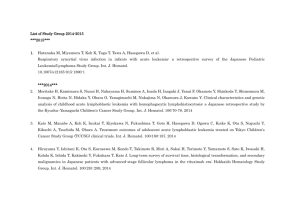
Table 17.1 Classification of acute lymphoblastic leukaemia (ALL
advertisement

Table 17.1 Classification of acute lymphoblastic leukaemia (ALL) according to the World Health Organization (WHO) classification (modified). Precursor lymphoid neoplasms B lymphoblastic leukaemia/lymphoma B lymphoblastic leukaemia/lymphoma, NOS B lymphoblastic leukaemia/lymphoma with recurrent genetic abnormalities B lymphoblastic leukaemia/lymphoma with t(9; 22)(q34; q11.2); BCR-ABL1 B lymphoblastic leukaemia/lymphoma with t(v; 11q23); MLL rearranged B lymphoblastic leukaemia/lymphoma with t(12; 21)(p13; q22); TEL-AML1 (ETV6-RUNX1) B lymphoblastic leukaemia/lymphoma with hyperdiploidy B lymphoblastic leukaemia/lymphoma with hypodiploidy (hypodiploid ALL) T lymphoblastic leukaemia/lymphoma NOS, not otherwise specified. Table 17.2 Specialized tests for acute lymphoblastic leukaemia (ALL). Cytochemistry Myeloperoxidase Sudan black Non-specific esterase Periodic acid–Schiff Acid phosphatase − − − + (coarse block positivity in ALL) + in T-ALL (Golgi staining) Immunoglobulin and TCR genes B-ALL: clonal rearrangement of immunoglobulin genes T-ALL: clonal rearrangement of TCR genes Chromosomes and genetic analysis (Table 17.1) Immunological markers (Table 17.3) (flow cytometry) B-ALL, B-cell acute lymphoblastic leukaemia; T-ALL, T-cell acute lymphoblastic leukaemia; TCR, T-cell receptor. Untitled-5.indd 35 2/8/2011 11:50:18 AM Table 17.3 Immunological markers for classification of acute lymphoblastic (ALL) leukaemia. Marker ALL B T B lineage CD19 cCD22 cCD79a CD10 cIg sIg TdT + + + + or − + (pre-B) − + − − − − − − + T lineage CD7 cCD3 CD2 TdT − − − + + + + + c, Cytoplasmic; S, surface. * B-ALL resembles precursor B-ALL immunologically but has surface immunoglobulin (Ig) and is terminal deoxynucleotidyl transferase negative (TdT−). Table 17.4 Prognosis in acute lymphoblastic leukaemia (ALL). Good Poor WBC Low High (e.g. >50 × 109/L) Sex Girls Boys Immunophenotype B-ALL T-ALL (in children) Age Child Adult (or infant <1 year) Cytogenetics Normal or hyperdiploidy; TEL rearrangement Ph+, 11q23 rearrangements MLL gene rearrangement Hypodiploidy (<44 chromosomes) Time to clear blasts from blood <1 week >1 week Time to remission <4 weeks >4 weeks CNS disease at presentation Absent Present Minimal residual disease Negative at 1 month (children) or 3 months (adults) Still positive at 3–6 months CNS, central nervous system; Ph+, Philadelphia chromosome positive; WBC, white blood cell count. Untitled-5.indd 36 2/8/2011 11:50:18 AM