Biliary Tract Disease - Cleveland Clinic
7/24/2012
Biliary Tract Disease
John J. Vargo, MD, MPH
Talk Outline
Demographics
Types / pathogenesis
Complications of cholelithiasis
Complications of choledocholithiasis
Other gallbladder disorders
Sphincter of Oddi dysfunction
Other bile duct disorders
1
Gallstones
Affects 20 million Americans
Gender and Ethnic Predisposition
Over 65% are female
Hispanic and Native American
Lower socioeconomic status
600,000 annual cholecystectomies in U.S.
$6.5 billion annual cost
Gallstone Types
Black Pigment Stones (20%)
Cirrhosis (hemolysis d/t hypersplenism)
Chronic hemolysis
Older age
Female gender
No relationship to obesity
7/24/2012
2
Cholesterol Gallstone Pathogenesis
75% of cholelithiasis
Cholesterol super saturation
Nucleation
Calcium nidus
Defective acidification
Nucleation vs. Anti-nucleation factors
Growth
Gallbladder dysmotility (TPN, pregnancy)
Gallbladder mucus
Gallstone Types
Cholesterol
80% of GB stones
Female gender
Obesity
Rapid weight loss
Terminal ileal resection or disease
Pregnancy
Drugs: estrogen, OCPs, octroetide
Hypertriglyceridemia, DM, ?vagotomy
7/24/2012
3
Cholesterol Gallstone Formation
Micellar
Liquid
-----------------Moles % Bile Salts---------------
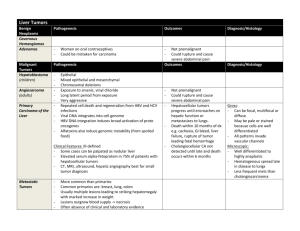
Pigmented Gallstones
10-25% of gallstones
Bilirubin deconjugation and precipitation
Bacterial β glucuronidase
Chronic hemolytic disorders
Decreased CaCO
3
Gallbladder stasis
7/24/2012
4
Brown Pigment Stones
Stasis and Infection s/p cholecystectomy > 2 yrs
7/24/2012
Gallbladder Sludge
Mixture of crystals and mucus
Can cause the same symptoms as stones
Can be transient
Diagnosed on ultrasound
5
Natural History of Gallstones
70-80%: remain asymptomatic
When symptoms occur, high likelihood that they will recur
Unknown why symptoms occur
Minority may have only one attack
Gracie and Ransohoff
5 yrs: 10% symptomatic
10 yrs: 15% symptomatic
15 yrs: 18% symptomatic
No sig complications
Complications of Cholelithiasis
Biliary colic
Cholecystitis
Fistulization (GB to duodenum)
Mirizzi syndrome
Cholangitis
Pancreatitis
GB cancer
7/24/2012
6
7/24/2012
7
7/24/2012
8
7/24/2012
9
Biliary Colic
RUQ, midepigastric
Lasts hours not weeks
Postprandial but may have nocturnal awakening
Crescendo, plateau, relief
Nausea and vomiting
Radiation to shoulder and back
Acute Cholecystitis
Duration: hours to days
Continued cystic duct obstruction
Cholescintigraphy: Sens/Spec > 90%
Ultrasonography: Sens/Spec > 90%
Alk phos, transaminases rarely twice normal
Mortality: 5-10% advanced age, comorbidities, complications
7/24/2012
10
Acute Cholecystitis
Complications
Emphysemaotus cholecystitis
Perforation
Mirizzi Syndrome
Cystic duct stone leading to biliary obstruction
Cholecystoenteric fistula
Pneumobilia
Duodenum, Colon, Jejunum, Stomach
Gallstone ileus
Cholescintigraphy False
Positives
Prolonged fasting
Liver disease
Chronic cholecystitis
Total parenteral nutrition
Critical illness
7/24/2012
11
Acalculous Cholecystitis
Older and more likely male
Triad
Hemodynamic instability
Prolonged fasting
Immobility
Fever, RUQ pain, leukocytosis, tenderness may be absent
More fulminant course
Acalculous Cholecystitis
CT scan
GB wall > 4 mm
Sonographic Murphy’s sign
Subserosal edema
Intramural gas
Pericholecystic fluid collection
Sloughed mucosa
Sens / Spec >95%
Sensitivity: 67-92%
Specificity: > 90%
Scintigraphy
False (+)#
* In the absence of hypoalbuminemia / ascites
# narcotics, anticholinergics, diabetes mellitus, celiac sprue, obesity
7/24/2012
12
7/24/2012
Cholecystectomy
Open or laparoscopic: 0.1% mortality
Laparoscopic: reduction in postoperative
LOS and pain
Complicated presentation, coagulopathy or adhesions->open
IOC: allows for ID and potential treatment of choledocholithiasis
False (+) rate of 1-5.6%
Ford JA et al. Br J Surg 2012;99:160-7.
13
Other Treatment Modalities
Ursodeoxycholic acid
Small floating stones on oral cholecystogram
Non-calcified on ultrasound
Much less effective
High recurrence rate (50%)
Risk of pancreatitis and cholangitis
ESWL not approved in U.S.
Cholecystostomy tube
Choledocholithiasis
Can present with biliary colic
Elevated liver profile
With chronicity, dilated common bile duct
Jaundice
Cholangitis
Pancreatitis
7/24/2012
14
Choledocholithiasis
RUQ Pain
Fever
Charcot’s
Triad
Jaundice
Choledocholithiasis:
Acute Suppurative Cholangitis
RUQ Pain
Hypotension
Raynaud’s
Pentad
Altered
Level of
Consciousness
Fever
Jaundice
7/24/2012
15
Choledocholithiasis
Recurrent biliary colic in the postcholecystectomy patient
ERCP for patients with high probability
95 success rate
5% complication rate
For low or intermediate probability
MRCP
EUS
Intraoperative cholangiogram
Choledocholithiasis
Biliary sphincterotomy
Balloon /basket extraction
Balloon sphincteroplasty
Cholangioscopy
Lithotripsy
Mechanical (basket)
Laser
Electrohydrualic
Extracorporeal shockwave lithotripsy
7/24/2012
16
Recurrent Pyogenic Cholangitis
Prototypic syndrome seen in Asia and
Asian immigrants
Parasitic infestation &/or malnutrition
Polymicrobial cholangitis
Brown and black stones
CBD,CHD; L > R hepatic duct
Complications: Cholangitis, PV thromobosis, Abscess, Cholangiocarinoma
Treatment :Endoscopic, IR, Surgical
Gallbladder Dyskinesia
Decreased GB ejection (via CCK-HIDA) fraction may predispose to gallstone formation
GB ejection fraction > 38%
Controversial whether cholecystectomy leads to symptomatic improvement
More common in subjects with functional bowel disorders
DiBaise et al., Clin Nuc Med 2012;37:63-70.
7/24/2012
17
Gallbladder Polyps
Cholesterolosis
Cholesterol / TG within epithelial macrophages
Local or diffuse
Can be combined with cholesterol polyps
10-15% autopsy series
Rarely detectable via imaging
Rarely thought to be asymptomatic
Gallbladder Polyps
Adenomyomatosis
Hypertrophy of the muscle layer
Usually focal (fundus) although can be diffuse
Incidental and asymptomatic
Surgery when wall > 10 mm, associated mass or in rare instances with diffuse disease
7/24/2012
18
Gallbladder Polyps
1-5% of population
> 95% non-neoplastic (cholesterol)
Follow with ultrasound for 6 month-1 yr intervals
If growth > 10 mm, cholecystectomy
If no growth after 2 yrs, can dispense surveillance
GB polyp (any size) + PSC = surgery
GB Cancer
Rarely diagnosed early
Surgery only curative option
5 yr survival: <10%
Associations:
Female gender
Porcelain gallbladder
IBD
PSC
Anomalous pancreaticobiliary junction
Cholelithiasis
Chronic Salmonella typhi
Adenomatous GB polyps
7/24/2012
19
Sphincter of Oddi Dysfunction
Stenosis or spasm of the Sphincter of Oddi
Persistent / recurrent biliary pain following cholecystectomy without structural abnormalities
Idiopathic recurrent pancreatitis
Biliary type pain with intact gallbladder and no stones
No role for Sphincter of Oddi manometry with gallbladder in place
Corraziara ES, Cotton PB. Am J Gastroenterol 2010;105: 764-9.
Biliary Sphincter of Oddi
Dysfunction
Type I: biliary type pain, elevated liver enzymes (> 2x nl on two occasions), bile duct diameter > 8 mm; delayed contrast drainage > 45 minute
Type II: biliary type pain and 1 or 2 of the aforementioned criteria
Type III: biliary type pain only
7/24/2012
20
Type I
Type II
Type III
Biliary Sphincter of Oddi
Dysfunction
SOD Type Prevalence of
Manometric
Abnormalities (%)
65-95*
50-63
12-59
Biliary Sphincter of Oddi
Dysfunction
Type I: empiric biliary sphincterotomy
85-100% response
Type II: sphincter of Oddi manometry
(SOM)
Pain relief up to 40-60% in this subset with biliary sphincterotomy with SOD
Normal SOM and sphincterotomy: controversial
7/24/2012
21
Biliary Sphincter of Oddi
Dysfunction
Type III:
10-58% response to sphincterotomy if SOD
Current subject of an NIH trial
Consider other treatments for functional bowel disorders
7/24/2012
Sphincter of Oddi Manometry
Basal pressure > 40 mm Hg
Correlates best with presence of symptoms and relief following sphincterotomy
22
Abnormal Biliary and Pancreatic
Sphincters in Pts with Suspected
SOD
Patient
#
360
Biliary
Alone (%)
41 (11.4)
Pancreatic
Alone (%)
68 (18.9)
Both
(%)
113
(31.4)
Total (%)
219 (60.1)
Eversman D, et al. Gastrointest Endosc 1999;50:637-41.
Pancreatic SOD
Consider in idiopathic acute recurrent pancreatitis
Type I: Acute pancreatitic pain, dilated
MPD (6 mm head, 5 mm body) Amylase or lipase > 1.5 x normal at least one occasion
Type II: Pain + one other criterion
Type III: Pain only
7/24/2012
23
Choledochal Cysts
Congenital anomalies of the biliary tree
Incidence: 1/15,000
15x’s more common in Japan
Females more commonly affected
2/3 cases manifest by age 10
Choledochal Cysts
Type I: (most common) 80-90% of cases.
Fusiform dilation of CBD (segmental or diffuse)
Type II: Choledochal diverticulum
Type III: Cholodochocoele (intraduodenal dilation
Type IV: Multiple intra- extrahepatic cysts
Type V: Multiple intra- extrahepatic dilation (Caroli’s disease)
7/24/2012
24
Choledochal Cysts
Association with anomalous union of pancreatic and biliary ducts
Jaundice, abdominal pain, intraductal stones
At risk for cholangiocarcinoma
Surgical excision
Caroli's disease associated with congenital hepatic fibrosis, renal tubular ectasia and polycystic kidney disease
IgG4 Cholangiopathy
PSC or hilar cholangiocarcinoma “look alike”
>90% associated with autoimmune pancreatitis
Elevated IgG4 levels
Tissue diagnosis required (ampullary bx, liver bx, bile duct biopsy)
Dramatic response to steroids
Zen Y, Nakanuma Y. Int J Hepatol ;doi:10.1155/2012/472376.
7/24/2012
25
Summary
Demographics
Types / pathogenesis
Complications of cholelithiasis
Complications of choledocholithiasis
Other gallbladder disorders
Sphincter of Oddi dysfunction
Other bile duct disorders
7/24/2012
26