Cath Lab Digest - Crouse Hospital
advertisement

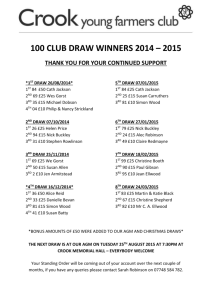
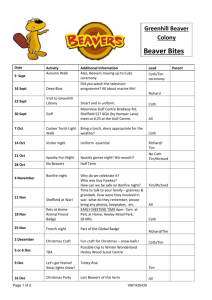
® Tom Lassar, MD: Platelet Function Testing at University Hospitals page 32 Clinical Editor’s Corner – Morton Kern, MD Serial Lesion FFR Made Simple page 4 www.cathlabdigest.com ® CASE REPORT & INTERVIEW Cath Lab Spotlight Treatment of Severe Coronary Artery Disease in a Diabetic Patient Using the Resolute Integrity Stent: A Case Study Ronald P. Caputo, MD, FACC, FSCAI, Director of Cardiac Services, St. Joseph’s Hospital, Syracuse, New York Lorissa Plis DNP, RN with the cath lab team. Crouse Hospital Lorissa Plis, DNP, RN, CNS, CCNS, CCPC, Manager Cardiac Care Center & Chest Pain Center Coordinator, Crouse Hospital, Syracuse, New York Tell us about your cath lab. Crouse Hospital is a 563-bed not-for-profit hospital located in Syracuse, New York. Within the Cardiac Care Center, there are three cath labs and a nine-bed admission/recovery area. Crouse is an Accredited Chest Pain Center and Heart Failure Center by the Society of Chest Pain Centers and is the site of the region’s only pediatric cath lab. We have twelve registered nurses (RNs), one licensed practical nurse (LPN) and one interventional radiologic technologist. Several nurses working in the cath lab are currently working on either a bachelor’s or master’s degree in nursing. Together, our staff has an average of 15+ years experience in cardiovascular nursing. What procedures are performed in your cath lab? We perform diagnostic and interventional cardiac catheterizations, patent foramen ovale (PFO) closures, temporary and permanent pacemaker insertions, implantable cardioverter-defibrillator (ICD) insertions, pediatric catheterizations and ablations, emergency balloon septostomies on newborns, and diagnostic and interventional peripheral vascular studies. We also have the capability for intra-aortic balloon pumps, pericardiocentesis and thrombectomies. We perform approximately 35 scheduled procedures a week, and provide 24/7 emergency call for adult and pediatric emergencies. continued on page 24 September 2012 vol. 20, no. 9 Intro/Abstract The Resolute Integrity drug-eluting stent (DES) (Medtronic) was approved for use in the U.S. in February 2012. The first stent to have an indication for the treatment of coronary artery disease in diabetic patients, the stent has enjoyed rapid adoption in the clinical arena. The following case study illustrates the effective use of this stent in a diabetic patient. continued on page 14 THE TRANSRADIALISTS Iliac Artery Intervention via Radial Access Matthew Evans, DO, Kintur Sanghvi, MD, Deborah Heart & Lung Institute Browns Mills, New Jersey continued on page 10 CATH LAB MANAGEMENT Community-Based Collaborative Vascular Disease Detection How one center utilized the PADnet Disease Management System to grow its service line Cath Lab Digest talks with Jane Bower, CV Service Line Director of Development, West Georgia Medical Center, LaGrange, Georgia. continued on page 16 24 Cath Lab Spotlight september 2012 Continued from cover Crouse Hospital Lorissa Plis, DNP, RN, CNS, CCNS, CCPC, Manager Cardiac Care Center & Chest Pain Center Coordinator, Crouse Hospital, Syracuse, New York Does your cath lab perform primary angioplasty without surgical backup on site? Yes. We have an agreement with SUNY University Hospital, which is adjacent to Crouse Hospital. In the event of an emergency surgical intervention, patients are transported via a connecting tunnel directly to the University Hospital OR. What percentage of your patients is female? Forty-five percent of the patients we see are female. What percentage of your diagnostic caths is normal? On average, 74.16% of our patients need an intervention at the time of their catheterization. Only 25.82% are normal. Do any of your physicians regularly gain access via the radial artery? Yes, almost exclusively. We have been using the radial approach since 1997. We only utilize a femoral artery or a brachial cut-down approach when absolutely clinically necessary. The radial artery is even the site used with emergency ST-elevation myocardial infarction (STEMI) patients. Femoral arteries are reserved for right heart caths and for patients who absolutely cannot be accessed through the radial artery. Who manages your cath lab? Lorissa Plis DNP, RN, CNS, CCNS, CCPC, is the Cardiac Care Center manager and Chest Pain Center coordinator, Robert Pikarsky is the administrative director and Joseph Battaglia, MD, FACC, FSCAI, is the medical director. Do you have cross-training? Who scrubs, who circulates and who monitors? All RNs in the department rotate scrub, circulator and monitor roles. The LPN and the RT cannot push intravenous medications, so they only scrub and monitor cases. The RT is responsible for the radiology equipment and radiation safety. Does an RT (radiologic technologist) have to be present in the room for all fluoroscopic procedures in your cath lab? No, but we have a RT on staff in the cath lab. She is present and available for all cases, but is not assigned to each case. The physicians initiate and operate fluoro in all the cases. Which personnel can operate the xray equipment (position the II, pan the table, change angles, step on the fluoro pedal) in your cath lab? Only trained physicians and the interventional radiological technologist can operate the x-ray equipment. The physicians in our lab typically operate the fluoro pedal and pan the table during cases; however, the RT can assist with positioning the II, panning the table, and changing the angles or operating the fluoro pedal as needed. Nurses have no involvement in any of these duties. How does your cath lab handle radiation protection for the physicians and staff? Radiation safety is very important to us. Our RT and the inventory and equipment support specialist sit on the Radiation Safety Committee. We monitor and disclose radiation levels monthly to staff and are always looking for strategies to reduce radiation exposure. Quality Cardiac Care is a team approach; we are happy to partner with our EMS and Emergency Department to provide the best in patient care and promote community health. Pictured are Susie Barnett AEMT-P, Dr. Richard Steinmann (Emergency Department), Dr. Anil George (interventional cardiologist), and Crystal Barus MS, RN. Cath lab staff and physicians with director Robert Pikarsky. The pediatric lab. What are some of the new equipment, devices and products recently introduced at your lab? Because safety is our priority, we have instituted the use of the RadPad for our fluoro cases (Worldwide Innovations & Technologies, Inc.). The RadPad is a disposable, lead-free pad that reduces scatter radiation exposure to medical personnel during fluoroscopy procedures by 95%. We are also implementing the LUMEDX Cardiovascular Information System for real-time scheduling, and cardiac catheterization and echocardiography physician documentation. We have a dedicated cardiovascular information system (CVIS)/picture archiving and communications system (PACS) manager, Justin Pratt, AEMT-P. How does your lab communicate information to staff and physicians to stay organized and on top of change? We utilize email, bulletin boards, staff huddles and a communication book. We have Vocera for day-today communication and group pager systems. daily communication with Janice Jorgensen, our inventory and equipment support specialist. Janice was a LPN in the cath lab, but now oversees equipment and supplies, and coordinates with coding to assure our service codes and billing sheets are up to date and compliant. artery sheaths. We use closure devices on any patient who can be closed. When a manual press is required, all the cath lab staff is trained to perform it. During the orientation period, staff must perform five manual press sheath removals with their preceptors before performing independently. How is coding and coding education handled in your lab? The coder is located outside of the Cardiac Care Center, but she is in Who pulls the sheaths post procedure, both post intervention and diagnostic? Since we primarily do the radial approach, we do not have many femoral Where are patients prepped and recovered (post sheath removal)? Patients are prepped and recovered in our pre and post care observation 26 Cath Lab Spotlight september 2012 Dr. Joseph Battaglia and Dr. Anil George. Dr. Joseph Battaglia and the cath lab team. area, housed in the cath lab area. Sheaths are typically pulled while the patient is still on the cath lab table. Patients in whom activated clotting times (ACTs) are high, where sheaths cannot be pulled immediately, are moved to the recovery area, where sheaths are pulled by a staff member when appropriate. We utilize a closure device (Angio-Seal, St. Jude Medical) whenever possible to avoid manual pressing. What is your lab’s hematoma management policy? The cath lab staff manages all access sites throughout the hospital. How is inventory managed at your cath lab? Who handles the purchasing of equipment and supplies? Inventory is ordered and managed by the inventory and equipment specialist. We perform daily reconciliation of critical supplies, stents and balloons. Each room has designated par levels of supplies, and the rooms are assigned daily for restocking. The inventory and equipment specialist is in charge of all ordering and maintenance of supplies. New products are introduced through our Cardiac Value Analysis Team (VAT) for approval. Has your cath lab recently expanded in size and patient volume? We recently transitioned all ICD implants from the main OR to the Cardiac Care Center. We are in the process of expanding our hours of operation to accommodate early admissions and late discharges directly from the Center, rather than utilizing the Recovery Care Center. This expansion will allow for later scheduling of procedures and allow for increased volume. Do you have a hybrid cath lab, or are you planning to build one? Yes, one of our labs is a hybrid lab. We have the Mac-Lab as our hemodynamic system (GE Healthcare) and Siemens medical imaging equipment. Is your lab involved in clinical research? Yes, we are active in many clinical studies, in coordination with our cardiologists. We are also active in research with our emergency medical services (EMS) community. We also participate in the American College of Cardiology National Cardiovascular Data Registry (ACC-NCDR) and the NCDR-ICD Registry. Can you share your lab’s average door-to-balloon (D2B) times and how employees at your facility have worked together to keep D2B times under the mandated 90 minutes? We are incredibly proud of our D2B times. In 2010, our mean D2B was 45.25 minutes and in 2011, it was 39.25 minutes. We achieve over 81% of our cases in less than 60 minutes, and 100% were achieved within 90 minutes in 2011. We do participate in the AHA Mission Lifeline and the American College of Cardiology’s D2B Alliance A look at lab layout: The Cardiac Cath and EP rooms were designed and built in 2000 under standards that allowed for smaller rooms. We would definitely like larger labs. The EP lab is very small and difficult to do device work in. The cath labs become very congested with equipment. Ideally, our labs would be larger, with more cabinet space and our admission/ recovery area would be larger to accommodate reclining chairs at each bedside for recovery from the radial procedures. Who transports the STEMI patient to the cath lab during regular and during off hours? STEMI patients are transported by a combination of ED nurses, paramedics, physicians and cath lab staff. The minute the cath lab is ready, we roll, so whoever is at the bedside at the time transports. This is the case with both on and off hours. What do you do when the call team is already busy doing a procedure and a STEMI comes into the ED? We utilize a group page system. If the team is already in the middle of case, a second page goes out. Because only one physician is on call for the cath lab at a time, the case on the table is finished while the STEMI is prepped in another lab. What other modalities do you use to verify stenosis? We use intravascular ultrasound (IVUS, Volcano Corporation) and fractional flow reserve (FFR). What measures has your cath lab implemented in order to cut or contain costs? We have a Value Analysis Team (VAT) that is constantly looking for expense reduction and operational efficiency savings. We re-evaluate contracts, custom packs and supplies on a continuous basis, and are very aggressive in empowering staff and physicians to look for cost containment and expense reduction ideas. What quality control/quality assurance measures are practiced in your cath lab? Crouse Hospital is both an Accredited Chest Pain Center as well as an Accredited Heart Failure Center, so we are measuring many clinical indicators, including, but not limited to D2B times, transmission rate for EKGs from EMS, readmission rates, and turnaround times for troponins. We also measure multiple value-based purchasing indicators as well as patient satisfaction, employee satisfaction, physician satisfaction, and Hospital Consumer Assessment of Health Providers and Systems (HCAPS). Are you recording fluoroscopy times/ dosages? Yes, we document our fluoro times and doses in the Mac-Lab electronic clinical event logs and in our logbooks. We have protocols in place for high fluoro exposures for long-term 28 Cath Lab Spotlight september 2012 The cath lab staff is trained in adult cath, pediatric cath, and electrophysiology procedures, as well as device work. This training really sets them apart from other labs in the region. Lorissa Plis, DNP, RN, chest pain center coordinator and manager of cardiac care, and Dr. Joseph Battaglia, medical director. follow-up of patients. We evaluate fluoro procedures and doses on a bimonthly basis, and have a strong focus radiation reduction. This information is also reviewed at the monthly Radiation Safety Committee Meetings. Who documents medication administration during the case? The nurse monitoring the case documents all medications in the MacLab. The nurse and physician both sign this report before it is placed in the patient’s chart. How does your cath lab compete for patients? Has your institution formed an alliance with others in the area? Within the city of Syracuse, there are four hospitals with cath labs. We are physically connected to SUNY University Hospital, which also has one, although not affiliated. There is a lot of competition for market share. We utilize radio, TV, billboards, community forums and other media sources for advertisement. How do you handle vendor visits to your lab? We utilize VeriREP for vendor tracking. Vendors must make an appointment in the lab. No more than one vendor is allowed at one time unless there is a specific request from a physician. How are new employees oriented and trained at your facility? Orientation to the lab is staged. We begin with circulating, then the scrub role, then, finally, monitoring. We then transition their orientation to pacemaker/ICDs and lastly, the pediatric cath lab. We utilize a team approach, so each new nurse is assigned two preceptors for the duration of their orientation. What continuing education opportunities are provided to staff members? We have a weekly cardiac cath conference with presentations from the cardiologists and staff is strongly encouraged to attend. We also look for local and national conferences for staff when funding is available. We have a strong focus on staff returning to school for advanced degrees and allow for flexible scheduling to accommodate school. How is staff competency evaluated? We have yearly competencies that include computer-based learning, hands-on return demonstration, as well as skills labs that are set up in collaboration with our vendors for validating competency with equipment. Where is your cath lab located in relation to the emergency department (ED)? The cath lab is below the ED and there is a dedicated transport elevator for patients to be brought down to the cath lab. Does your lab have a clinical ladder? No. Currently there is a clinical ladder being developed for the organization. We do have an informal clinical ladder that allows staff to transition to charge nurse and orientor roles. What is unique or innovative about your cath lab and staff? We are almost exclusively a radial approach lab (for adults only). Patients have learned of this option and often come in requesting this approach. We are also the only pediatric cath lab in the region. The cath lab staff is trained in adult cath, pediatric cath, and electrophysiology procedures, as well as device work. This training really sets them apart from other labs in the region. How does your lab handle call time for staff members? We utilize self-scheduling for call. The only requirement is that there are two RNs on each team (which is always made up of three staff members). We do pay special attention to skill mix so that new nurses are not together when they come off orientation, until they gain more confidence and experience with emergencies. Within what time period are call team members expected to arrive to the lab after being paged? Staff has 20 minutes to arrive. Do you have flextime or multiple shifts? We do have some flexibility with shift scheduling. We currently have 0645, 0730 and 0830 start times. This will soon be expanded to include 0600-1830 shifts. Has your lab recently undergone a national accrediting agency inspection? We received Chest Pain Center Designation in 2010 and Heart Failure Center Designation in 2011. The best advice we have is start looking at your gaps, and build strong relationships and processes to support providing the best patient care. These designations really solidified the fact that our processes were resulting in the best patient care. What trends have you seen in your procedures and/or patient population? We are seeing a very disturbing trend of acute myocardial infarctions (AMIs) in our 30- to 50-year-old population. Is there a problem or challenge your lab has faced? Our greatest struggle is with consistency of scheduling. Given the nature of the cath lab, it is often hard to predict volumes. We work closely with our cardiology practices to try for consistency in scheduling elective caths, but inpatient and emergency cases are far less predictable. Worklife balance for the staff is very important, so we work hard at trying to help them achieve this. What’s special about your city or general regional area in comparison to the rest of the U.S.? How does it affect your “cath lab culture”? Syracuse University is adjacent to our hospital. Syracuse University football and basketball draw very big crowds to the “hill” where the university and Crouse Hospital are located. This creates large traffic jams and reduces accessibility to the hospital. As a result, we require on-call staff to stay in-house 2-3 hours before game time until the start of the game in order to ensure there are no delays in D2B times. The Society of Invasive Cardiovascular Professionals (SICP) has added two questions to our spotlight: 1. Do you require your clinical staff members to take the registry exam for Registered Cardiovascular Invasive Specialist (RCIS)? At this time, it is not required. We do encourage it and several staff members are in the process of obtaining their RCIS credential. They will receive an additional hourly stipend per union contract upon obtaining the RCIS. 2. Are your team members involved with any professional organizations that support the invasive cardiology service line? Members of the cath lab leadership have joined SCPC, AACN, SICP, and ACC. n Lorissa Pils, DNP, RN, can be contacted at LorissaPlis@crouse.org. A question from the American College of Cardiology’s National Cardiovascular Data Registry: How do you use the NCDR Outcome Reports to drive QI initiatives at your facility? We compare the reports with current QI initiatives and develop yearly QI initiatives driven by this data.