Maple Syrup Urine Disease Care Plan
advertisement
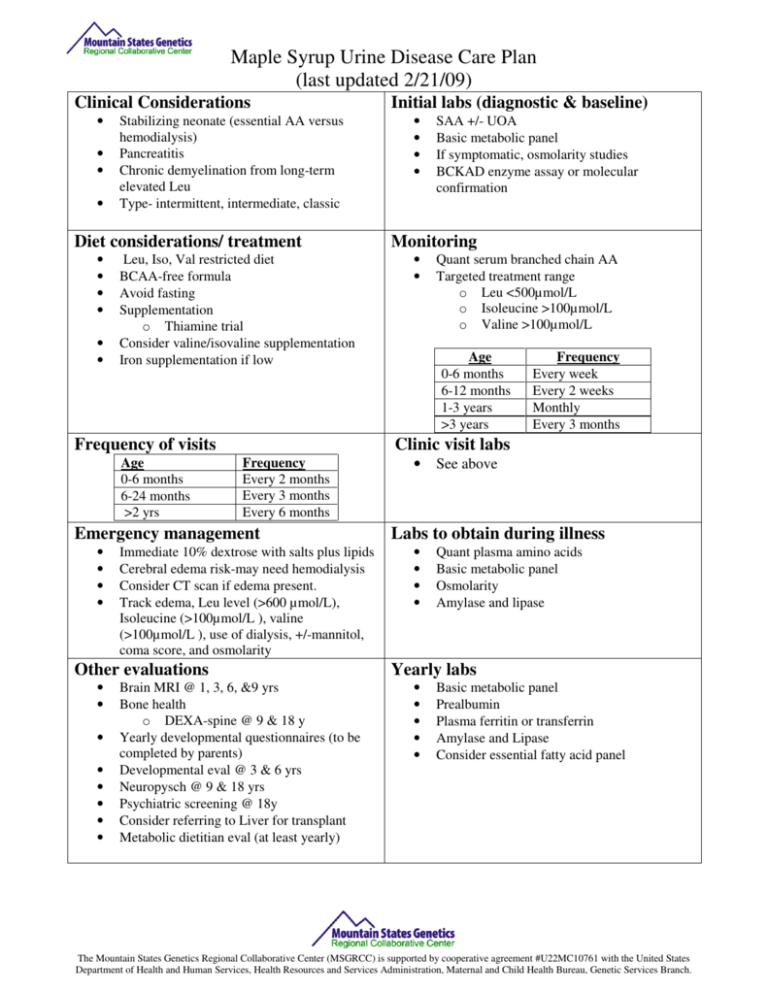
Maple Syrup Urine Disease Care Plan (last updated 2/21/09) Clinical Considerations • • • • Stabilizing neonate (essential AA versus hemodialysis) Pancreatitis Chronic demyelination from long-term elevated Leu Type- intermittent, intermediate, classic Diet considerations/ treatment • • • • • • Leu, Iso, Val restricted diet BCAA-free formula Avoid fasting Supplementation o Thiamine trial Consider valine/isovaline supplementation Iron supplementation if low Frequency of visits Age 0-6 months 6-24 months >2 yrs Frequency Every 2 months Every 3 months Every 6 months Immediate 10% dextrose with salts plus lipids Cerebral edema risk-may need hemodialysis Consider CT scan if edema present. Track edema, Leu level (>600 µmol/L), Isoleucine (>100µmol/L ), valine (>100µmol/L ), use of dialysis, +/-mannitol, coma score, and osmolarity Other evaluations • • • • • • • • • • • • SAA +/- UOA Basic metabolic panel If symptomatic, osmolarity studies BCKAD enzyme assay or molecular confirmation Monitoring • • Quant serum branched chain AA Targeted treatment range o Leu <500µmol/L o Isoleucine >100µmol/L o Valine >100µmol/L Age 0-6 months 6-12 months 1-3 years >3 years Frequency Every week Every 2 weeks Monthly Every 3 months Clinic visit labs Emergency management • • • • Initial labs (diagnostic & baseline) Brain MRI @ 1, 3, 6, &9 yrs Bone health o DEXA-spine @ 9 & 18 y Yearly developmental questionnaires (to be completed by parents) Developmental eval @ 3 & 6 yrs Neuropysch @ 9 & 18 yrs Psychiatric screening @ 18y Consider referring to Liver for transplant Metabolic dietitian eval (at least yearly) • See above Labs to obtain during illness • • • • Quant plasma amino acids Basic metabolic panel Osmolarity Amylase and lipase Yearly labs • • • • • Basic metabolic panel Prealbumin Plasma ferritin or transferrin Amylase and Lipase Consider essential fatty acid panel The Mountain States Genetics Regional Collaborative Center (MSGRCC) is supported by cooperative agreement #U22MC10761 with the United States Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau, Genetic Services Branch. Maple Syrup Urine Disease Care Plan (last updated 2/21/09) Performance Measures 1. Age of diagnosis (both positive NBS and confirmatory SAA) 2. Presence of illness at time of diagnosis. 3. Days until Leucine is within treatment range (<500µmol/L) 4. Therapy during initial care a. Enteral MSD formula vs. dialysis b. Track edema, Leu level (>600 µmol/L), use of dialysis, +/-mannitol, coma score, and osmolarity 5. Initial lab studies a. NBS result b. Quant plasma amino acids c. UOA d. Metabolic panel e. Osmolarity studies f. Enzymatic results g. Molecular results 6. Monitoring lab studies a. Quantitative plasma amino acids b. Basic metabolic panel c. Osmolarity d. Amylase and lipase e. Nutrition labs 7. Frequency of clinic contacts and visits (track compliance with visits) 8. Total decompensations and hospitalizations. a. Track ICU admissions b. # of days of hospitalization c. # of ER visits d. Track edema, Leu level (>600 µmol/L), Isoleucine (>100µmol/L ), valine (>100µmol/L ), use of dialysis, +/-mannitol, coma score, and osmolarity e. Lab studies 9. Number of pancreatitis episodes 10. DEXA results and number of fractures 11. Growth parameters (ht, wt, OFC, BMI) 12. Type of MSUD a. Classic, Intermediate, Intermittent, Thiamine responsive, or Lipoamide dehydrogenase (E3) deficiency 13. Diet a. Frequency of Metabolic dietitian visits b. Frequency of dietary analysis (3 day diet records) c. Natural protein intake (tolerance) d. Formula (Y/N) e. Medical foods (Y/N) f. Mode (oral, G-tube, bolus/drip, meds only/meds and diet) 14. Transplant (Y/ N) 15. Neuropsychological evaluation results 16. Developmental services (PT, OT, & speech) 17. School performance a. Grade appropriate (Y/N) b. Special services (Y/N) c. IEP (Y/N) 18. Genetic Counseling (Y/N) Outcome measures 1. Mortality 2. Development a. IQ b. Level of functioning c. Decline in IQ or level of function 3. History and/or presence of pancreatitis 4. History and/or presence of ADHD and use of medication 5. History and/or presence of psychiatric issues (generalized anxiety, panic, and/or depression) 6. History and/or presence of osteopenia 7. History and/or presence of abnormal MRI findings 8. Outcome of liver transplantation 9. Growth a. Final adult parameters The Mountain States Genetics Regional Collaborative Center (MSGRCC) is supported by cooperative agreement #U22MC10761 with the United States Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau, Genetic Services Branch.