Clinical Medicine: Therapeutics
Review
Open Access
Full open access to this and
thousands of other papers at
http://www.la-press.com.
A Review of Multimatrix System (MMX) Mesalazine
in the Management of Ulcerative Colitis
A Barney Hawthorne
Consultant gastroenterologist, University Hospital of Wales, Heath Park, Cardiff CF14 4XW, Wales UK.
Abstract: MMXTM mesalazine is a novel delayed release mesalazine formulation with a high-strength 1.2 g tablet for the treatment of
active mild to moderate colitis and maintenance of remission. In vitro and in vivo studies show initiation of drug release in the terminal
ileum and caecum with gradual release of 5-ASA as the tablet passes through the colon. Pharmacokinetic data are comparable to other
5-ASA formulations with low systemic absorption and high levels in feces and in mucosal biopsies in the left colon. Clinical trials have
shown high rates of clinical and endoscopic remission in active mild to moderate colitis over 8 weeks with a 2.4 g once daily dose. There
do not appear to be higher remission rates with the 4.8 g dose. Prolongation of treatment with a further 8 weeks of 2.4 g twice daily can
induce remission in those failing the initial 8 weeks of therapy. A maintenance study enrolling patients who achieved remission in the
acute studies showed high rates of remission maintained at one year with 1.2 g twice daily (68.5%) and 2.4 g once daily (64.4%) using
the strict definition of remission (including mucosal healing) that was used in the active treatment trials. The drug is safe and effective
in colitis. The high tablet strength, and once-daily dosage make this formulation a welcome addition to therapy options for patients with
colitis.
Keywords: mesalazine, ulcerative colitis, colonic-release
Clinical Medicine: Therapeutics 2009:1 1423–1436
This article is available from http://www.la-press.com.
© Libertas Academica Ltd.
This is an open access article distributed under the terms of the Creative Commons Attribution License
(http://www.creativecommons.org/licenses/by/2.0) which permits unrestricted use, distribution and reproduction
provided the original work is properly cited.
The authors grant exclusive rights to all commercial reproduction and distribution to Libertas Academica. Commercial
reproduction and distribution rights are reserved by Libertas Academica. No unauthorised commercial use permitted
without express consent of Libertas Academica. Contact tom.hill@la-press.com for further information.
Clinical Medicine: Therapeutics 2009:1
1423
Hawthorne
Mesalazine or 5-aminosalicylic acid (5-ASA)
remains the first-line therapy for treatment of mild to
moderately active ulcerative colitis, and maintenance
of mucosal healing. The drug exerts a topical antiinflammatory effect on colonic mucosa. Therapeutic
benefit of sulphasalazine was first described in 1942
by Svartz.1 Recently there has been a resurgence of
interest in several aspects of mesalazine use. There
is new information on mechanism of action through
peroxisome proliferator-activated receptor-γ (PPARγ)
receptors, effect on carcinogenesis, new technology
in drug delivery coatings to allow gradual release of
the drug after reaching the colon, and higher dose per
tablet, and a growing number of trials showing that once
daily dosing is as effective as divided doses. This review
discusses a new formulation of 5-ASA—multimatrix
(MMX) mesalazine: the evidence for its clinical
effect, pharmacokinetics, and safety in comparison
to other preparations of 5-ASA currently available.
Pharmacology
The clinical efficacy of sulphasalazine in ulcerative
colitis was a serendipitous discovery. The drug
was originally designed as a combination of an
antibacterial agent (sulphapyridine) linked to an antiinflammatory agent (5-ASA) by an azo bond, in order
to treat rheumatoid arthritis, at a time when it was
thought to have an infective as well as inflammatory
aetiology. It is ironic that the initial studies failed
to show the benefits of the drug in rheumatoid
arthritis (that subsequently were shown in larger
studies), but did show benefit in ulcerative colitis
patients in the rheumatoid arthritis trial, confirmed
in randomized controlled trials.2 Later studies in
distal colitis showed that the active agent was 5-ASA
rather than sulphapyridine,3 and that 5-ASA was
as effective as intact sulphasalazine and exerted a
topical effect on the colonic mucosa.4,5 Uncoated
5-ASA is rapidly and completely absorbed in the
proximal small intestine, but poorly absorbed from
the colon.6 It is metabolised to N-acetyl 5-ASA, by
N-acetyl-transferase 1 (NAT 1), present in intestinal
epithelial cells and liver. N-acetyl 5-ASA had no antiinflammatory activity in two of three trials.7–9 As the
sulphapyridine moiety was responsible for most of the
toxicity of sulphasalazine,10,11 it was logical to develop
coated forms of 5-ASA that were released in the colon.12
1424
Colonic release of 5-ASA
The first delayed-release 5-ASA tablet used a
pH-sensitive acrylic resin (Eudragit S) and was
developed and evaluated in Cardiff, and produced as
Asacol®.13 The resin dissolves at pH 7, and utilises
the fact that pH gradually rises through the small
intestine, to achieve pH 7 in the terminal ileum14
(Fig. 1). Since then a range of further coatings have
been developed to deliver drug to the colon using
other pH-sensitive resins (Claversal®, Mesasal®),
delayed-release microgranules using ethylcellulose
(Pentasa®), or alternative non sulfa-containing
prodrugs (balsalazide, olsalazine) (Table 1).
Pharmacokinetics
The pharmacokinetics of mesalazine have been
widely studied,15 but it is clear that plasma levels
do not necessarily reflect drug efficacy for a drug
with a topical effect on colonic mucosa. It is easy
to demonstrate significant variations in plasma
pharmacokinetic profiles, but it is not at all clear that
this correlates with drug efficacy, although there is
a great dearth of adequately powered comparative
studies. Plasma levels may be more important as
an indicator for potential nephrotoxicity. There is
however no evidence that drugs with more proximal
small bowel release and higher plasma levels are any
more toxic, and it seems more likely that interstitial
nephritis is either an idiosyncratic or hypersensitivity
reaction.15 Most of the pharmacokinetic studies
have been performed in healthy volunteers.
There is also evidence to show that patients with
quiescent ulcerative colitis have colonic motility and
8
7.5
7
pH
Introduction
6.5
6
5.5
5
proximal small
intestine
Distal small
intestine
caecum/Rt
colon
Left
colon/rectum
Figure 1. pH gradient along gastrointestinal tract in man.
Clinical Medicine: Therapeutics 2009:1
MMXTM mesalazine in ulcerative colitis
Table 1. Current Oral 5-ASA formulations.
Generic name
Proprietary name
Formulation
Site of release
Strength
Sulfasalazine
Azulfidine Salazopyrin
5-ASA and sulfapyridine
linked by azo-bond.
Tablet
Colon
500 mg
(200 mg 5-ASA)
Sulfasalazine
Azulfidine EN-tabs
Salazopyrin EN-tabs
As above, but tablet
coated with cellulose
acetate phthalate
Colon
500 mg
(200 mg 5-ASA)
Olsalazine
Dipentum®
5-ASA dimer linked
by azo-bond. Gelatin
capsule
Colon
250 mg
Olsalazine
Dipentum®
5-ASA dimer linked by
azo-bond. Tablet
Colon
500 mg
Balsalazide
Colazide®, Colazal®
5-ASA and
4-aminobenzoylβ-alanine (4ABA) linked
by azo-bond. Capsule
Colon
750 mg
(262 mg 5-ASA)
Mesalazine
N American Asacol®*
Eudragit-S coated
tablets (release at
pH 7)
Terminal ileum, colon
400 mg 800 mg
Mesalazine
United Kingdom, Italy,
Netherlands Asacol®*
Eudragit-S coated
tablets (release
at pH 7)
Terminal ileum, colon
400 mg 800 mg
Mesalazine
Ipocol®# Mesren®#
Eudragit-S coated
tablets (release
at pH 7)
Terminal ileum, colon
400 mg
Mesalazine
Salofalk® Mesasal®
Claversal®
Eudragit-L coated
tablets (release at
pH 6). Tablets,
granules
Distal ileum, colon
250 mg tablets 500 mg
and 1 g sachets
Mesalazine
Pentasa®
Ethylcellulose-coated
microgranules (timedependent release)
available as a tablet,
capsule or sachet
Duodenum, jejunum,
ileum, colon
500 mg tablet 1 g
and 2 g sachet
Mesalazine
Mezavant®
Eudragit-S coated tablet
containing inner core of
Multi-Matrix System □
Terminal ileum, colon
1.2 g
*North American Asacol® manufactured by the original Tillotts Laboratories process, whereas changes in manufacturing process of European Asacol® may
result in differences in thickness of coating and excipients. #Differences in manufacturing processes of generic tablets may result in differences in coating
and excipients making the release characteristics different to Asacol®. □ A matrix containing lipophilic and hydrophilic excipients.
function that is similar to healthy controls.16,17 The
pharmacokinetics of mesalazine should therefore
be the same in quiescent ulcerative colitis as in the
normal colon.
Need for novel 5-ASA delivery systems
There are a number of theoretical reasons to
develop novel 5-ASA delivery systems. The
ethylcellulose-coated and Eudragit-L coated
Clinical Medicine: Therapeutics 2009:1
preparations undoubtedly release 5-ASA higher in
the small intestine than Eudragit-S coatings.15 This
should result in higher plasma levels, and thus greater
urinary excretion of 5-ASA. In fact it is difficult to
demonstrate this in the numerous pharmacokinetic
studies, where interindividual variation is far
greater, but there is some evidence of greater total
urine 5-ASA for Claversal®, Salofalk® and Mesasal
compared to all the others.15 Faecal excretion is
1425
Hawthorne
however broadly similar for all preparations. The
only exception to this is the effect of administering
bisacodyl to volunteers to increase colonic transit and
cause diarrhoea.18 This resulted in a marked increase
in faecal excretion of the pro-drugs sulphasalazine
and olsalazine. This was more significant than
the increase in faecal loss of free 5-ASA when the
bisacodyl-treated volunteers were given Asacol® or
the other slow-release preparations. When comparing
UC patients with and without diarrhoea, a similar
increase in faecal loss of unsplit sulfasalazine
and olsalazine is found,19 but the amount of free
5-ASA (as a proportion of total free- and acetylated
5-ASA) rose most dramatically in diarrhoea patients
receiving Asacol® from 66% to 87%. In other words,
very little Asacol® was being acetylated in patients
with diarrhoea, and may link with observations of
patients that they pass intact or partially dissolved
tablets at times. The rise in proportion of free 5-ASA
in faeces was not as marked for Pentasa® or Salofalk®
with diarrhoea.19
An ideal drug delivery system would not release
drug at all in the upper small bowel, but start to
release the drug gradually in the ileocaecal region,
and then progressively throughout the colon. In this
way, unacetylated active drug would be available
through the colon. It is worth noting that the right
colon is generally thought to be a storage and mixing
organ and chyme is likely to travel back and forth
for some time in this area, as water is absorbed and
the consistency of stool gets more solid. Once a mass
action occurs, the stool then passes more rapidly
down the left colon before evacuation. The left colon
in normal patients, and certainly in active colitis, is
generally relatively empty, and represents a much
more challenging area for drug delivery.
Evaluation of intestinal release profiles
It is necessary therefore to evaluate the release
characteristics of these formulations in the gut. There
are two main techniques used to assess the rate of
dissolution of slow-release tablets, and the location in
the gut where this occurs. In vitro, the pH conditions
of the gut can be simulated by measuring the rate of
dissolution of tablet coatings in fluids at different
pHs. Systems have been developed to simulate more
accurately conditions in the normal gut, including
pH, body temperature, peristalsis, gut secretions,
1426
nutrient and water absorption and colonic microbiota.
An example is the TNO GastroIntestinal Model (TIM;
TNO Quality of Life, Zeist, The Netherlands).20 There
are of course limitations to these models as they cannot
completely simulate an organ whose function is still
so poorly understood. It is also clear from in vivo
magnetic resonance imaging of intestinal fluid along
the gut, that there are fluid pockets, separated by areas
of collapsed gut containing only minimal amounts of
secretions.21
The second, in vivo method,22 involves labelling
tablets with radioactive tracer (152Sm2O3) added
during tablet manufacture and then neutron-irradiated
to produce 153Sm2O3. Gamma scintigraphy can then
follow the dissolution of individual tablets after
oral ingestion, with measurement of radioactivity
in regions of interest plotted out on the basis of
typical anatomy (stomach, small intestine, ileocaecal,
ascending, transverse, descending colon and rectum).
The limitations of this technique are the complexity of
the incorporation of tracer into tablets, the possibility
that this may alter the release characteristics of
5-ASA, and the possibility that tracer release may
not accurately correspond to drug release. Variable
anatomy may also limit the accuracy of plotting
regions of interest in the gut.
MMXTM multimatrix system
Mesalazine with MMXTM multimatrix system
(MezavantTM, also known as Mezavant XLTM in the
UK and Ireland, and LialdaTM in the USA: Shire
Pharmaceuticals Inc, Wayne PA, USA, under licence
from Giuliani SpA, Milan, Italy) is a novel tablet
coating designed to release mesalazine gradually
throughout the colon. The outer coating is a gastroresistant Eudragit-S film that dissolves above pH 7
(usually in the terminal ileum). Within this is a core
of lipophilic and hydrophilic matrix. Once exposed to
intestinal fluid, this absorbs water to form a sponge-like
viscous gel mass, containing the drug. The lipophilic
elements creates a partially hydrophobic environment
in the core, and is expected to slow the penetration of
aqueous fluid into the tablet, and allowing the slow
diffusion out of the drug as it passes round the colon,
allowing contact of the drug with a larger surface
area of mucosa before conversion to n-acetyl 5-ASA.
The hydrophilic elements may promote adherence
to colonic mucosa. This proposed mechanism is
Clinical Medicine: Therapeutics 2009:1
MMXTM mesalazine in ulcerative colitis
thought to have the advantage of gradual 5-ASA
release through the colon. This review will discuss
the evidence that this occurs, and the clinical benefit
in relation to other preparations.
In vitro, dissolution of MMXTM mesalazine has been
studied in the TIM-1 and TIM-2 system (simulating
stomach and small intestine, and colorectum
respectively).23 In simulated fasting and fed conditions,
less than 1% of drug is released in stomach and small
intestine during a mean residence time of 5 hours
(fasted) and 6 hours (fed). Release of 78% (69%–87%)
occurred in the colon in the simulated fasting state
(over a mean 19 hours), but was 68% (61%–76%) in
the fed state (mean 18 hours residence). No sign of the
tablet was left in the colon residue. This model cannot
indicate what level in the colon the drug is released,
but measuring 5-ASA release in the colon dialysate
over time indicates a sigmoidal pattern, (slow rising
initially and then after a 2–3 hour lag, increasing
linearly to a peak of release at 6–8 hours (fasted) and
5–6 hours (fed). There are no comparative studies
with other 5-ASA preparations, but the results do
suggest that MMXTM release is gradual once the colon
is reached, in this in vitro model.
The in vivo release of MMXTM mesalazine has
been studied using gamma-scintigraphy. Brunner et al
studied 12 healthy volunteers using 153Sm2O3 labelled
tablets, and plasma pharmacokinetics.24 In fasting
single-dose studies, the mean gastric emptying time
was 0.4 ± 0.4 hours (hr), with appearance in the small
intestine at 0.8 ± 0.5 hr, ileum at 4 ± 1 hr and colon
at 5.8 ± 1.2 hr. Initial tablet disintegration started
at a mean of 6.9 ± 1.1 hr, in ascending (n = 8) or
transverse colon (n = 4). It was difficult to determine
time to complete dissolution, as there was a tail of
radioactivity behind the tablet on scintigraphic images.
Plasma levels peaked (Tmax) when tablets were in the
ileocaecal region. Plasma levels as area under curve
(AUC) were 12.37 nmol/ml, comparable to that of
other slow-release 5-ASA preparations and prodrugs.15 19.9 ± 18.2% of drug absorption occurred in
the ileal region, and 80.1 ± 18.2% in the colon. Urinary
excretion was measured for 24 hours, with a mean 9%
of administered dose excreted (almost all acetylated).
This is less than in studies with other drugs, with mean
values ranging from 11%–33% for sulfasalazine,
Asacol® 10%–35%, Pentasa® 15%–53%, and up
to 27%–56% for Salofalk®, Mesasal and Claversal®.15
Clinical Medicine: Therapeutics 2009:1
It should be noted however that the elimination process
was not complete at 24 hours (plasma concentrations
still significant at this point, and in some subjects,
the start of the decay phase had still not occurred).
Overall, the results suggest a low systemic availability
of 5-ASA with the MMXTM mesalazine tablet, and a
slower and more sustained release from the ileocaecal
region onwards through the colon.
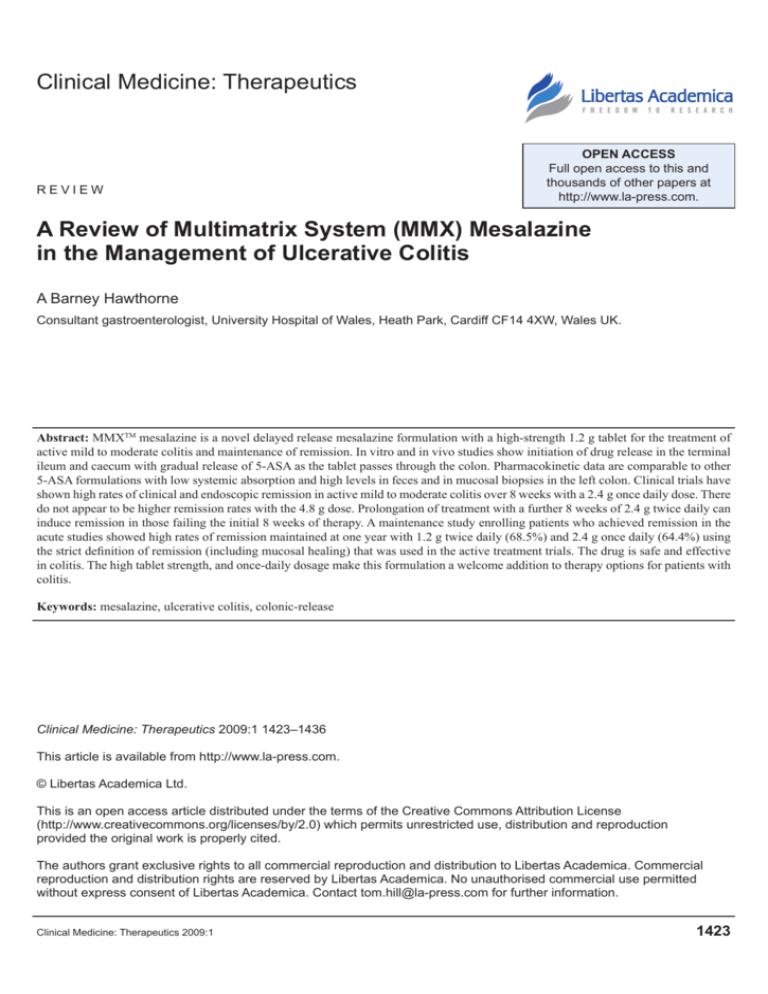
A small study has used the same scintigraphic
method to compare release of MMXTM mesalazine
and delayed-release mesalazine (Asacol® Giuliani,
S.p.A., Milan, Italy) in eight healthy volunteers in
a single-dose, two-way, cross-over design.25 Plasma
release of both tablets was very similar, with a
Tmax at approximately eight hours. Scintigraphy
showed initial disintegration slightly earlier for
MMXTM mesalazine (4.75 ± 1.3 hours) than Asacol®
(6.16 ± 1.8 hours). Complete disintegration was later
however for MMXTM mesalazine (17.4 ± 8.6 hours)
versus Asacol® (7.3 ± 2.1 hours). The location of
complete disintegration was also more distal for
MMXTM mesalazine (Fig. 2). These scintigraphic
studies demonstrate the variability in location of
tablet disintegration between individuals. Whether this
variability is greater between different preparations
is not clear.
In summary, both in vitro and in vivo studies
confirm that initial disintegration of MMXTM
mesalazine is in the ileocaecal region but subsequent
release is gradual through the colon.
Clinical trials of MMXTM mesalazine
(Table 2)
A small preliminary trial was carried out in five Italian
centres to evaluate the effect of MMXTM mesalazine
in active left-sided disease compared to 5-ASA
enemas.26 Patients had disease extending more than
15 cm but no further than splenic flexure and had
mild to moderate disease activity as determined by
a clinical disease activity (Rachmilewitz score) 6.27
This was an eight week double-blind double-dummy
trial comparing MMXTM mesalazine 1.2 g three times
daily plus placebo enema (n = 40) with Asacol®
4 g/100 ml enema with placebo tablets. The primary
end-point was remission at eight weeks, defined
by a Rachmilewitz score of 4. In the MMXTM
group, 60% achieved remission, versus 50% in the
enema group. This study showed that oral MMXTM
1427
Hawthorne
A
MMX mesalazine
Asacol
5
4
3
2
Dc
sF
Tc
HF
Ac
IcJ
DsB
MsB
0
psB
1
s
number of subjects
6
Region of gut
Active disease
B
MMX mesalazine
Asacol
5
4
3
2
Dc
sF
Tc
HF
Ac
IcJ
DsB
MsB
psB
1
s
number of subjects
6
0
Figure 2. Scintigraphic location of initial dissolution (Fig. 1a) and
Region of gut
complete tablet dissolution (Fig. 1b) for MMXTM mesalazine or Asacol®
tablets radiolabelled with 153Sm2O3 in 8 healthy volunteers given a single
tablet.36
Abbreviations: S, stomach; PSB, proximal small bowel; MSB, mid small
bowel; DSB, distal small bowel; ICJ, ileocaecal junction; AC, ascending
colon; HF, hepatic flexure; TC, transverse colon; SF, splenic flexure;
DC, descending colon.
mesalazine is as effective as enemas in left-sided
disease, confirming delivery of drug in significant
amounts to the left colon. A small dose-ranging pilot
study28 investigated the efficacy of three different
doses (1.2 g, 2.4 g and 4.8 g given once daily to
13, 14 and 11 patients respectively) in patients with
mild to moderate active UC (UC-DAI score 4–10)29
1428
extending beyond the rectum. The primary end-point
was remission at eight weeks as defined by a UC-DAI
score 1, with a zero score for rectal bleeding and
stool frequency and at least a one-point reduction
in sigmoidoscopy score from baseline. No patients
in the 1.2 g group achieved remission, versus
4 (30.8%) in the 2.4 g group and 2 (18.2%) in the
4.8 g group. There was however a dose-response
relationship in improvement in UC-DAI score, and
also in rectal and sigmoidoscopic histology scores.
Levels of 5-ASA and acetyl-5-ASA in colonic
mucosa were considerably higher in the 4.8 g group
(48.8 ng/mg and 29.7 ng/mg) compared to the 1.2 g
group (11.2 ng/mg and 6 ng/mg) and the 2.4 g group
(6.9 ng/mg and 7 ng/mg).
A large phase III double-blind parallel-group study
in 280 patients compared 1.2 g twice daily, versus
4.8 g daily versus placebo over eight weeks in mild to
moderate active UC.30 The trial used a modification of
the Sutherland UC-disease activity index (UC-DAI).
The index has a maximum score of 12 comprising
a score of 0–3 each for rectal bleeding, increased
stool frequency, sigmoidoscopic appearance and
physicians global assessment. The sigmoidoscopic
score was modified. In Sutherland’s sigmoidoscopic
score, normal scores 0, erythema, decreased vascular
pattern, or mild friability scores 1, and marked friability
scores 2, with ulceration and spontaneous bleeding
scoring 3. This was modified to make any degree
of friability give a score of 2. This has the effect of
making the score somewhat more objective, reducing
interobserver variability and indeed bringing it in
line with the original sigmoidoscopic score devised
by Baron.31 Mild to moderate disease was defined as
a score of 4–10, with the sigmoidoscopic score of
0 or more, and the physician’s global assessment as
2 or less. The relapse duration had to be less than six
weeks, and patients were excluded if they had relapsed
using more than 2 g mesalazine. The primary endpoint was clinical and endoscopic remission at eight
weeks (i.e. modified UC-DAI score 1, with a score
of 0 for rectal bleeding and stool frequency, and no
mucosal friability and at least a 1-point reduction in
sigmoidoscopy score. Using this stringent definition,
12.9% on placebo achieved remission, with 34.1%
in the 1.2 g twice daily, and 29.2% in the 4.8 g daily
Clinical Medicine: Therapeutics 2009:1
MMXTM mesalazine in ulcerative colitis
Table 2. Trials of MMXTM mesalazine in active UC and maintenance of remission.
Trial
Study population
Treatment arm
Number
treated
Primary end-point
Result
Significance
compared
to placebo
Prantera26
Mild-moderate
active left-sided
colitis
1.2 g three
times daily
40
60%
n/a
Asacol®
4 g/100 ml
enema
39
Remission at 8 wks
(Rachmilewitz CAI
score 4)
50%
n/a
Mild-moderate
active colitis
(proctitis excluded)
1.2 g daily
13
0%
n/a
2.4 g daily
14
30.8%
n/a
4.8 g daily
11
Remission at 8 weeks
(UC-DAI score 1
with score 0 for rectal
bleeding and stool
frequency and at
least 1-point reduction
from baseline
sigmoidoscopy score
18.2%
n/a
Mild-moderate
active colitis
(proctitis excluded)
Placebo
88
12.9%
1.2 g twice
daily
88
4.8 g daily
89
Remission at 8 weeks
(modified UC-DAI
score 1, with score
0 for rectal bleeding
and stool frequency,
no mucosal friability
and at least a 1-point
reduction from baseline
sigmoidoscopy score
Placebo
86
2.4 g daily
84
D’Haens28
Lichtenstein
et al30
Kamm
et al32
Kamm
et al33
Mild-moderate
active colitis
(proctitis excluded)
UC in remission
(proctitis excluded)
4.8 g daily
85
Asacol®
800 mg tid
86
1.2 g twice
a day
234
2.4 g daily
225
group (Table 2). There was no significant difference
between the doses.
A similar trial32 ran concurrently with this study,
and had the same entry criteria, definitions and endpoints. Patients were randomized to 2.4 g once daily,
4.8 g once daily, placebo, or a comparator group
of Asacol® 800 mg three times daily, all for eight
weeks. The latter tablets were over-capsulated with
a gelatine capsule to ensure blinding. The study was
not powered to detect a difference between MMXTM
mesalazine and Asacol®. In spite of such similar
Clinical Medicine: Therapeutics 2009:1
34.1%
P 0.001
29.2%
P 0.009
22.1%
“
Safety and tolerability
over 12 months
(Remission as defined
above for Lichtenstein
et al was secondary
end-point)
40.5%
P = 0.01
41.2%
P = 0.007
32.6%
P = 0.124
Remission at
12 mo 68.5%
n/a
Remission at
12 mo 64.4%
n/a
design, the rates of clinical and endoscopic remission
was higher than in the previous study at 22.1% in the
placebo group, rising to 40.5% in the 2.4 g group, and
41.2% in the 4.8 g daily group. The remission rate
in the Asacol® comparator group was 32.6%, which
was not statistically significant compared to placebo.
There were no significant safety concerns with either
of these studies, and together they show convincingly
that MMXTM mesalazine is an effective treatment for
mild or moderate colitis in a once daily dosage of
2.4 g, with no benefit from increasing to 4.8 g daily.
1429
Hawthorne
Maintenance of remission
A one year maintenance trial followed on for patients
in the above two trials of active colitis. This trial was
designed to assess safety and tolerability of MMXTM
mesalazine.33 For those achieving remission at the
end of the active treatment period, they could enrol
directly (n = 246), and for others they could receive
a further 8 weeks of 2.4 g MMXTM mesalazine twice
daily (312 patients, of whom 213 achieved remission
and were enrolled). These numbers included
approximately 20% who had not achieved the strict
definition of remission required in the index trials, but
were deemed well enough by the investigators to enter
the maintenance phase. Patients were re-randomized
to either 2.4 g daily, or 1.2 g twice a day. At one year,
there were 64.4% of patients in remission (using the
strict definition above) in the 2.4 g daily group, versus
68.5% in the 1.2 g twice a day group. When defined as
the absence of a relapse requiring additional treatment,
88.9% (once daily) and 93.2% (twice daily) remained
in remission. The differences between groups were
not significant. These results show high numbers
remaining in remission, (in comparison to other
maintenance studies), but it is worth remembering
that this is a selected population, who had not relapsed
previously on more than 2 g mesalazine, and who had
responded well in the active treatment trial.
Dose-response with 5-ASA
in Active Disease
To date, the evidence for dose-response in treatment
of colitis remains contentious. In theory, a higher dose
of 5-ASA might be more effective by saturating the
acetylating enzyme capacity in colonic mucosa, thus
increasing availability of the active free 5-ASA.34
The trials of MMXTM mesalazine to date do not
show an advantage of 4.8 g daily over 2.4 g in active
disease. This is in keeping with most of the literature
on 5-ASA. In the trial comparing 1.6 g Asacol® with
4.8 g, Schroeder et al35 found the higher dose more
effective. Sutherland, however, in his Cochrane
review meta-analysis,36 concluded that 1.6 g was
insufficient, and at least 2 g was needed, but it was not
possible to demonstrate a dose-response above this
level. In the Ascend I and II trials37,38 of 2.4 g versus
4.8 Asacol® over six weeks in mild to moderate colitis,
there was significant benefit of the higher dose only
evident in the moderate group (72% improvement
1430
with 4.8 g versus 59% with 2.4 g in Ascend II),
with no significant benefit in the mild colitis group.
In the Ascend III study,39 in spite of including
772 patients with moderately active disease, there
was a numerical increase from 66% improvement
with 2.4 g to 70% on 4.8 g. This benefit is of dubious
clinical significance. The MMXTM mesalazine studies
were not powered to demonstrate differences in the
dose regimens. A pooled analysis of the two large
active treatment trials do not show overall benefit
for the 4.8 g dose over 2.4 g.40 Three hundred and
four patients who did not achieve remission in the
two eight week MMXTM mesalazine studies,30,32
were given open-label MMXTM mesalazine 2.4 g
twice daily for a further eight weeks, as reported in
the maintenance study.33 Of these, 59.5% achieved
remission according to the stringent definition
used in the trials. When patients were separated
according to the initial treatment group they had
been in, there was no difference in remission rates:
the placebo group had 57% remission, 2.4 g MMXTM
mesalazine 61.5%, 4.8 g MMXTM mesalazine 60.3%
and the Asacol® 2.4 g group 61% remission after
the eight week extension. The implication is that it
is the prolongation of treatment, rather than the switch
to high dose, that achieved remission. In conclusion,
there is no evidence that doses of MMXTM mesalazine
above 2.4 g daily have greater efficacy.
Safety and Tolerability
In the literature, 5-ASA is recognised as an
extremely safe drug, with headaches and nausea
being the commonest side-effects. In the trials of
MMXTM mesalazine to date, no significant safety
concerns have arisen. In the D’Haens28 study,
headache was the commonest adverse event,
occurring in 21% of patients. This was also reported
in the other trials,26,28,30,32,33 but no more commonly
in the active treatment than in the placebo groups,
and there was no evidence of a dose response—i.e.
no increase in frequency in the high-dose or once
daily dose groups. Overall, gastrointestinal sideeffects were the commonest, again no more
common than in the placebo group. Two cases of
pancreatitis occurred (one on 2.4 g and one on 4.8 g
daily), a documented side-effect of 5-ASA.41 Both
resolved on withdrawal of medication. One patient
developed a hepatitis, but a subsequent infectious
Clinical Medicine: Therapeutics 2009:1
MMXTM mesalazine in ulcerative colitis
mononucleosis test was positive, and glandular
fever the likely cause.
No renal failure or interstitial nephritis was
recorded in the 723 patients in the MMXTM mesalazine
trials to date. Interstitial nephritis is recognised as
a complication of mesalazine treatment and exact
frequency is unknown. Renal impairment (elevated
creatinine) was found in 0.2% in a large study involving
2940 patients.42 In one study of 223 IBD patients,43
microalbuminuria was found in up to a third of patients
treated with doses of more than 3 g daily, and appeared
to be dose-dependent. A UK review of reports to
the Committee on Safety in Medicines (CSM) from
1991–8 (2.8 million prescriptions for mesalazine,
4.7million for sulfasalazine) found 11.1 reports per
million prescriptions for mesalazine, but none for
sulfasalazine.44 Even considering the incomplete
nature of adverse event notifications through this
system, the disparity implies that the higher plasma
levels seen with delayed-release 5-ASA15 are relevant
in causing renal damage, although they are still at least
10-fold lower than salicylate levels in patients taking
aspirin. Other renal complications of untreated IBD
include tubular proteinuria, renal calculi, amyloidosis
and glomerulonephritis, and it has been proposed
that interstitial nephritis could also be related to
the underlying IBD (more severe disease likely to
require higher doses of 5-ASA). However, it is well
recognised that early withdrawal of 5-ASA results
in resolution of the renal function, providing strong
evidence that this is a drug-related hypersensitivity.
If mesalazine-induced interstitial nephritis is not
recognised, then permanent renal impairment is
likely to result.45 In conclusion, renal toxicity from
5-ASA does occur, but is rare, and as yet there is no
strong evidence that it is dose-dependent. There is no
evidence of differences in risk, either with different
5-ASA colonic-release mechanism, nor with oncedaily therapy.
There is evidence that 5-ASA inhibits thiopurine
methyltransferase in vitro, and so could potentially
affect metabolite levels of azathioprine and
6-mercaptopurine.46 In theory higher levels could
have a more pronounced effect, with more thioguanine
nucleotides, responsible for marrow suppression.
A study comparing 2 g with 4 g doses of mesalazine
for 4 weeks however showed no significant
difference in thioguanine nucleotide levels, although
Clinical Medicine: Therapeutics 2009:1
6 methylmercaptopurine levels were significantly
lower on the high dose.47 High-dose mesalazine could
in theory enhance the effectiveness, and also toxicity
of coprescribed thiopurines, but in reality this effect
is likely to be non-clinically significant.
Once Daily Therapy with 5-ASA
In the past it was assumed that divided dosing
would maximise the time that drug would spend in
contact with colonic mucosa and this would improve
efficacy, but this has never been shown to be true.
With a growing interest in treatment adherence, once
daily therapy is an important consideration, if it could
be shown to be as safe and as effective as divided
doses. A study in Sheffield of steady state plasma
pharmacokinetics (after 7 days) showed that in
normal subjects, median peak concentrations, trough
concentrations, and areas under the curve were similar
for once-daily and three-times-daily mesalazine
dosing regimens using Asacol®.48 Urine and fecal
5-ASA 24 hour collections were also similar, as were
levels in rectal biopsies. This implies that safety is
not a concern, (albeit with a maximum daily dose
of only 2.4 g). The study was not able to measure
peak levels in the colonic lumen, which might have
therapeutic relevance. A computer simulation model
of 5-ASA levels in segments of the colon predicts
that both total and regional levels would be similar
after once daily, and three times daily dosing with
Asacol®.49 The same model did predict that levels
in sigmoid colon and rectum would be considerably
lower than in the right colon with Asacol®, and this
difference would be exacerbated by frequent bowel
actions, as in active colitis.
A pilot feasibility study of once daily (Asacol®,
using 400 mg tablets) versus conventional dosing
of mesalazine for the maintenance of remission of
ulcerative colitis, was the first study to investigate
once daily dosing.50 Over six months, there was one
relapse in the 12 patients on daily dosing (average
2.5 g daily) versus one relapse among the 10 patients
taking an average 2.7 g per day either in twice daily
or three times daily administration (Table 3). The
authors concluded that a larger trial was warranted.
Four of the MMXTM mesalazine trials to date have
included once daily arms,28,30,32,33 and have confirmed
that once daily dosing is as effective as divided doses,
both in active disease and maintenance of remission.
1431
Hawthorne
Table 3. Trials of once-daily 5-ASA therapy (MMXTM mesalazine trials shown in Table 2).
Trial
Study population
Treatment arm
Number Primary
treated end-point
Result
Kane et al50
UC in remission
Asacol® once daily
in usual dose
(mean 2.5 g daily)
12
1/12 (8%) n/a
relapse
Asacol® in usual
twice or three
times daily dosing
(mean daily
dose 2.7 g)
10
1/10
(10%)
relapse
Salofalk® granules
3 g once daily
191
Remission
79%
Non-inferiority
(CAI 4 at
remission confirmed
week 8 (last
observation
carried forward))
Salofalk® granules
1 g three times
daily
189
Pentasa® granules
2 g once daily
169
Pentasa® granules
1 g twice daily
184
Kruis et al51
Dignass et al53
Active UC (excluding
proctitis) with clinical
activity index 4 and
endoscopic index 4
(Rachmilewitz) REF
UC in remission based
on UC-DAI score 2
(excluding proctitis)
The 1.2 g MMXTM tablet has made it easier to dose
once daily with a small number of tablets. These
studies were powered to compare each dose regimen
with placebo, and were not designed to demonstrate
non-inferiority of once daily compared to divided
doses.
Two further studies have now been completed using
5-ASA granules that were designed as non-inferiority
studies. Eudragit-L coated 5-ASA (Salofalk®) in the
form of granules was investigated in active UC by
Kruis et al51 in a single-blind study. Of 381 patients
enrolled, 347 completed the study, which used
the Rachmilewitz CAI index27 4 as the primary
end-point. 79% patients treated with 3 g once daily
achieved remission, compared to 75.7% in the 1 g t.i.d.
arm. The confidence interval for the difference was
3.4% [95% confidence interval (CI) -5.0%–11.8%].
Using the same end-point as in the MMXTM mesalazine
trials (modified DAI score 1 with score 0 for rectal
bleeding and stool frequency and at least 1-point
reduction from baseline sigmoidoscopy score),30 the
1432
n/a (pilot study)
Significance
75.7%
remission
Remission
rate at 1 yr
(UC-DAI 2)
analysed by
Kaplan-Meier
method
70.9%
Once daily
remission superior
(p = 0.024)
58.9%
remission
once daily group achieved 37% remission, versus
39% in the t.i.d. group. These figures are virtually the
same as the two MMXTM mesalazine active colitis
trials.32,33 The Kruis trial results also showed that in
patients treated with once daily 3 g, those with distal
disease had statistically better outcomes than those
with more extensive disease, and also did better
than those with distal disease treated with 1 g t.i.d.
This was an exploratory analysis, and is most likely
to have arisen by chance, but the authors speculated
that the difference could be explained by once daily
therapy giving intermittent high 5-ASA levels in the
distal colon.
A pharmacokinetic study in 30 healthy volunteers
had shown bioequivalence for once versus twice
daily administered 4 g of ethylcellulose-coated
5-ASA.52 In the Podium trial,53 the investigators
evaluated the clinical effectiveness of a granule
preparation of Pentasa® for maintenance of remission
in a single-blind non-inferiority designed study. The
study used the UC-DAI score,29 and patients enrolled
Clinical Medicine: Therapeutics 2009:1
MMXTM mesalazine in ulcerative colitis
had to have a score of 2, with proctitis patients
excluded. Patients taking 2 g Pentasa® granules once
daily (n = 169) did better with 70.9% remaining in
remission at 1 year, than the 184 patients taking
1 g bd. Although designed as a non-inferiority study,
the outcome was in fact statistically superior for the
2 g daily dose (p = 0.024). Using Cox regression
analysis, the difference related to the improved
adherence in the once daily dosing group. An
economic analysis showed that once daily treatment
was cost-saving in this trial, mainly due to reduced
relapse rate.54
Adherence
In the controlled environment of clinical trials, with
a high level of medical supervision, approximately
70%–95% of IBD patients adhere to their
medication.55,56 However, this high rate of medication
adherence is not reflected in normal clinical practice.
A cross sectional study of US outpatients with quiescent
UC found that only 40% were adherent to maintenance
mesalazine therapy.56 Several community-based
studies have reported non-adherence rates ranging
from 43% to 72% of IBD patients.57 In the UK,
approximately 15% of patients fail to even redeem
prescriptions at the pharmacist.58 Treatment nonadherence rates vary considerably between countries
(in Europe, a survey of 203 IBD patients revealed
self-reported non-adherence rates ranging from 13%
to 46%).59 The implications are extensive, with good
evidence of higher relapse rates in non-adherent
patients,60 and evidence that non-continuation of
long-term 5-ASA increases colorectal cancer risk.61
Non-adherence is likely to result in a significant
increase in treatment costs.62 Poor adherence is
strongly linked to complex dosage regimens.63 In a
study involving 105 hypertensive patients receiving
long-term treatment, once daily (od) or twice daily (bd)
dosing was associated with significant improvements
in mean adherence rates compared with 3-times daily
(tds) dosing,64 and many other reviews confirm that
od and bd dosing is associated with better adherence
than more frequent dosing.64 It is more difficult to
show the small benefit increment from switching
from bd to od dosing.65
It is evident that non-adherence during maintenance
therapy for quiescent disease is far more likely than
in active disease. In the Podium trial of maintenance
Clinical Medicine: Therapeutics 2009:1
once daily therapy with Pentasa® granules,53
adherence was recorded by medication returns.
This was higher for the once daily (versus twice
daily) group, but not statistically significant. In a
validated questionnaire, patients in the twice daily
group reported higher rates of forgetting medication,
or carelessness about their medication. Visual
analogue scores showed significantly improved
acceptability for once daily. In a multivariate
analysis, treatment adherence was a significant
factor in improving outcome over one year, whereas
the dosing regimen was no longer significant. In the
Salofalk® granule study of once daily versus three
times daily therapy in active UC,51 adherence was
not specifically assessed, but on questioning, 82%
of patients preferred once daily dosing, compared
to only 2% preferring three times daily. In the
MMXTM mesalazine acute studies evaluating once
daily therapy,30,32 the studies were double-blind
and double-dummy, so the once daily groups were
still taking multiple daily tablets and differences
in adherence were not noted. In the maintenance
MMXTM mesalazine trial33 which was open-label,
there was no difference in treatment adherence
(recorded on pill counts as adherent if 80% of
medication taken), with 93.3% adherence in the
once-daily group and 99.6% in the twice-daily
group. In summary, adherence is greatly improved
when dosage can be given once or twice daily, but
the difference between once and twice daily is not
significant. It is likely that patient preference may
be the most important factor, and the freedom to
take medication once or twice daily is an advantage,
and may be a factor in quality of life.
Quality of Life
In ulcerative colitis, disease symptoms are the
main determinant of quality of life (QOL) at any
one time.66 In an eight week trial comparing 1 g,
2 g and 4 g Pentasa® or placebo in active UC,
quality of life was evaluated in 374 patients, and
was significantly improved compared to placebo
in the 2 g and 4 g dose groups.67 The benefit was
seen in all 12 QOL parameters, including five
disease-specific parameters (e.g. trips to the toilet or
urgency) and seven general QOL parameters (e.g.
ability to sleep, sexual relationships, or hobbies/
recreations). Effective medication is thus a vital
1433
Hawthorne
tool in improving QOL. In a qualitative study of
IBD patient experiences,68 over two thirds identified
medication as necessary in controlling symptoms,
in spite of being a nuisance, a concern regarding
toxicity, and anti-drug feelings. Two-thirds of the
patients also reported a desire to self-manage their
medication. In the Podium study,53 health-related
utility was measured, and was strongly linked to
disease severity,69 and although not different between
once-daily and divided dose groups, the option of
once-daily dosing is likely to lead to higher quality
of life if relapse rates are lower.
Conclusions
MMXTM mesalazine is a novel 5-ASA delivery tablet
that starts to release the drug in the terminal ileum
and caecum, and then allows the slow release of drug
during passage through the colon. The theoretical
advantages of this formulation are borne out in the
clinical trial data. In mild and moderate colitis these
show high rates of remission and mucosal healing in
clinical trials with stringent end-points. Once daily
dosing is as effective as divided doses, and the 2.4 g
dose appears as effective as 4.8 g daily. Although
the clinical trials included Asacol® as a comparator,
there are no adequately powered non-inferiority or
superiority trials to show that MMXTM mesalazine
is more effective than other 5-ASA preparations, but
the drug has the advantage of a high strength 1.2 g
tablet and well-designed trials showing high clinical
and endoscopic remission rates in active disease
and maintenance of remission with once-daily
therapy. It is becoming clear that once daily therapy
is effective for other formulations of 5-ASA, and
this benefit is not exclusive to MMXTM mesalazine.
Other considerations, particularly cost and patient
preference, must be taken into consideration in
choosing a formulation for individual patients, but there
is no doubt that this drug is a welcome addition to the
therapeutic armamentarium.
Disclosure
Dr Hawthorne has received honoraria and participated
in continuing medical educational events supported
by Shire Pharmaceuticals Inc, Proctor and Gamble,
Ferring Pharmaceuticals, and Dr Falk Pharma,
and received research funding from Proctor and
Gamble.
1434
References
1. Svartz N. Salazopyrin, a new sulfanilamide preparation: A. Therapeutic
results in rheumatic polyarthritis: B. Therapeutic results in ulcerative
colitis: C. Toxic manifestations in treatments with sulfanilamide preparation.
Acta Medica Scandinavia. 1942;110:557–90.
2. Baron JH, Connell AM, Lennard-Jones JE, et al. Sulphasalazine and
salicylazosulphadimidine in ulcerative colitis. Lancet. 1962;I:1094–6.
3. Azad Khan AK, Piris J, Truolove SC. An experiment to determine the active
therapeutic moiety of sulphasalazine. Lancet. 1977;II:892–5.
4. Van Hees PA, Bakker JH, van Tongeren JH. Effect of sulphapyridine,
5-aminosalicylic acid, and placebo in patients with idiopathic proctitis:
a study to determine the active therapeutic moiety of sulphasalazine. Gut.
1980;21:632–5.
5. Klotz U, Maier K, Fischer C, et al. Therapeutic efficacy of sulfasalazine and
its metabolites in patients with ulcerative colitis and Cron’s disease. N Engl
J Med. 1980;303:1499–502.
6. Schroder H, Campbell DE. Absorption, metabolism, and excretion of
salicylazosulfapyridine in man. Clin Pharmacol Ther. 1972;13:539–51.
7. Willoughby CP, Piris J, Truelove SC. The effect of topical N-acetyl
5-aminosalicylic acid in ulcerative colitis. Scand J Gastroenterol.
1980;15:715–9.
8. Binder VS, Halskov E, Hvidberg E, et al. A controlled study of
5-acetaminosalicylic acid (5-Ac-ASA) as enema in ulcerative colitis.
Scand J Gastroenterol. 1981;16:1122.
9. Van Hogezand RA, van Hees PA, van Gorp JP, et al. Double-blind
comparison of 5-aminosalicylic acid and acetyl-5-aminosalicylic acid
suppositories in patients with idiopathic proctitis. Aliment Pharmacol Ther.
1988;2:33–40.
10. Das KM, Eastwood MA, McManus JP, Sircus W. Adverse reactions during
salicylazosulfapyridine therapy and the relation with drug metabolism and
acetylator phenotype. N Engl J Med. 1973;289:491–5.
11. Taffet SL, Das KM. Sulfasalazine. Adverse effects and desensitization.
Dig Dis Sci. 1983;28:833–42.
12. Dew MJ, Hughes PJ, Lee MG, Evans BK, Rhodes J. An oral preparation
to release drugs in the human colon. Br J Clin Pharmacol. 1983;16:
738–40.
13. Dew MJ, Hughes P, Harries AD, Williams G, Evans BK, Rhodes J.
Maintenance of remission in ulcerative colitis with oral preparation of
5-aminosalicylic acid. Br Med J. 1982;285:1012.
14. Nugent SG, Kumar D, Rampton DR, Evans DF. Intestinal luminal pH in
inflammatory bowel disease: possible determinants and implications for
therapy with aminosalicylates and other drugs. Gut. 2001;48:571.
15. Sandborn WJ, Hanauer SB. Systematic review: the pharmacokinetic
profiles of oral mesalazine formulations and mesalazine pro-drugs
used in the management of ulcerative colitis. Aliment Pharmacol Ther.
2003;17:29–42.
16. Rao SS, Read NW, Brown C, Bruce C, Holdsworth CD. Studies on the
mechanism of bowel disturbance in ulcerative colitis. Gastoenterol.
1987;93:934–40.
17. Rao SS, Read NW. Gastrointestinal motility in patients with ulcerative
colitis. Scand J Gastroenterol Suppl. 1990;172:22–8.
18. Rijk MC, van Hogezand RA, van Schaik A, van Tongeren JH. Disposition
of 5-aminosalicylic acid from 5-aminosalicylic acid-delivering drugs during
accelerated intestinal transit in healthy volunteers. Scand J Gastroenterol.
1989;24:1179–85.
19. Rijk MCM, van Schaik A, van Tongeren HM. Disposition of mesalazine
from mesalazine-delivering drugs in patients with inflammatory bowel
disease, with and without diarrhoea. Scand J Gastroenterol. 1992;27:
863–8.
20. Minekus M, Smeets-Peeters M, Bernalier A, et al. A computer-controlled
system to simulate conditions of the large intestine with peristaltic mixing,
water absorption and absorption of fermentation products. Appl Microbiol
Biotechnol. 1999;53:108–14.
21. Schiller C, Frohlich CP, Giessmann T, et al. Intestinal fluid volumes and
transit of dosage forms as assessed by magnetic resonance imaging. Aliment
Pharmacol Ther. 2005;22:971–9.
Clinical Medicine: Therapeutics 2009:1
MMXTM mesalazine in ulcerative colitis
22. Davis SS, Hardy JG, Newman SP, Wilding IR. Gamma scintigraphy in
the evaluation of pharmaceutical dosage forms. Eur J Nucl Med. 1992;
19:971–86.
23. Tenjarla S, Romasanta V, Zeijdner E, Villa R, Moro L. Release of
5-aminosalicylate from an MMXTM mesalamine tablet during transit
through a simulated gastrointestinal tract system. Advances in therapy.
2007;24:826–40.
24. Brunner M, Assandr R, Kletter K, et al. Gastrointestinal transit and 5-ASA
release from a new mesalazine extended release formulation. Aliment
Pharmacol Ther. 2003;17:395–402.
25. Wray H, Joseph RE, Palmen M, Pierce D. A pharmacokinetic and
scintigraphic comparison of MMXTM mesalamine and delayed-release
mesalamine. Poster presented at the American College of Gastroenterology
Meeting, Orlando, Fl, USA 3–8 Oct 2008.
26. Prantera C, Viscido A, Biancone L, Francavilla A, Giglio L, Campieri M.
A new oral delivery system for 5-ASA: preliminary clinical findings for
MMx. Infl Bowel dis. 2005;11:421–7.
27. Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus
sulphasalazine in the treatment of active ulcerative colitis: a randomised
trial. Br Med J. 1989;298:82–6.
28. D’Haens G, Hommes D, Engels L, et al. Once daily MMXTM mesalazine
for the treatment of mild-to-moderate ulcerative colitis: a phase II,
dose-ranging study. Aliment Pharmacol Ther. 2006;24:1087–97.
29. Sutherland LR, Martin F, Greer S, et al. 5-aminosalicylic acid enema in
the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis.
Gastroenterol. 1987;92:1894–8.
30. Lichtenstein GR, Kamm MA, Boddu P, et al. Effect of once- or twicedaily MMXTM mesalamine (SPD476) for the induction of remission of
mild to moderately active ulcerative colitis. Clin Gastroenterol Hepatol.
2007;5:95–102.
31. Baron H, et al. Variation between observers in describing mucosal
appearances in proctocolitis. BMJ. 1964;1:89–92.
32. Kamm MA, Sandborn WJ, Gassull M, et al. Once-daily, high-concentration
MMXTM mesalamine in active ulcerative colitis. Gastroenterol.
2007;132:66–75.
33. Kamm MA, Lichtenstein GR, Sandborn WJ, et al. Randomised trial of
once- or twice-daily MMX™ mesalazine for maintenance of remission in
ulcerative colitis. Gut. 2008;57:893–902.
34. De Vos M, Verdievel H, Schoonjans R, et al. Concentrations of 5-ASA and
Ac-5-ASA in human ileocolonic biopsy homogenates after oral 5-ASA
preparations. Gut. 1992;33:1338–42.
35. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic
acid therapy for mildly to moderately active ulcerative colitis. A randomized
study. N Engl J Med. 1987;317:1625–9.
36. Sutherland L, Macdonald JK. Oral 5-aminosalicylic acid for induction
of remission in ulcerative colitis. Cochrane Database Syst Rev. 2006;3:
CD000543.
37. Hanauer S, Sandborn W, Kornbluth A, et al. Delayed-release oral
mesalamine at 4.8 g/day (800 mg tablet) for the treatment of moderately
active ulcerative colitis: the ASCEND II trial. Am J Gastroenterol. 2005;100:
2478–85.
38. Hanauer SB, Sandborn WJ, Dallaire C, et al. Delayed-release oral
mesalamine 4.8 g/day (800 mg tablets) compared to 2.4 g/day (400 mg
tablets) for the treatment of mildly to moderately active ulcerative colitis:
The ASCEND I trial. Can J Gastroenterol. 2007;21:827–34.
39. Sandborn WJ, et al. DDW2008. GE. 2008;134 S1:A99.
40. Sandborn WJ, Kamm MA, Lichtenstein GR, Lynes A, Butler T, Joseph RE.
MMXTM Multi Matrix System mesalazine for the induction of remission in
patients with mild-to-moderate ulcerative colitis: a combined analysis of two
randomized, double-blind, placebo-controlled trials. Aliment Pharmacol
Ther. 2007;26:205–15.
41. Bergholm U, Langman M, Rawlins M, et al. Drug-induced acute pancreatitis.
Pharmacoepidemiol Drug Safety. 1995;4:329–34.
42. Hanauer SB, Verst-Brasch C, Regalli G. Renal safety of long-term
mesalamine therapy in inflammatory bowel disease. Gastroenterol.
1997;112(suppl)A991.
Clinical Medicine: Therapeutics 2009:1
43. Schreiber S, Hamling J, Zehnter E, et al. Renal tubular dysfunction in
patients with inflammatory bowel disease treated with aminosalicylate. Gut.
1997;40:761–6.
44. Ransford RAJ, Langman MJS. Sulphasalazine and mesalazine: serious
adverse reactions reevaluated on the basis of suspected adverse reaction
reports to the Committee on Safety of Medicines. Gut. 2002;51:
536–9.
45. Tadic M, Grgurevic I, Scukanec-Spoljar M, et al. Acute interstitial nephritis
due to mesalazine. Nephrology. 2005;10:103–5.
46. Gilissen LDL, Bierau J, Derijks LJJ, et al. The pharmacokinetic effect
of discontinuation of mesalazine on mercaptopurine metabolite levels
in inflammatory bowel disease patients. Aliment Pharmacol Ther. 2005;
22:605.
47. Graaf PD, de Boer N, Jharap B, Mulder CJ, van Bodegraven AA, Schwab M.
Alteration of Thiopurinephosphate Metabolite Levels By Aminosalicylates
in IBD-Patients. Gastroenterol. 2008;134(suppl 1):A69.
48. Hussain FN, Ajjan RA, Kapur K, Moustafa M, Riley SA. Once versus
divided daily dosing with delayed-release mesalazine: a study of tissue
drug concentrations and standard pharmacokinetic parameters. Aliment
Pharmacol Ther. 2001;15:53–62.
49. Thorpe MP, Ehrenpreis ED, Putt KS, Hannon B. A dynamic model of
colonic concentrations of delayed-release 5-aminosalicylic acid (Asacol).
Aliment Pharmacol Ther. 2009;29:1193–201.
50. Kane S, Huo D, Magnanti K. A pilot feasibility study of once daily versus
conventional dosing mesalamine for maintenance of ulcerative colitis.
Clin Gastroenterol Hepatol. 2003;1:170–3.
51. Kruis W, Kiudelis G, Racz I, et al. Once-daily versus three-timesdaily mesalazine granules in active ulcerative colitis: a double-dummy,
randomised non-inferiority trial. Gut. 2008: epub.
52. Gandia P, Idier I, Houin G. Is once-daily mesalazine equivalent to the
currently used twice daily regimen? A study performed in 30 healthy
volunteers. J Clin Pharmacol. 2007;47:334–42.
53. Dignass AU, Bokemeyer B, Adamek H, et al. Mesalamine once daily is
more effective than twice daily in patients with quiescent ulcerative colitis.
Clin Gastroenterol Hepatol. 2009. In press.
54. Connolly M, Nielsen SK, Currie CJ, Poole CD, Travis SPL. Once daily
mesalazine for maintaining remission is cost-saving compared to twice
daily mesalazine: an economic evaluation based on the Podium randomised
controlled trial. Gut. 2008;57(suppl II):A261.
55. Kane SV, Cohen RD, Aikens JE, Hanauer SB. Prevalence of non-adherence
with maintenance mesalamine in quiescent ulcerative colitis. Am J
Gastroenterol. 2001;96(10):2929–33.
56. Kane SV. Systematic review: adherence issues in the treatment of ulcerative
colitis. Aliment Pharmacol Ther. 2006;23:577–85.
57. Rubin G, Hungin AP, Chinn D, et al. Long-term aminosalicylate therapy
is under-used in patients with ulcerative colitis: a cross-sectional survey.
Aliment Pharmacol Ther. 2002;16(11):1889–93.
58. Beardon PH, McGilchrist MM, McKendrick AD, et al. Primary
non-compliance with prescribed medication in primary care. BMJ.
1993;307(6908):846–8.
59. Robinson A. Patient-reported compliance with 5-ASA drugs in inflammatory
bowel disease: a multi-national study. Gastroenterology. 2002;122(4):
A-499.
60. Kane S, Huo D, Aikens J, et al. Medication non-adherence and outcomes of
patients with quiescent ulcerative colitis. Am J Med. 2003;114:39–43.
61. Moody GA, Jayanthi V, Probert CS, et al. Long-term therapy with
sulphasalazine protects against colorectal cancer in ulcerative colitis:
a retrospective study of colorectal cancer risk and compliance with treatment
in Leicestershire. Eur J Gastroenterol Hepatol. 1996;8(12):1179–83.
62. Review article: medication non-adherence in ulcerative colitis—
strategies to improve adherence with mesalazine and other maintenance
therapies. Hawthorne AB, Rubin G, Ghosh S. Aliment Pharmacol Ther.
2008;27:1157–66.
63. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations
between dose regimens and medication compliance. Clin Therapeutics.
2001;23(8):1296–310.
1435
Hawthorne
64. Eisen SA, Miller DK, Woodward RS, et al. The effect of prescribed
daily dose frequency on patient medication compliance. Arch Int Med.
1990;150:1881–4.
65. Greenberg RN. Overview of patient compliance with medication dosing:
a literature review. Clin Ther. 1984;6(5):592–9.
66. Han, et al. Inflamm Bowel. Dis. 2005;11:24–34.
67. Robinson M, Hanauer S, Hoop R, Zbrozek A, Wilkinson C. Mesalamine
capsules enhance the quality of life for patients with ulcerative colitis.
Aliment Pharmacol Ther. 1994;8:27–34.
68. Hall NJ, Rubin GP, Dougall A, Hungin APS, Neely J. The fight for
‘health-related normality’: a qualitative study of the experiences of
individuals living with established inflammatory bowel disease (IBD).
J Health Psychology. 2005;10:443–55.
69. Poole CD, Nielsen SK, Currie CJ, Marteau P. Quality of life (health-related
utility) in adults with ulcerative colitis in remission vs. mild/moderate
and severe relapse: findings from the Podium study. Gut. 2008;
57(suppl II):A260.
Publish with Libertas Academica and
every scientist working in your field can
read your article
“I would like to say that this is the most author-friendly
editing process I have experienced in over 150
publications. Thank you most sincerely.”
“The communication between your staff and me has
been terrific. Whenever progress is made with the
manuscript, I receive notice. Quite honestly, I’ve
never had such complete communication with a
journal.”
“LA is different, and hopefully represents a kind of
scientific publication machinery that removes the
hurdles from free flow of scientific thought.”
Your paper will be:
•
Available to your entire community
free of charge
•
Fairly and quickly peer reviewed
•
Yours! You retain copyright
http://www.la-press.com
1436
Clinical Medicine: Therapeutics 2009:1