Comparison of Roentgenography and Moire Topography for
advertisement

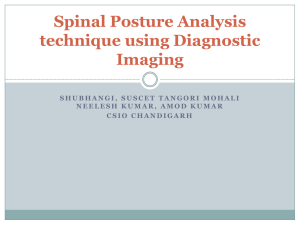
Comparison of Roentgenography and Moire Topography for Quantifying Spinal Curvature MOHSEN M. EL-SAYYAD The purpose of this study was to compare roentgenography and moire topography for identification, treatment, and prevention of scoliosis at an early age. Moire topography was used as an assessment tool for the quantitative examination of 12 children with mild-to-moderate scoliosis receiving physical therapy during a three-month period. Each child's roentgenogram also was analyzed independently by orthopedic physicians and radiologists using the Cobb method of measuring spinal curvature. Rho correlations of Cobb angles and the spinal curvature angles based on moire photographs taken at weeks 4, 8, and 12 were found to be +.94, +.96, and +.93, respectively. The moire method, thus, may be used as an available, inexpensive, and easily interpreted diagnostic and treatment tool in physical therapy. Key Words: Physical therapy, Radiography, Scoliosis, Spine. Both the initial examination of patients with scoliosis and their followup assessment during treatment present a considerable challenge to health care professionals. The lack of accurate and scientifically acceptable assessment tools previously made the quantification of the degree of deformity and of improvement of scoliosis difficult to document. In 1982, the faculties of the School of Physical Therapy and the Department of Orthopedics in the School of Medicine of Cairo University jointly participated in the examination of children enrolled in a preschool and in an elementary school to detect, treat, and prevent scoliosis at an early age. In this study, moire topography was chosen as one of the tools for examination of the school children and for the follow-up assessment of those children who subsequently were assigned to physical therapy for the treatment of scoliosis. Other methods of assessment used were independent clinical examinations conducted by orthopedic physicians and roentgenographic examinations conducted by radiologists. In this article, Dr. El-Sayyad was Associate Professor of Physical Therapy, School of Medicine, Cairo University, Cairo, Egypt, when this study was conducted. He is currently Associate Professor of Physical Therapy, King Abdulaziz University, Medinah Munawwara, PO Box 344, Saudi Arabia. This paper was presented at the Ninth Congress of the International Society of Biomechanics, Waterloo, Ontario, Canada, August 7-12, 1983. This article was submitted March 4, 1985; was with the author for revision 19 weeks; and was accepted November 20, 1985. 1078 moire topography is described as a method of obtaining quantified data used to analyze changes in spinal curvature. The results of a correlational study comparing moire and roentgenogram data are presented. Moire topography is a simple biostereometric method of analysis of spatial characteristics by means of three-dimensional mapping of the body. It involves the illumination of the subject with a spotlight through a special screen to highlight contour surfaces of the body that will appear as "fringes" or separate bands that can be observed or photographed. The technique is not new, having been described as long ago as the late 19th century.1,2 Its applicability to body surface shape was introduced first by Takasaki in 1970.3 In a moire study of scoliosis conducted by Adair et al, the authors compared the results of three independent diagnostic methods: roentgenogram analysis, moire topography, and orthopedic clinical examination.4 They reported that 94% of the diagnoses of scoliosis made using roentgenography also were detected using moire topography, but that only 46% of those diagnoses also were made through clinical examination. The authors, therefore, concluded that the moire method essentially is as effective as roentgenography in the diagnosis of scoliosis and that it is superior to clinical examination. The moire method may be used both to obtain a graphical representation of the back for the qualitative evaluation of scoliosis and to obtain mathematical measurements for a quantitative assess- ment of scoliosis as described by ElSayyad and Kamal in 1981.5 A review of the literature reveals that the reliability of quantitative measurements of the Cobb angle5"7 using the roentgenograms of patients with scoliosis have not been reported. Cobb's method of measuring spinal curvature, also called the "end-of-curve method,"8 is used widely today. Cobb suggested measuring the angle of spinal curvature by drawing lines parallel to the upper border of the upper vertebral body and to the lower border of the lowest vertebral body of the primary curve. The angle between perpendiculars erected from these lines is the angle of curvature. A literature search also revealed that the reliability of the moire topographic technique used in this study was not known previously.9 Tredwell and Bannon, however, cite an unpublished report of a study conducted by Tredwell at Shaughnessy Hospital in Vancouver, Canada, August 1983, in which an interrater variance of ±3 degrees for measurements of the Cobb angle in scoliosis was reported.9 METHOD Subjects Four hundred children were examined by the orthopedic physicians. Of that total, seven boys and five girls ranging in age from 4 to 7 years ( age 5.5 years, s = .98) were diagnosed and classified according to the angle of spinal curvature as either mildly scoliotic (515°) or moderately scoliotic (15-40°). PHYSICAL THERAPY RESEARCH Roentgenograms and moiré photographs were taken for each child at the beginning and at monthly intervals of the three-month physical therapy program. Roentgenographic data of the subjects were not made available either to me as I conducted the moire examinations or to the physical therapists who treated the children. Informed consent was obtained from a parent of each subject before the study. Equipment For standardized positioning of each subject, two laser beams were aimed at an angle of 45 degrees to the midline of the body and focused on the center of the mirror installed on a belt worn at the subject's waist (Fig. 1). For the photograph of the back, the mirror's center was marked with a dot and aligned as precisely as possible with the umbilicus of the subject, who stood facing the lasers with his back to the screen. For this study, a special 100-cm × 50cm moiré screen was constructed at Cairo University. The screen was composed of a simple frame and of a grid of horizontally placed nylon wires that were separated by a distance equal to their thickness (Fig. 2). The subjects stood behind the screen and were photographed with a sonar-focusing, instant-processing camera and with a 35mm single-lens reflex camera located 170 cm from the screen. A 1,000 W tungsten light source was positioned 50 cm above the cameras. Fig. 1. Positioning of the subject. Procedures The positioning of the subjects is the most important element in taking a good photograph for moiré analysis. A moiré topogram taken with the subject misaligned would appear blurred or unclear and cannot be used for quantitative analysis.10-13 In this study, the subjects were instructed to stand looking straight ahead, arms down in a relaxed position and back parallel to the screen, and as close as possible to the grid without actually touching it. If required, the subject's position was adjusted until the fringe patterns demonstrated by the buttocks were symmetrical. No attempt was made to position the upper trunk, except that the subjects were instructed to relax. A standard projection system involves a grid screen, a light source, and a camVolume 66 / Number 7, July 1986 Fig. 2. Arrangement of equipment. era arranged in a geometric relationship according to Takasaki's equation3: (1) where h is the height of the n-th fringe from the grating plane, L is the distance from the camera to the screen, w is the distance from the light source to the camera, d is the pitch of the fringe screen, and n is the fringe plane number. The screen-length measurement (70 cm) was photographed and used to calculate the ratio of real screen length to projected screen length. Two reflective dots, one located at the seventh cervical vertebra (C7) and the other at the first sacral vertebra (Sl), were used as reference points. All photographs were scaled 1079 malities of the structural and functional relationships between the right and left sides of the body. The spine is symmetrical if all corresponding points (eg, points H and E in Fig. 4) that are located equidistant from a central axis (PQ) are mirror images. A scoliotic spine, however, will show a lack of symmetry that is associated with lateral deviation. Disturbances in the surface contours are produced readily by scoliosis in the thoracic region because the rib cage magnifies the rotational component of the scoliosis. In the left lower thoracic curve shown in Figure 4, the asymmetry involves primarily both the scapular pattern and the W pattern. In this particular pattern disturbance, a greater number of scapular contours are shown in the involved right side compared with the uninvolved left side, and one limb of the W pattern descends along the upper thoracolumbar region of the involved side indicating elevation in this area. Fig. 3. Moiré pattern of a normal spine. to a factor of 1:3 at the level of the grid screen for topographic analysis. The moiré topography procedure described in this article varies from that used by other investigators. It provides anatomical points of reference (C7 and Sl) for the examination of spinal curvature, rather than of the shape of the back, either by using an arbitrary vertical line on the moiré screen or drawing a line on the moiré photograph dividing the body into right and left segments.3,14 The subjects' alignment also was improved by instructing them to relax with their arms hanging naturally. As the lower base points of the W pattern descend along the paravertebral thoracolumbar region into the upper lumbar region, they are replaced by vertically oriented contour levels descending on either side of the waist (Fife. 4). The nearest visible moiré fringes to the central axis (PQ) corresponding to points E and H represent the level of maximum asymmetry. The point 0 is the midpoint of the line segment HE, and point C is the origin. The distance between points E and H was determined using the following formula: Normal Back Topography The surface of the normal back (Fig. 3) reflects the expected elevations in the scapular and middle thoracic regions, the depression through the middle lumbar region, and subsequent elevation in the sacral region. Because the contour lines formed by the moiré fringe represent lines of uniform height, they tend to be continuous O patterns around the elevated areas of each scapula and the gluteal region. In the upper thoracic region, as the contour lines rise cephalad from these elevated scapular regions toward the base of the neck, the contour lines become discontinuous laterally in the shoulder region to form the contours of the shoulder. Similarly, the contour lines descending caudally from the scapular region usually form a W pattern in the thoracic region. The lower base points of the W pattern descend along the paravertebral thoracolumbar ridges into the upper lumbar regions where they are replaced by vertically oriented contour levels descending on either side 1080 Fig. 4. Measurement of the angle of spinal curvature by moiré topographs. of the waist, which are designated lateral V left andright.The pattern of the upper back begins to repeat itself, proceeding caudally in the lumbar region.13 In the normal back, the number of fringes are equal on both sides of the back to within one fringe interval of difference (Fig. 3). The actual number of fringe lines occurring symmetrically on both sides is, in part, determined by the size of the subject and the amount of deformity. Because the generator of the curved surface is a straight line, the curves of the oblique section of the spine are symmetric if the spine is symmetric and parallel to the screen. This distinctive feature of an instrument composed of a horizontal grid is used to detect asymmetries that may indicate abnor- d1 = ½ (CH + CE) (2) where line segment CE (positive) is the distance on theright,and line segment CH (negative) is the distance on the left. In the upper thoracic region, as the contour lines rise cephalad from these elevated scapular regions toward the base of the neck, the contour lines become discontinuous laterally in the shoulder region to form the minimum asymmetry level. The nearest visible moiré fringes to the central axis (PQ) corresponding to points G and D represent the level of minimum asymmetry. At point A above point C, the distance d2 was determined using the following formula: d2 = ½ (AD + AG) (3) At point B below point C, where the moiré fringes also show minimum PHYSICAL THERAPY RESEARCH asymmetry, the distance d3 was determined using the following formula: d3 = ½ (BF + BI) (4) The angle of spinal curvature at point O, thus, was calculated using the equation: Q = tan-1 (d, - d2/AC) TABLE Correlation of the Angles of Scoliosis Curvature Based on Roentgenogram and Moiré Methods (N = 12) First Measurements (after 4 wk) Subjects -1 + tan (d1 - d3/BC) (5) The data were processed at Indiana University using a Fortran digital computer program and the formula for determining the angle of spinal curvature. To obtain the angle of spinal curvature from the roentgenograms, the radiologists used the Cobb method. Data Analysis Spearman's rho correlation coefficients, appropriate for small sample sizes, were determined using the data obtained after the 4th, 8th, and 12th weeks of the treatment program. RESULTS The Table shows the angles of spinal curvature for each examination period, as calculated from the roentgenograms using the Cobb method and from the moiré photographs using the formula described earlier. The statistical correlation of the two sets of measurement for each examination period were calculated using Spearman's method of rho correlation. The rho correlation coefficients were found to be +.94, +.96, and +.93 for weeks 4,8, and 12, respectively. DISCUSSION The calculation of the moiré angle provides a method for the objective measurement of symmetry because the calculation is based on a single midline axis between C7 and the gluteal fold. Unlike profile-type analysis, it is not dependent on locating other landmarks on a subject's back to be repeatable over a period of time, such as during the course of treatment for the subject's scoliosis. Moiré topography involves the examination of the outside of the body, rather than of the skeleton. The objective of moiré topography, therefore, is to align the subject's skeleton according to fixed reference points that will facilitate the analysis of contour changes. I believe that it is important to align the subject's skeleton so that repeated moiré Volume 66 / Number 7, July 1986 1 2 3 4 5 6 7 8 9 10 11 12 Rho correlation coefficient Second Measurements (after 8 wk) Third Measurements (after 12 wk) Cobb Angle (°) Moire Angle (°) Cobb Angle (°) Moiré Angle (°) Cobb Angle (°) Moiré Angle (°) 11.50 20.00 15.50 31.50 8.00 11.00 36.00 25.00 22.50 34.00 16.50 28.50 11.26 22.50 16.08 31.44 9.38 11.96 36.74 23.00 22.25 31.80 16.75 28.24 9.00 16.50 15.00 28.00 4.50 11.00 34.50 23.50 22.00 31.00 9.50 21.00 10.75 16.58 16.52 29.90 6.00 11.25 33.88 23.70 23.10 30.74 10.15 19.62 8.50 17.00 14.50 25.00 5.00 9.00 27.50 20.00 17.50 31.50 7.50 20.00 8.94 16.75 14.22 24.88 8.30 10.74 29.70 19.96 16.95 32.15 8.24 22.60 +.94 photographs will show that contour changes are caused by skeletal changes. Other methods of moiré topography used in the diagnosis and treatment of scoliosis also have been reported.15-19 Drerup et al demonstrated the changes resulting from treatment of spinal curvature using a longitudinal cross-sectional contour graph.2 This method is simple and graphically demonstrates the changes in the back produced by an operation. Roger analyzed the digital data of moiré topograms and developed a transverse cross-sectional contour graph based on five different reference points on the back.10 He then calculated rotation, from the reference plane, of the time tangent of both humps of the contour line. This method is useful to reveal rotational deformities of the scoliotic back. The method of moiré topography that I used in my study is more comprehensive than the methods used in these previous studies because the method that I used enables the clinician to determine the location and the angle of spinal curvature. The correlation coefficients in the Table indicate that the moiré method of quantifying mild and moderate scoliosis and of analyzing changes in the subject's spinal curvature is a simple and convenient physical therapy technique. Such results should be interpreted with caution, however, because of the following potential sources of error: 1. Changes in the patient's positioning during roentgenography or moiré +.96 +.93 photography may alter the shape of the spinal curvature, thereby affecting measurements based on the Cobb angle or the moiré topography formula. 2. The growth of the child generally results in changes in the measurements obtained by either method of examination and may be misinterpreted as changes attributed to treatment. 3. Studies of the interrater reliability of the Cobb method of measuring topographic values have not been reported in the literature and are needed. 4. Studies of the intrarater reliability of measurements based on the Cobb angle or on moiré topography and obtained from the same subjects during the same examination period have not been reported. CONCLUSIONS In this study of mild and moderate scoliosis using both roentgenography and moiré fringe topography, I found that distinct patterns could be identified that correlated with the anatomical regions of the scoliosis. The measurements of the moire angles and of the Cobb angles were closely correlated. Moiré analysis can reduce the risk of radiation to children who presently must undergo repeated roentgenographical examinations. Moiré topography is economical (about 40 cents an examination), noninvasive, and relatively fast and easy to use and interpret. It is an assessment tool that is available to physical therapy clinics without requiring 1081 much space or training. The topographs may be maintained as permanent records of patients in physical therapy and allow the therapist to review and compare curve changes in a quantified manner. The topographs also provide a basis for the clear identification of the region of spinal involvement if anatomical regions are used as points of reference, as described in this study. Further research of the reliability of the methods of measurement used in this preliminary study based on a larger sample is needed. The experimental design of future studies should include a control group of healthy subjects to counterbalance the effects of growth change and other possible sources of invalidity. The development of a positioning protocol is essential to further studies of moiré topography, as well as to its clinical use in physical therapy. Acknowledgment. I thank Dr. Tali Conine, Professor and Director, School of Rehabilitation Medicine, University of British Columbia, for her continuing advice and support. 1082 REFERENCES 1. Deutschlander CA: Perimetrische Buckelmessung. Centralblatt fur Chirurgie 43:1049-1051, 1901 (German) 2. Drerup B: Anwendungen der Moiré-Topography zur Diagnose und Dokumentation von Fehlbldungen des Rumfes. Z Orthop 116:789, 1978 (German) 3. Takasaki H: Moiré topography. Appl Optics 9:1467-1472,1970 4. Adair IV, van Wijk MC, Armstrong GWD: Moiré topography in scoliosis screening. Clin Orthop 129:165-171,1977 5. El-Sayyad MM, Kamal A: Cobb's angle measurement by moiré topographs. In: Proceedings of the Thirty-Fourth Annual Conference on Engineering in Medicine and Biology. Houston, TX, September 23,1981, p 311 6. Cobb JR: Outline for study of scoliosis. In: American Academy of Orthopaedic Surgeons: Instructional Course Lectures. St. Louis, MO, C V Mosby Co, 1948, vol 5, pp 261-275 7. Csongradi JJ, Bleck EE: Moiré topography: Use in scoliosis observation. In Drerup B, et al (eds): Moiré Fringe Topography and Spinal Deformity. Stuttgart, West Germany, Gustav Fischer Verlag, 1983, pp 141-147 8. Neugebauer H: The different methods of measuring the curve of a scoliotic spine. In Drerup, B, et al (eds): Moiré Fringe Topography and Spinal Deformity. Stuttgart, West Germany, Gustav Fischer Verlag, 1983, pp 17-26 9. Tredwell S, Bannon M: Use of shadow moiré topography in predicting clinical changes in scoliosis. In: Proceedings of the Scoliosis Research Society. San Diego, CA, September 17-20,1985 10. Roger RE: Monitoring adolescent idiopathic scoliosis with moiré fringe photography. Eng Med 8:119, 1979 11. Willner S: Moiré topography for the diagnosis and documentation of scoliosis. Acta Orthop Scand 50:295-302,1979 12. Windischbauer G, Schedle J: Moiré topographical evaluation of back shape deformities by basic programmable computer. In Drerup B, et al (eds): Moiré Fringe Topography and Spinal Deformity. Stuttgart, West Germany, Gustav Fischer Verlag, 1983, pp 227-335 13. Moreland MS, Barce CA, Pope MH: Moiré topography in scoliosis: Pattern recognition and analysis. In Moreland MS, et al (eds): Moiré Fringe Topography and Spinal Deformity: Proceedings of an International Symposium. Elmsford, NY, Pergamon Press Inc, 1981, pp 171185 14. Bannon M, Tredwell S: Clinical decision making: The role of relative moiré measurements. In: Proceedings of the Third International Symposium on Surface Topography and Spinal Deformity. Oxford, England, September 27-28, 1984 15. Beekman CE, Hall V: Variability of scoliosis measurement from spinal roentgenograms. Phys Ther 59:764-765,1979 16. Lonstein JE, Bjorklund S, Wanninger MH, et al: Voluntary school screening for scoliosis in Minnesota. J Bone Joint Surg [Am] 64:481488,1982 17. Stone B, Beekman CE, Hall V, et al: The effect of an exercise program on change in curve in adolescents with minimal idiopathic scoliosis: A preliminary study. Phys Ther 59:759-763, 1979 18. White AA, Panjaki MM: The clinical biomechanics of scoliosis. Clin Orthop 118:100-112, 1976 19. Torell G, Nordwell A, Nachemson A: The changing pattern of scoliosis treatment due to effective screening. J Bone Joint Surg [Am] 63:337-341,1981 PHYSICAL THERAPY