes 1)gravis(13 types)-most serious disease Colonies: large, irregular, gray 2)mitis(40 types)-mild illness colonies: small, round, convex, black 3)intermedius(4 types)-intermediate severity Colonies: small, flat and gray Diphtheria • • • • Children, fatal if not treated in time Exclusively human disease Droplet infection- fomites Fever, cervical lymphadenopathy, pseudomembrane • Myocarditis arrhythmia fatal • Polyneuropathy, paltine paralysis • Rare in adults. Pseudomembrane formation Thick membrane lining throat that interferes with eating, drinking and breathing Contents: WBC, RBC, bacteria, disintegrating epithelial cells Cause: fibrinous exudate from local necrosis by exotoxin (removal of PF may cause bleeding) Localization: faucial, laryngeal, nasal, otitic, conjunctival, genital, cutaneous Faucial: Signs: sore throat, fever complications: prostration, dyspnea, asphyxia, arhythmia, difficulties of speech, vision, swallowing, movement Septic: Ulceretic: Clinical classification i) Malignant (hypertoxic) diphtheria Signs: severe toxemia and adenitis, lymph glands swelling in the neck Complications: death-circulatory failure, paralytic sequelae ii) Septic diphtheria: Signs: ulceration with pseudomembrane formation and cellulites (gangrene around pm) iii) Hemorrhagic diphtheria Signs: local and general bleeding from edge of psudomembrane, conjunctival, epistaxis and purpura Complications 1)Asphyxia-obstruction of resp tract 2)Acute circulatory failure 3)kidney failure 4)paralysis-soft palate, eye muscles, extremities (3rd-4th week) 5)septic sequelae-pnemonia, otitis media Laboratory diagnosis • Sample collection: Throat swab or swab from membrane • Microscopy: Gram stain and Alberts stain • Culture: Loefflers and PT • Biochemicals • Virulence test in vivo and in vitro Virulence test contd In vivo Guinea pig– subcutaneous intradermal Test and control animals to be used In vitro Eleks gel precipitation test Toxigenicity test (virulence test) i) Animal inocculation -bacteria culture emulsified in water and 0.8 ml injected into 2 guinea pigs GP A-has dipht antitoxin (injected 2 hours before) GP B-Doesn't have antitoxin Result: Guinea pig B dies. ii) Elek's gel precipitation test -filter paper saturated with antitoxin is placed on agar plate with 20% horse serum -bacterial culture streaked at right angles to filter paper iii) tissue culture test -incorporation of bacteria into agar overlay of eukaryotic cell culture monolayers. Result: toxin diffuses into cells and kills them iv) PCR assays -test presence of specific bacteriophate gene (tox) Elek's gel precipitation test EPIDEMIOLOGY • • • • • • • • Formally important pediatric disease Developed countries - Eradicated Developing countries serious problem Rare in 1st year – maternal antibodies Peak 1-5 years, 5-10 years- decreases there after Immunity – sub clinical infections Carriers outnumber cases – throat & nasal Rarely spread through milk Prevention • Active immunity- DPT dosage – Antitoxin level – 0.01/ ml protective • Passive immunity- ADS – When susceptibles are exposed – 500 – 1000 units sc of Anti Diphtheritic Serum ( ADS) • Combined immunisation – First dose of adsorbed toxoid on one arm – ADS on another arm – To be continued with full course of active immunization Prevention a) DTP (DPT)• Formal toxoid - Incubation of Toxin at pH 7.4 -7.6 for 3 – 4 weeks at 37 °C • Adsorbed toxoid – purified toxoid adsorbed on to aluminum phosphate or hydroxide • triple vaccine given to children. trivalent preparation • Diphtheria toxoid, Tetanus toxoid and Pertussis vaccine Td- contains absorbed tetanus and ten-fold smaller dose of diphtheria toxoid. b) Schedule i) primary immunization – - infants and children - 3 doses, 4-6 weeks - 4th dose after a year - booster at school entry ii) Booster immunization - adults - Td toxoids used (traveling adults may need more) Shick test-to test sensitivity (allergic reaction) Treatment • Antitoxin – 20,000 to 1 lakh units • Antibiotic therapy – Penicillin • Carriers - Erythromycin Patch in the throat • • • • Diphtheria Streptococcal tonsillitis Oral thrush– Candida albicans Spirochete- Borrelia vincenti Other Corynebacteria 1. C. ulcerans: – – – Diphtheria like lesions Spread thru milk Antitoxin protective, erythromycin 2. C.minutissimum– Erythrasma 3. C. tenuis: - Trichomycosis axillaris 4. C.pseudotuberculosis: – Veterinary importance 5. C.parvum: – Immunomodulator 6. A. haemolyticum: – pharyngitis, skin ulcers 7. C.jakieum: – Skin inf/ BSI in IC. Rx- Vancomycin. Diphtheroids • Morphologically resembling diphtheria but do not cause any disease. • Present as commensals in throat, skin • Do not contain metachromatic granules. • Do not produce any toxin ie virulence test is negative. • C.hofmani, C.xerosis, C.pseudodiphtheriticum