Pediatric Palliative Care Consultant
advertisement

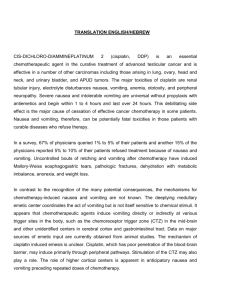
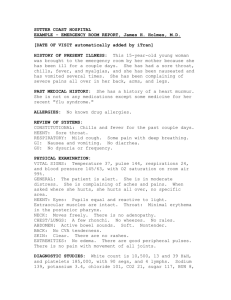
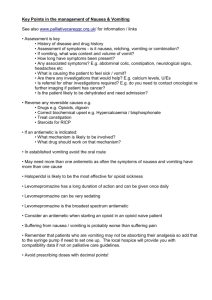
Pediatric Palliative Care Consultant Table of Contents II. E Introduction & Acknowledgments Pediatric hospice and palliative care standards Models of palliative care Disease trajectory Medical abbreviations Medication Therapy Management Services (MTMS) in hospice and palliative care Interdisciplinary team Ethical and legal considerations in pediatric hospice Communicating with pediatric patients and their families Barriers to pediatric hospice Medication administration in pediatric patients Compounded medications in palliative care M PL Introduction Guidelines for Effective Management of Symptoms (PediGEMS™) Agitation & Delirium Anorexia & Cachexia Anxiety Bleeding Bowel obstruction Congestion Constipation Cough Depression Diarrhea Dypepsia, GERD & Gastritis Dysphagia Dyspnea Edema & Ascites Fatigue/Somnolence SA I. Fever Hiccups Infections Insomnia Mucositis Muscle spasms Nausea & Vomiting Pain Pruritus Secretions Sedation Seizures Spasticity Urinary retention Xerostomia DISCLAIMER: All clinical recommendations contained herein are intended to assist with determining the appropriate medical therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patient’s attending physicians. Nothing in this document shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Use of product brand names are intended to assist the clinician in identifying products and does not connote endorsement or promotion of any kind. No financial support for the development of this book was provided by any product vendor or manufacturer. © 2013, HospiScript Services, a Catamaran Company IV. Pediatric cardiovascular disease Cystic Fibrosis HIV/AIDS Neurodegenerative & neurodevelopmental disorders (including Cerebral Palsy) Palliative chemotherapy & radiation E III. Common Pediatric Diseases Neonatal Management Appendices Normal pediatric lab values Immunization guide Extrapyramidal symptoms (EPS) from medications Medications associated with anticholinergic side effects Drugs that prolong the QT interval or induce Torsades de Pointes Medications that may increase risk of falls Look‐alike and sound‐alike drug names Method of dosage adjustment in renal failure Drugs affected by cytochrome P450 enzyme metabolism Glucocorticoid equivalency table Benzodiazepine equivalency table Insulin comparison chart Recommended starting doses in children and adults less than 50 kg body weight Pediatric recommended maximum dosing Subcutaneous administration of medications butterfly procedure Medication compatibility with feeds Drug information table SA V. M PL DISCLAIMER: All clinical recommendations contained herein are intended to assist with determining the appropriate medical therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patient’s attending physicians. Nothing in this document shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Use of product brand names are intended to assist the clinician in identifying products and does not connote endorsement or promotion of any kind. No financial support for the development of this book was provided by any product vendor or manufacturer. © 2013, HospiScript Services, a Catamaran Company PediGEMS – Nausea & Vomiting Introduction and Background1‐6 E Nausea is an unpleasant feeling of needing to vomit often accompanied by autonomic symptoms of pallor, cold sweats, salivation, tachycardia and diarrhea. Nausea can range from a mild stomach upset to complete anorexia. Retching presents as spasmodic movements of the diaphragm and abdominal muscles that may progress to vomiting. Vomiting is a complex process of involuntary spasms resulting in the reflux of gastric contents through the mouth. Chronic nausea can be defined as lasting longer than a week without a well‐defined or self‐limiting cause such as chemotherapy, radiation or infection. Children are at a higher risk of developing consequences of prolonged nausea/vomiting (i.e. dehydration, electrolyte disturbances, etc.). Recognize and correct consequences as appropriate. The GI tract and brain are the two organ systems involved with nausea and vomiting. In these two systems, the primary neurotransmitters that mediate these systems include dopamine, histamine, acetylcholine, and serotonin. The pathophysiology of nausea and vomiting is complex. The vomiting center located in the brain receives input from various areas within the brain as well as from the gastrointestinal tract. The cause of nausea and vomiting might be multifactorial. The figure below indicates the four major mechanisms for stimulation of the vomiting center (Figure 1). M PL Figure 1. Mechanisms Involved in Nausea and Vomiting Chemoreceptor Trigger Zone (CTZ) Dopamine, 5‐HT, Neurokinin‐1 Cerebral Cortex Dopamine, 5‐HT, Neurokinin‐1 Gastrointestinal Tract (GI) Dopamine, 5‐HT Vomiting Center Acetylcholine, Histamine Vestibular Nerve Cranial Nerve VIII Nausea & Vomiting SA Prevalence6 Studies suggest 40‐ 63% of children receiving palliative care will suffer from nausea and/or vomiting. Causes1‐2,7 Major causes of chronic nausea include: o Anxiety o Autonomic dysfunction o Bowel obstruction o Constipation o Gastrostasis o Infections o Increased intracranial pressure © 2013, HospiScript Services, a Catamaran Company o o o o Medications Antibiotics Nonsteroidal anti‐inflammatory drugs (NSAIDs) Chemotherapy/Radiation Opioids Overdoses/Withdrawals Metabolic disorders (ie. Hypercalcemia, renal failure) Pain Reflux PediGEMS – Nausea & Vomiting Assessment Figure 2. BARF Nausea Scale8 SA M PL E Onset o Timing, acute, anticipatory, delayed Duration o Prolonged vomiting in children is defined as > 12 hours in a neonate, > 24 hours in children younger than 2 years of age, or > 48 hours in older children. Severity8‐9 o Baxter Retching Faces (BARF) Scale (Figure 2)8 Pediatric nausea assessment scale with preliminary validation in patients aged 7 to 18 Can assist clinicians in identifying a need for or assessing effectiveness of nausea treatment Prompt questions to consider: 1. “Have you ever felt bad enough that what you ate came back out of your mouth? 2. “What do you call it when that happens?” 3. “What do you call the feeling when you feel like you might ____(use patient’s answer to question 2)?” We call this feeling nausea. 4. “These faces show children who feel no “nausea” (use patient’s answer to question 3), who feel a little bit of “nausea”, who feel even more “nauseated”, and these are children who have the most “nausea” it is possible to feel.” [Point to each corresponding face.] “Which face is more like you feel right now?” Table 1. Patient Evaluation to Determine Potential Etiologies1‐5,10‐12 History Onset of symptoms Abrupt Insidious Pattern Large, infrequent vomitus that relieves nausea Small‐volume emesis Projectile Effortless, regurgitation © 2013, HospiScript Services, a Catamaran Company Possible Causes Cholecystitis, food poisoning, gastroenteritis, pancreatitis, medications Reflux, gastroparesis, medications, metabolic disorders, pregnancy Complete or partial bowel obstruction Gastric stasis Pyloric stenosis Reflux, rumination syndrome PediGEMS – Nausea & Vomiting Table 1. Patient Evaluation to Determine Potential Etiologies, continued1‐5,10‐12 E Possible Causes Increased intracranial pressure, pregnancy, uremia Pyloric stenosis, peptic ulcer disease, psychiatric causes Dyspepsia, peptic ulcer disease, neoplasms, gastroparesis Conversion disorder, depression Achalasia, esophageal disorders Gastric outlet obstruction, gastroparesis Proximal small bowel obstruction Fistula, obstruction Organic cause GI bleed, ulcer, gastritis Upper respiratory infection, allergies, reflux Gallbladder disease, liver disease Dyspepsia, pancreatic disease, peptic ulcer disease Appendicitis Biliary disease, pancreatic disease, peritoneal irritation, small bowel obstruction Small bowel obstruction Malignancy, gastric outlet obstructions, peptic ulcer disease Viral Increased intracranial pressure, encephalitis/meningitis, head injury, mass, migraine Gastroparesis Cyclic vomiting syndrome Vestibular dysfunction Increased intracranial pressure Hyperglycemia or hypercalcemia Uremia, hyponatremia, or increased intracranial pressure Autonomic insufficiency Constipation Anxiety Evaluate location and size Bowel obstruction, ileus, or constipation Bulimia Kernicterus, liver failure, UTI (neonate) Signs of dehydration Increased intracranial pressure Constipation SA M PL History Timing of symptoms Before breakfast During or directly after eating 1‐4 hr after meal Continuous Nature of vomited matter Undigested food Partially digested food Bile Feculent or odorous Large Volume Coffee‐ground or bright red blood Mucus Abdominal pain Right upper quadrant Epigastric Right lower quadrant Severe pain Severe pain that proceeds vomiting Associated symptoms Weight loss Diarrhea, myalgias, malaise, headache Headache, stiff neck, vertigo, focal neurologic deficits Early satiety, postprandial bloating, abdominal discomfort Repetitive migraine headaches or symptoms of irritable bowel syndrome Vertigo and symptoms associated with movement Morning symptoms with morning headache and neurological symptoms Polyuria, polydipsia Altered mental status Syncope episodes, early satiety Decreased frequency of bowel movements, abdominal fullness, hard stools, straining Worry, emotional responses Physical Exam Masses Bowel Sounds and abdominal distention Calluses on dorsal surfaces of hands Jaundice Poor skin turgor, delayed capillary refill, tachycardia, hypotension Papilledema, neurological signs Fecal impaction, rectal examination © 2013, HospiScript Services, a Catamaran Company PediGEMS – Nausea & Vomiting Hydrocephalus Mass lesion Meningitis/encephalitis Subdural hematoma Kernicterus Inborn errors of metabolism Infection Urinary tract infection (UTI) Sepsis Medications Milk allergy Urea cycle defects GI Tract Excessive feeding volume Gastroesophageal reflux Hepatobiliary disease Necrotizing enterocolitis (NEC) Obstruction Esophageal stenosis Hirschsprung’s disease Incarcerated hernia Intestinal stenosis Meconium ileus Pyloric stenosis Tracheoesophageal fistula Volvulus Paralytic ileus Peritonitis Thrush Congenital adrenal hyperplasia Infection Otitis media Pneumonia Pertussis Sepsis Urinary tract infection (UTI) Ingestion accidents Medications Celiac disease Cholecystitis Constipation Eosinophillic esophagitis Gastroenteritis Gastroesophageal reflux Hepatobiliary disease Obstruction Foreign bodies Incarcerated hernia Intussusception Meckel’s Diverticulum Pyloric stenosis Volvulus Thrush Adolescents Abdominal migraine Cyclic vomiting Fear/anxiety Increased intracranial pressure Head injury Mass lesion Meningitis/encephalitis Abdominal migraine Adolescent rumination syndrome Cyclic vomiting Fear/anxiety Increased intracranial pressure Head injury Mass lesion Meningitis/encephalitis Migraines Pseudotumor cerebri Psychogenic vomiting Diabetic ketoacidosis (DKA) Infection Pharyngitis Pneumonia Sepsis Ingestions Medications Pregnancy Adrenal crisis Diabetic ketoacidosis (DKA) Infection Otitis media Pharyngitis Pneumonia Sepsis Urinary tract infections (UTI) Ingestion accidents Medications Appendicitis Celiac disease Cholecystitis Constipation Dyspepsia Eosinophilic esophagitis Gastroenteritis Gastroesophageal reflux Gastroparesis Hepatitis Inflammatory bowel disease Obstruction Foreign bodies Incarcerated hernia Intussusception Meckel’s diverticulum Volvulus Pancreatitis Peptic ulcer Peritonitis Motion sickness SA M PL CTZ Hydrocephalus Mass lesion Meningitis/encephalitis Children E Table 2. Age‐Dependent Possible Etiologies of Vomiting3‐4,13 Neonates Infants Increased intracranial pressure Increased intracranial pressure Cerebral Cortex Vestibular Nerve © 2013, HospiScript Services, a Catamaran Company Appendicitis Cholecystitis Constipation Dyspepsia Gastroenteritis Gastroesophageal reflux Gastroparesis Hepatitis Inflammatory bowel disease Obstruction Incarcerated hernia Meckel’s diverticulum Volvulus Pancreatitis Peptic ulcer disease Peritonitis Motion sickness PediGEMS – Nausea & Vomiting Clinical Characteristics1‐6 E Chemoreceptor trigger zone (CTZ) is located in the area postrema of the medulla. Nausea and vomiting are stimulated here by chemotherapeutic agents, bacterial toxins, metabolic products (ie. uremia) and opioids. Dopamine (D2), serotonin (5‐HT) and neurokinin‐1 are the primary neurotransmitters involved in this process. Therapy is based on blocking D2 with dopamine antagonists including butyrophenones (ie. haloperidol), phenothiazines (ie. chlorpromazine, prochlorperazine, promethazine) and metoclopramide. 5‐HT3 antagonists (ie. ondansetron), also active here, are mainly used for chemotherapy and radiotherapy‐induced nausea. 5‐ HT3 antagonists also have a multitude of safety and efficacy data in pediatric patients of all ages, with less incidence of side effects seen with other classes. Cerebral Cortex induced nausea and vomiting can be caused by anxiety, taste, and smell, as well as increased intracranial pressure (ICP). Corticosteroids are useful to decrease intracranial pressure, while anxiolytics, such as benzodiazepines, are used to treat “anticipatory” nausea, as well as gustatory and olfactory stimulation. Vestibular nausea and vomiting is triggered by motion. Opioids can sensitize the vestibular center, resulting in movement‐induced nausea. Ambulatory patients are more susceptible to vestibular nausea and vomiting than bedbound patients. Since histamine (H1) and acetylcholine (ACh) are the predominate neurotransmitters, antihistamines (ie. diphenhydramine) and anticholinergics (ie. glycopyrrolate, hyoscyamine) are the drugs of choice in movement‐induced nausea and vomiting. Gastrointestinal (GI) tract stimulation occurs through vagal and sympathetic pathways. These pathways can be triggered by stimulation of either mechanoreceptors or chemoreceptors located in the gut. Gastric stasis, gastrointestinal obstruction, medications, metastatic disease, bacterial toxins, chemotherapeutic agents, and irradiation, can lead to nausea and vomiting. Glossopharryngeal or vagus nerve stimulation in the pharynx by sputum, mucosal lesions or infection can also evoke nausea. The major neurotransmitters in the upper GI tract are D2, acetylcholine and 5‐HT. Metoclopramide blocks 5‐HT4 and increases gastric motility above the jejunum, whereas anticholinergics will decrease GI spasticity and motility in nausea induced by gut hyperactivity. In high doses, metoclopramide will also act as a D2 antagonist. Autonomic failure causes gastroparesis resulting in anorexia, nausea, early satiety and constipation. Delayed gastric emptying is frequently observed in patients with diabetes mellitus, chronic renal failure and neurological disorders. Malnutrition, cachexia, lung and pancreatic cancers, human immunodeficiency virus, radiotherapy, and drugs such as opioids, anticholinergics, antidepressants and vasodilators have been associated with autonomic failure and resulting chronic nausea, poor performance, tachycardia and malnutrition. Non‐pharmacologic Treatment1‐2,5‐6,10 Acupressure or acupuncture Avoid strong odors, foods, or other triggers o Try pleasant masking aromas of the child’s choosing Eliminate offending medications if possible Play/distraction: music, games, storytelling, art projects, television Promote good oral care Offer clear liquids o Sip liquids slowly Sipping off a spoon may prevent gulping Provision of small, frequent meals chosen by the child o Cold foods may be better tolerated o Promote bland foods: mashed potatoes, apple sauce, sherbert, crackers, toast o Avoid greasy, fried or spicy foods Relaxation techniques o Younger children may need a parent to cue them and help with guided imagery and stories o Older children can be taught self‐hypnosis Oral Rehydration Therapy (ORT) if prolonged vomiting (see Diarrhea PediGEMS) SA M PL © 2013, HospiScript Services, a Catamaran Company PediGEMS – Nausea & Vomiting Pharmacotherapy6 Age of the patient, combined with the clinical features of nausea and vomiting, should guide the choice of antiemetics used. Initial approach should be based on pathophysiology of the nausea and vomiting and mechanism of action of the agent (Table 3). Table 3. Pathophysiology Based Approach to Management of Nausea and Vomiting Receptor 5‐HT3 D2 D2 5‐HT4 ‐ ‐ GABA H1 H1 ACh Medication ondansetron (Zofran®) metoclopramide (Reglan®) haloperidol (Haldol®) metoclopramide (Reglan®) erythromycin (E‐Mycin®) dexamethasone (Decadron®) lorazepam (Ativan®) hydrOXYzine (Vistaril®) promethazine (Phenergan®) or diphenhydrAMINE (Benadryl®) glycopyrrolate (Robinul®) or hyoscamine (Levsin®) E Class 5‐HT3 antagonist Antiemetic Butyrophenones GI Prokinetic Macrolide antibiotic Cerebral Cortex: ↑ ICP Corticosteroid Cerebral Cortex: Anxiety Benzodiazepine Antihistamine Vestibular Antihistamine Anticholinergic M PL Mechanism of Nausea CTZ If initial approach is unsuccessful: o Ensure first line agent dose is optimized o Rotate to a different agent based on mechanism and/or o Substitute a phenothiazine, such as promethazine (Phenergan®), for both H1 and D2 receptor antagonism and/or o Consider adding a corticosteroid, such as dexamethasone (Decadron®) as a short‐term pulse and/or o Consider adding a low dose benzodiazepine, such as lorazepam (Ativan®) Table 4. Pharmacologic Management of Nausea and Vomiting14 Age Guide* Typical Starting Dose** Routes Pediatric Formulation Considerations Comments SA Generic Name (Brand Name) Chemoreceptor Trigger Zone Nausea haloperidol > 3 yoa 0.01‐0.1 mg/kg q8h 15 Adult: 0.5‐1 mg q12h or q4‐6h prn (Haldol®) © 2013, HospiScript Services, a Catamaran Company PO SL PR Solution: 2 mg/mL Tablets: 0.5, 1, 2, 5, 10, 20 mg Injection (lactate): 5 mg/mL Avoid contact with oral solution and skin, may cause contact dermatitis Dilute oral solution with water or acidic beverage IV formulation not approved in children Injection contains benzyl alcohol Protect all dosage forms from light Butyrophenone; potent D2 antagonist Useful in phenothiazine intolerance EPS more common in younger patients, but rare in low doses Less sedating than other anti‐emetics Lowers seizure threshold PediGEMS – Nausea & Vomiting Routes Pediatric Formulation Considerations Comments PO PR IM IV Solution: 5 mg/5 mL Tablets: 5, 10 mg Tablets,ODT: 5, 10 mg (no generic) Injection: 5 mg/mL Some products contain sodium benzoate > 1 month M PL ondansetron (Zofran®)16 0.1‐0.15 mg/kg q6‐8h Max: 4‐8 mg/dose Adult: 4 mg May dose 0.45 mg/kg 30 minutes prior to emetogenic chemo chlorproMAZINE (Thorazine®) prochlorperazine (Compazine®) PO SL IV Solution: 4 mg/5 mL Tablets: 4, 8 mg Tablets, ODT: 4, 8 mg Film, soluble: 4, 8 mg (not generic) Injection: 2 mg/mL Infusion, premixed in D5W or NS: 32 mg/50 mL Oral solution contains sodium benzoate Disintegrating tablets contain phenylalanine PO PR IM Syrup: 6.25 mg/5 mL Tablets: 12.5, 25, 50 mg Injection: 25, 50 mg/mL Suppositories: 12.5 mg, 25 mg, 50 mg Do not give IV or SQ SA Chemoreceptor Trigger Zone Nausea: Phenothiazines promethazine > 2 yoa 0.25‐1 mg/kg q4‐6h prn (Phenergan®) Max: 25 mg/dose Adult: 12.5‐50 mg ≥ 6 months 0.5‐1 mg/kg q4‐6h Max Dosing: <5 yoa: 40 mg/day 5‐12 yoa: 75 mg/day Adult: 10‐25 mg PO SL PR IM IV > 2 yoa PO, PR: 0.1 mg/kg q6‐8h Adult: 10 mg PO q4‐6h prn, 25 mg PR q6‐12h prn IM, IV: 0.1‐0.15 mg/kg q8‐12h, NTE 40 mg/day Adult: 5‐10 mg PO PR IM IV © 2013, HospiScript Services, a Catamaran Company D2 ‐ receptor antagonist, especially at higher doses 5‐HT4 agonist activity in the gut Prokinetic: useful if gastric stasis also present EPS more common in children. May administer diphenhydrAMINE for EPS prevention. Concurrent administration with antimuscarinic agents (ie. diphenhydrAMINE) will decrease prokinetic effect, but not anti‐emetic effect. Black box warning for irreversible tardive dyskinesia, especially at higher doses May cause sedation and confusion Contraindicated in complete bowel obstruction 5‐HT3 receptor antagonist SE minimal: headache, constipation May induce nausea at high doses E Generic Name Age Typical Starting Dose** (Brand Name) Guide* Chemoreceptor Trigger Zone Nausea, continued metoclopramide 0.1‐0.2 mg/kg q 6h Adult: 10 mg (Reglan®) Up to 1 mg/kg for dopamine antagonism or chemotherapy induced Administer 30 min before meals and at bedtime Tablets: 10, 25, 50, 100, 200 mg Injection: 25 mg/mL Tablets contain benzoic acid For direct IV injection, dilute with NS to max concentration: 1 mg/mL & infuse at rate NTE 0.5 mg/minute Do not administer SQ (tissue damage) Tablets: 5, 10 mg Injection: 5 mg/mL Suppositories: 25 mg Injection contains benzyl alcohol Do not administer SQ (tissue damage) Black box warning in <2 yoa due to risk of fatal respiratory depression Avoid IV administration ‐risk of extravasation May lower seizure threshold Anticholinergic side effects, including significant sedation May cause EPS Extrapyramidal symptoms (EPS) common in pediatric patients Sedating May lower seizure threshold Dosage adjustment in hepatic impairment More frequent dosing with PO Use with caution in chronic respiratory diseases May lower seizure threshold High incidence of EPS in children Reserve use in children <5 yoa to those who are unresponsive to other antiemetics Sedating PediGEMS – Nausea & Vomiting Generic Name Age (Brand Name) Guide* Gastric Stasis Nausea metoclopramide (Reglan®) Typical Starting Dose** Routes Pediatric Formulation Considerations Comments 0.1‐0.2 mg/kg q 6h Adult: 10 mg May dose up to 1 mg/kg for dopamine antagonism or chemotherapy induced nausea/vomiting Administer 30 min before meals and at bedtime PO PR IM IV Erythromycin (E‐ Mycin®) 2.5 mg/kg q6h Administer before meals and at hs Adult: 125‐250 mg D2 ‐ receptor antagonist, especially at higher doses 5‐HT4 agonist action in the gut EPS may occur more frequently in children. May administer diphenhydrAMINE for EPS prevention. Concurrent administration with antimuscarinic agents (ie. diphenhydrAMINE) will decrease prokinetic effect, but not anti‐emetic effect. Black box warning for irreversible tardive dyskinesia May cause sedation and confusion Contraindicated in complete bowel obstruction Consider if patient’s cannot tolerate metoclopramide (due to EPS) E M PL PO Suspension: 200 mg/5 mL Capsules, Tablets: 250 mg Chewable tablets should not be swallowed whole Delayed release and enteric coated tablets should not be broken or chewed Avoid IV administration, associated with fatal complications, contains benzyl alcohol Vestibular Nausea: Antihistamines promethazine > 2 yoa 0.25‐1 mg/kg q4‐6h prn (Phenergan®) Max: 25 mg/dose Adult: 12.5‐50 mg PO PR IM Syrup: 6.25 mg/5 mL Tablets: 12.5, 25, 50 mg Injection: 25, 50 mg/mL Suppositories: 12.5 mg, 25 mg, 50 mg Do not give IV or SQ dimenhyDRINATE (Dramamine®) PO IM Tablet: 50 mg Tablet, chewable: 25, 50 mg Injection: 50 mg/mL Injectable solution contains benzyl alcohol IV route not recommended in children Chewable tablet contains phenylalanine Elixir, Liquid, Solution, Syrup: 12.5 mg/5 mL Caplet, Capsule, Tablet: 25, 50 mg Strip, Tablet, ODT: 12.5, 25 mg (not generic) Injection: 50 mg/mL IV: Dilute to 25 mg/mL, infuse over 10‐15 min > 2 yoa 1.25 mg/kg q6‐8h Max Dosing: 2‐5 yoa: 75 mg/day 6‐12 yoa: 150 mg/day Adult: 50‐100 mg Adult Max: 400 mg/day 0.5‐1 mg/kg q4‐6h Max: 50 mg/dose Adult: 25‐ 50 mg Alt dosing regimen: 2‐5 yoa: 6.25 mg q4‐6h Max: 37.5 mg/day 6‐11 yoa: 12.5‐25 mg q4‐6h Max: 150 mg/day >12 yoa: 25‐50 mg q4‐6h Max: 300 mg/day SA diphenhydrAMINE (Benadryl®) Solution: 5 mg/5 mL Tablets: 5, 10 mg Tablets, ODT: 5, 10 mg (no generic) Injection: 5 mg/mL Some products contain sodium benzoate > 2 yoa © 2013, HospiScript Services, a Catamaran Company PO PR IM IV Black box warning in <2 yoa due to risk of fatal respiratory depression Avoid IV administration ‐risk of extravasation May lower seizure threshold Anticholinergic side effects, including significant sedation May cause EPS May produce excitation in young children Anticholinergic side effects including constipation, sedation May cause paradoxical excitation Serious adverse reactions have been reported in <2 yoa Anticholinergic side effects, including sedation PediGEMS – Nausea & Vomiting Routes Pediatric Formulation Considerations Comments PO IM Antihistamines not recommended in <2 yoa Very sedating Atarax® (hydroxyzine HCL) and Vistaril® (hydroxyzine pamoate) are different salt forms of same active drug meclizine >12 yoa 12.5‐ 25 mg q8h (Antivert®) Vestibular Nausea: Anticholinergics glycopyrrolate PO: 40‐100 mcg/kg q6‐8h (Robinul®) Adult: 1‐2 mg IM, IV: 4‐10 mcg/kg q3‐4h Adult: 0.2 mg PO Solution : 10 mg/5 mL (Atarax®), 25 mg/5 mL (Vistaril®) Tablets: 10, 25, 50 mg Capsules: 25, 50, 100 mg Injection: 25, 50 mg/mL IM painful; IV not recommended Injection contains benzyl alcohol Tablets: 12.5, 25 mg Tablet, chewable: 25 mg dicyclomine (Bentyl®) > 6 months 6 mon ‐ 2 yoa: 5 mg q6‐8h > 2 yoa: 10 mg q6‐8h Adults: 20 mg q6‐8h PO IV Solution: 1 mg/5 mL (not generic) Tablets: 1, 2 mg Injection: 0.2 mg/mL Administer solution on empty stomach Oral solution contains propylene glycol Compounding recipes available using tablets Injection contains benzyl alcohol Syrup: 10 mg/5 mL (not generic) Capsule: 10 mg Tablet: 20 mg Injection: 10 mg/mL hyoscyamine (Levsin®) Infants ‐ 2 yoa: PO SL Paradoxical excitation may occur in infants and young children. Infants, patients with Down’s syndrome, and children with spastic paralysis or brain damage may be hypersensitive to antimuscarinic effects Least likely to cross blood‐brain barrier, therefore it causes less confusion and visual disturbances Contraindicated in <6 mon due to serious adverse effects Caution in children with Down’s syndrome, spastic paralysis or brain damage due to increased sensitivity to toxic effects. Maintain good oral hygiene M PL Dose (drops) 5 6 8 Max Daily Dose (Drops) 30 36 48 2 ‐ 12 yoa: 0.0625‐0.125 mg q4h prn Max: 0.75 mg/day >12 yoa 0.125‐0.25 mg q4h prn Max: 1.5 mg/day 1 patch q3days Adult: 1‐3 patches SA scopolamine (Transderm Scōp®) Weight (kg) 5 7 10 PO IM IV > 12 yoa E Generic Name Age Typical Starting Dose** (Brand Name) Guide* Vestibular Nausea: Antihistamines, continued hydrOXYzine 0.5‐1 mg/kg q6h (Atarax®, Vistaril®) Adult: 10‐25 mg © 2013, HospiScript Services, a Catamaran Company TD Elixir: 0.125 mg/5 mL Solution (drops): 0.125 mg/mL Tablets, ODT, SL: 0.125 mg (no generic) Tablets: 0.125 mg Injection: 0.5 mg/mL Liquid may contain sodium benzoate or ethanol Disintegrating tablets contain aspartame IV not approved in children Transdermal Patch: 1.5 mg (not generic) Apply patch to hairless area behind one ear Do not cut patch Sedating Stronger anticholinergic effects than dimenhydrinate Sedating and constipating May cause confusion and visual disturbances May be useful in post operative nausea & vomiting PediGEMS – Nausea & Vomiting Routes Pediatric Formulation Considerations Comments PO SL PR IV Paradoxical reactions more common in children Indirect anti‐emetic effect; treats underlying anxiety that exacerbates nausea and vomiting hydrOXYzine (Atarax®, Vistaril®) PO IM Solution: 2 mg/mL Tablets: 0.5, 1, 2 mg Injection: 2, 4 mg/mL IV and oral solutions contain benzyl alcohol, polyethylene and propylene glycol Tablets can be crushed Oral suspension can be made from tablets IV: dilute with equal volume; IVP over 2‐5 min IV form may be given rectally Solution : 10 mg/5 mL (Atarax®), 25 mg/5 mL (Vistaril®) Tablets: 10, 25, 50 mg Capsules: 25, 50, 100 mg Injection: 25, 50 mg/mL IM painful; IV not recommended Injection contains benzyl alcohol Solution, Elixir: 0.5 mg/5 mL (5% EtOH) Solution, concentrate: 0.5 mg/0.5 mL (30% EtOH) Oral solutions and elixirs should be avoided in pediatric patients, as they may contain alcohol, propylene glycol, and benzoic acid. May use IV formulation orally (10 mg/mL PF) Tablets: 0.5, 0.75, 1, 1.5, 2, 4 mg Injection: 10, 25, 50 mg/mL Minimal mineral corticoid activity May have benefit in non‐specific nausea & vomiting For short term use unless terminal condition Withdraw gradually after long‐term therapy 0.5‐1mg/kg q6h Adult: 10‐25 mg M PL E Generic Name Age Typical Starting Dose** (Brand Name) Guide* Cerebral Cortex Nausea‐ Anxiety: Anxiolytics lorazepam 0.02‐0.05 mg/kg q6h prn (Ativan®) Max: 2 mg/dose Adult: 0.5‐1 mg Cerebral Cortex Nausea‐ Increased Intracranial Pressure: Corticosteroids dexamethasone 10 mg/m2, then 5 mg/m2 q6h prn (Decadron®) Alt dosing prior to chemo 0.3 mg/kg Max: 20 mg/day Adult: 4 mg PO SL PR IM IV Very sedating Atarax® (hydroxyzine HCL) and Vistaril® (hydroxyzine pamoate) are different salt forms of same active drug SA *Use cautiously in patients outside of recommended age parameters. **Do not exceed usual maximum adult starting doses. Not intended for use in neonatal population. © 2013, HospiScript Services, a Catamaran Company PediGEMS – Nausea & Vomiting Clinical Pearls SA E Recognize and correct consequences of prolonged vomiting (ie. dehydration, electrolyte disturbances, etc) as appropriate for patient goals, as these may occur quickly in children. Potentially reversible causes of nausea and vomiting should not be overlooked (ie. anxiety, constipation, gastro‐esophageal reflux (GER), medications, pain, peptic ulcer disease, bowel obstruction). Treat according to symptom specific PediGEMS. Initial therapy should be targeted towards the proposed etiology and patient’s age. Refractory cases of nausea and vomiting often require judiciously selected combinations of medications from different classes. Short courses of corticosteroids may have a role in non‐specific nausea and vomiting in addition to their usefulness in reducing intracranial pressure. The mechanism of this action is unknown.17 Risks and benefits should be weighed for long‐term use in pediatric palliative medicine. Children tend to exhibit more extrapyramidal side effects from phenothiazines (ie. chlorpromazine, prochlorperazine, promethazine), especially when given during acute viral illnesses.18 Promethazine has activity similar to antihistamines and therefore may be the best option in this class, although it does have a black box warning in those less than two years of age for fatal respiratory depression.19 DiphenhydrAMINE (Benadryl®) can be used to treat EPS from phenothiazines. Antihistamines are not approved for use in less than two years of age and should be used cautiously in those less than six years of age.20 Serotonin antagonists, while expensive, have been shown safe and effective in children of all ages, particularly postoperatively or in conjunction with chemotherapy. These agents also lack the extrapyramidal side effects seen with many other antiemetic agents.16 M PL © 2013, HospiScript Services, a Catamaran Company PediGEMS – Nausea & Vomiting References 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. E 7. 8. 9. M PL 2. 3. 4. 5. 6. Santucci G, Mack JW. Common Gastrointestinal Symptoms in Pediatric Palliative Care: Nausea, Vomiting, Constipation, Anorexia, Cachexia. Pediatr Clin N Am 2007; 54: 673‐689. Hain RDW, Jassal SS. Paediatric Palliative Medicine. New York: Oxford; c2010. Chapter 9, Nausea and Vomiting; p. 89‐103. Di Lorenzo C. Approach to the infant or child with nausea and vomiting. In:UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA 2012. Hernandez CG, Singleton JK, Aronzon DZ. Primary Care Pediatrics. Philadelphia: Lippincott; c2001. Chapter 38, Abdominal Pain, Vomiting and Diarrhea; p. 443‐467. Wood GJ, Shega JW, Lynch B, et al. Management of Intractable Nausea and Vomiting in patients at the End of Life. JAMA 2007; 298(10): 1196‐1207. Friedrichsdorf SJ, Drake R, Webster ML. Chapter 33, Gastrointestinal Symptoms. In: Wolfe J, Hinds PS, Sourkes BM, editors. Textbook of Interdisciplinary Pediatric Palliative Care. Philadelphia: Saunders; c2011. p.311‐334. Hauer J, Jones BL, Wolfe J. Pediatric Palliative Care. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA 2012. Baxter AL, Watcha MF, Baxter WV, et al. Development and validation of a pictorial nausea rating scale for children. Pediatrics 2011;127:e1542‐e1549. Dupuis LL, Taddio A, Kerr EN, et al. Development and validation of the pediatric nausea assessment tool for use in children receiving antineoplastic agents. Pharmacotherapy 2006;26:1221‐31. Wrede‐Seaman L. Pediatric Pain and Symptom Management Algorithms for Palliative Care. China: Intellicard, c2005. Nausea and Vomiting, p. 50‐53. Scorza K, Williams A, Phillips D, et al. Evaluation of Nausea and Vomiting. Am Fam Physician 2007;76(1):76‐84. Getto L, Zeserson E, Breyer M. Vomiting, Diarrhea, Constipation, and Gastroenteritis. Emerg Mede Clin N Am 2011;29:211‐37. Sreedharan R, Liacouras CA. Major Symptoms and Signs of Digestive Tract Disorders. In: Kliegman RM, Stanton BF, Gemelll JW, et al, editors. Nelson Textbook of Pediatrics, 19th ed. Philadelphia: Saunders, c2011. p. 1242‐1243. Lexi‐Comp Online, Pediatric & Neonatal Lexi‐Drugs Online, Hudson, Ohio: Lexi‐Comp, Inc; July 23, 2012. Siden HB. Haloperidol as a Palliative Anti‐Emetic in a Toddler: An Evidence Base Challenge. Journal of Pain and Symptom Management 2008; 35(3):235‐238. Culy CR, Bhana N, Plosker GL. Ondansetron: a review of its use as an antiemetic in children. Paediatr Drugs 2001; 3(6): 441‐79. Phillips RS, Gopaul S, Gibson F, et al. Antiemetic medication for prevention and treatment of chemotherapy induced nausea and vomiting in childhood. Cochrane Database Syst Rev 2010;9:CD007786. Dyer KS, Woolf AD. Use of Phenothiazines as Sedatives in Children. Drug Safety 1999;21(2):81‐90. Starke PR, Weaver J, Chowdhurry BA, et al. Boxed Warning Added to Promethazine Labeling for Pediatric Use. N Engl J Med 2005;352:2653. Harris G. FDA panel urges ban on medicine for child colds. New York Times 2007 Oct 20. SA 1. © 2013, HospiScript Services, a Catamaran Company PediGEMS – Nausea & Vomiting SA M PL E Figure 3. Nausea and Vomiting Treatment Algorithm1‐3,10 © 2013, HospiScript Services, a Catamaran Company

![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)