Payment systems and their role in integration

Key points on payment systems and their role in integration
There are many influential factors to deliver integrated care. The payment system is one of several levers
(or barriers) that could support it.
1. Types of payment systems
There are various different payment systems. Different systems are more or less appropriate for commissioning different types of care.
How money currently flows from commissioners to providers:
Payment by Results - reimburses providers of care by the volume and type of care (case-mix) provided based on a schedule of national prices for specific interventions
Local tariffs - paid by volume with the unit of activity and price determined locally by providers and commissioners
Block contracts - pay providers to provide a given level of capacity (e.g., staffing or number of beds)
Using payment systems to incentivise integrated care
The following could be used to incentivise integrated care by how they incentivise investment in preventative medicine and how they incentivise payment in different parts of the care pathway:
Pathway payment systems – A price is set for bundle of activities with defined start and end points (eg. from referral to reablement)
Capitation/partial capitation - Fixed price paid per patient for defined period of time (eg. frail elderly)
Outcomes-based contracting - aims to shift the emphasis from what services a provider will offer to what outcomes they will achieve (eg. maintained independence)
2. Advantages and Disadvantages
The following table gives some advantages and disadvantages for patients, providers and commissioners associated with the various payment systems. The list is by no means exhaustive, and it is important to remember that the effectiveness of the payment system depends on the context of care and constitutes one of many levers to better, more efficient and integrated care.
Advantages
Block Contracts
Disadvantages
Low transaction costs
Predictable expenditure and income
Flexibility for innovation as it has no impact on income
Lacks transparency and accountability.
Disincentive to increase activity
Providers could avoid or under-serve complex and costly patients
Disincentive to increase innovation if more costly
Lack of choice, competition and performance incentives
Pathway/Activity Based Payment Systems
Advantages
Supports patient and commissioner choice
Disadvantages
Financial control for commissioners is more difficult
Better benchmarking of costs
Incentivises increased activity
Transaction costs are higher due to the need for billing and more sophisticated costing systems.
Can incentivise increased activity in the acute sector
Can lead to treating one patient condition amongst multiple long term conditions
Payment by Results/Outcomes-based contracting
Advantages
Incentivises efficiency
Incentivises quality
Advantages
Low transaction costs
Financial control
Money follows the patient, so potentially improved quality and incentives for prevention
Disadvantages
Providers may avoid treating sicker patients or those with complex conditions
Increased financial risk associated with innovation
Difficulties with measuring outcomes due to time-lag at what to attribute to a single activity
There is currently limited evidence to support financial incentivisation of outcomes.
Capitation
Disadvantages
There is no incentive to provide additional or more costly services for patients enrolled.
Incentives are dependent on patient choice
Incentives for prevention rely on long term contracts
Incentives rely on capitation payments covering al l aspects of a patient’s care
3. Existing examples of payment systems for integration: a) Capitation – Alzira, Spain
Definition - Capitated payment systems provide a set payment for each person within a group’s care, regardless of how much care each person receives. They cover primary and secondary care and encourage investment in preventative medicine. This capitation can either be ‘global’ across a whole network or specific to individual providers. It is controversial because it puts more economic considerations into the provision of patient care by providers, which could lead to cutting corners, disincentives to prevention and competitiveness.
Example from Alzira, Spain - Under this model, the private contractor receives a fixed annual sum per local inhabitant (capitation) from the regional government for the duration of the contract and in return must offer free, universal access to its range of health services. b) Prime/Provider Contractor - Staffordshire
Definition - The prime contractor model involves a single organisation subcontracting work to other providers to integrate services across a pathway. The prime takes all of the risk and reward and then shares this out proportionally to the subs thereby effectively spread betting the contract.
Example from Staffordshire – for cancer and end of life care, a single (or prime) provider will be held accountable for the entire patient experience and clinical outcomes. This enables a transformation in service design and delivery focused on the patient and outcomes along an integrated pathway, not on individual providers.
4. Leeds as an Integration Pioneer:
Leeds has asked Monitor and NHS England to provide through the Pioneer programme support to test and refine financial incentives to ensure that they fully align with achieving the best outcomes for people.
External support has been promised to enable the pioneers to be the first to test new models of commissioning and new payment arrangements. The current general approach from Monitor is to try to provide support and tool, not national rules. In Leeds, we are currently looking at how best to approach this and what support from Monitor and PwC, amongst others, would potentially look like.
Appendix:
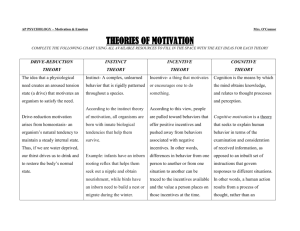
Diagram from Monitor on how different currencies incentives different behaviours:
Monitor - Integration and Payments
Contact: Rob.Newton@leeds.gov.uk
07990088417